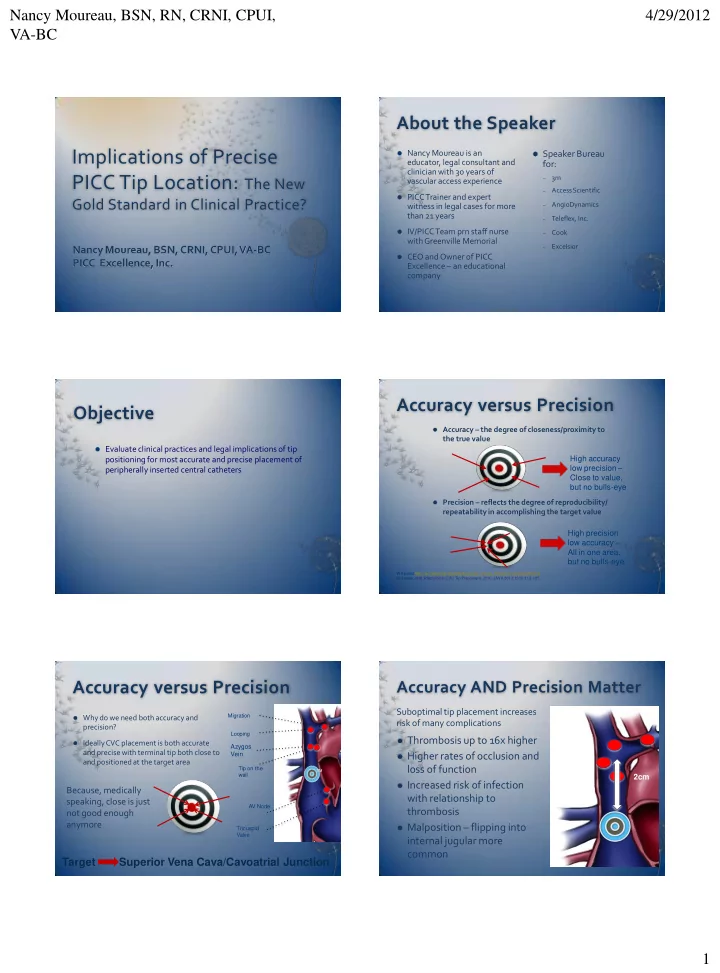
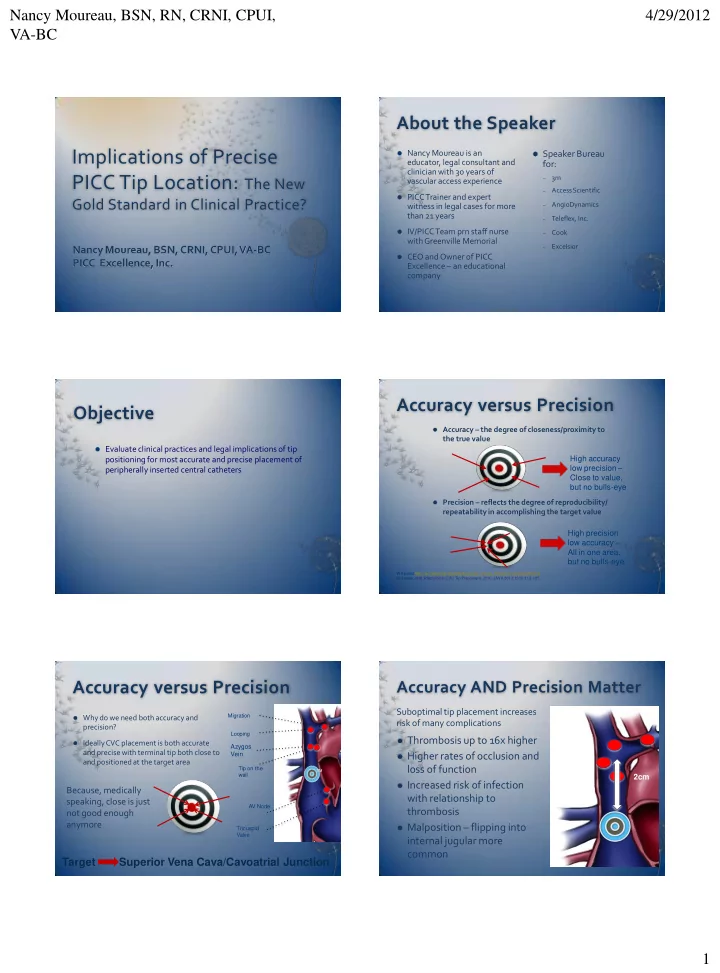
Nancy Moureau, BSN, RN, CRNI, CPUI, 4/29/2012 VA-BC About the Speaker Implications of Precise Nancy Moureau is an Speaker Bureau educator, legal consultant and for: clinician with 30 years of PICC Tip Location: The New 3m – vascular access experience Access Scientific – PICC Trainer and expert Gold Standard in Clinical Practice? AngioDynamics witness in legal cases for more – than 21 years Teleflex, Inc. – IV/PICC Team prn staff nurse Cook – with Greenville Memorial Excelsior Nancy Moureau, BSN, CRNI, CPUI, VA-BC – CEO and Owner of PICC PICC Excellence, Inc. Excellence – an educational company Accuracy versus Precision Objective Accuracy – the degree of closeness/proximity to the true value Evaluate clinical practices and legal implications of tip positioning for most accurate and precise placement of High accuracy low precision – peripherally inserted central catheters Close to value, but no bulls-eye Precision – reflects the degree of reproducibility/ repeatability in accomplishing the target value High precision low accuracy – All in one area, but no bulls-eye Wikipedia http://en.wikipedia.org/wiki/Accuracy_versus_Precision accessed 4/6/12 Hostetter, et al. Precision in CVC Tip Placement. 2010. JAVA 2010;15(3):112-125. Accuracy versus Precision Accuracy AND Precision Matter Suboptimal tip placement increases Migration Why do we need both accuracy and risk of many complications precision? Looping Thrombosis up to 16x higher Ideally CVC placement is both accurate Azygos and precise with terminal tip both close to Vein Higher rates of occlusion and and positioned at the target area loss of function Tip on the TM wall 2cm Increased risk of infection Because, medically with relationship to speaking, close is just AV Node thrombosis not good enough anymore Malposition – flipping into Tricuspid Valve internal jugular more common Target Superior Vena Cava/Cavoatrial Junction 1
Nancy Moureau, BSN, RN, CRNI, CPUI, 4/29/2012 VA-BC Goals of Terminal Tip Why is Tip Location Important? Confirmation 45.2% 87% Designed to: Verify placement in vein versus artery 19% 31% Reduce complications associated with malpositioning Reduce liability from terminal tip complications 18% 4.2% Establish catheter tip into optimal high flow area Promote patient safety 1.5% 0-2% Why Distal SVC near Cavo Atrial Junction? Established as standard by FDA CVC Working Group in 1994 5.6% 5.6% Included in instructions for use by manufacturers Reduces potential for malpractice Caers J, et al. Catheter Tip Position as a risk factor for thrombosis associated with the use of subcutaneous ports. Support Care Cancer 2005 13:325-331. Petersen et al, Silicone Venous Access Devices Positioned with Their Tips High in the Superior Vena Cava Are More Likely to Malfunction, Am J Surg 1999, 178:38-41 (Special thanks to Lorelle Wuerz) Case Study Situation - Emergency transport Background – 10 year old boy receiving long-term medications at home. MD ordered recheck of PICC placement after 4 months when pt having mild SOB. Prior Clinical Applications to X-ray pt developed acute SOB, anxiety, then cardiac arrest. Cause Catheter was positioned in right atrium – Potential for Malpractice Eroded through the heart wall – Resulted in cardiac tamponade – Action 911 – Patient died en-route to hospital – Malpractice potential, huge, which was why I was contacted. Original confirmation was deep. Solution – Accuracy and Precision the first time Pinpointing for Safety and Precision Matters – What Position for X-Ray? Reduced Liability Upper RA placement increases risk Factors Moving Tip Upward or Downwards External Landmark Without • Catheter induced Guidance Afib or V-Tach • Other RA wall 2 cm 2cm Magnetic Tip Navigation related complications • Irritation from TPN SVC and other high ECG Guidance osmotic solutions 2-4 cm creating thrombosis risk ECG with Doppler • Increased infection risk - Cavo Atrial thrombosis and Junction infection related 1. Trerotola et al. J Vasc Interv Radiol 2007; 18:513-518 2. Naylor JAVA 2007:12:1:29-31 1-2cm 3. Starr et al, Ann Surg, 1986:673-676 4. Salmela et al. Acta Anaesthesiol Scand 1993: 37:26-28 5. Hostetter, et al. Precision in CVC Tip Placement. 2010. JAVA 2010;15(3):112-125. R Atrium 2
Nancy Moureau, BSN, RN, CRNI, CPUI, 4/29/2012 VA-BC Case Study Target Area Superior Vena Cava/CAJ Situation – Friday 4pm PICC placement requiring confirmation prior to use • Cardiac Arrythmias Background – 72 yo female requires PICC for fluids, K+ and medications. Radiologist • Arterial Access leaves at 16:30, PICC nurse not authorized to read films. X-ray report dictated PICC Complications • Erosion through vein wall in the IJ • Thrombosis • Erosion through heart wall Action choices • Pulmonary Emboli • Cardiac Tamponade Remove (patient required access) – Wait for catheter to drop (no PICC nurse available S/S) – – Pull back to alternative position (K+ is an irritant) • Positioning too deep, malposition or in artery • High position of terminal tip Replace with new insertion or exchange – Cause Left sided position without making downward turn into SVC Nurse pulled catheter back – no X-ray recheck • Irritation to vein wall. Suboptimal position high in SVC, subclavian or collateral veins Response – LOC change within 24 hours, pt confused, died within 48 hours • Positioning in the right atrium or ventricle • Coagulation and thrombotic development resulting in emboli blocking pulmonary artery into lungs Cause – Arterial placement • Erosion of catheter through heart wall allowing infusion of solutions into the pericardium Potential for Malpractice – Radiologist misread film (too difficult to differentiate vein Result from artery up the neck – final report PICC in vertebral artery), Nurse did not correct • Atrial fibrillation, flutter, premature ventricular contractions , emboli, stroke or confirm the placement, cleared the line for use. Nurse suspended from work. • Infusion into pleural space. • Failure to achieve blood return Patient’s family sued, hospital settled for undisclosed amount. • Pneumonia, infiltrates, abscess • Poor function, lack of blood return, pulmonary emboli, post thrombotic Solution – Better forms of confirmation that allow location pinpoint during insertion, sequellae • Compromise of heart function, cardiac tamponade with 70% mortality and vein and artery differentiation. • Difficulty breathing, chest pain, palpitations and sudden death • Pericardial effusion results in pressure on the heart resulting in decreased cardiac function and death Measuring Liability Liability Issues Performing tip confirmation: Where is the risk? Where is the Levels of success with Landmark: 46-75% 2,3,4,5 safety? Success with Magnetic navigation: 80% 3 X-ray – The Current Standard ECG Confirmation ECG with Doppler Confirmation Success with ECG: 55-88% 6,7 • Simple chest X-ray confirmation • Greater accuracy and precision • Same advantages as with ECG • Frequently difficult to read • Requires discernible P-wave and • Indicates position or malposition interpretation with flow indicator Since SA node is located near the CAJ in the • General area validation. Placement frequently too deep or too shallow • Measures changes in P-wave once • Detects arterial flow (10-15%) reaching superior vena cava posterior wall of the right atrium, the P-wave • Combined use designed to measure • Malpositions: 5-8% in IJ, 3-5% • Requires understanding of target location and provide all clear contra- lateral or “looped back” P-wave polarization and Blue Bullseye indication acts like a beacon used to guide a catheter tip, depolarization • 1D flat film reading missing Azygos • Broad application for accuracy and and other malpositions • Unable to detect arterial placement precision with cardiac patients towards the CAJ • More than 50% need some kind of • Improved accuracy and precision • No interpretation required adjustment after first placement ECG and Doppler potential success 95% or • Failure to differentiate arterial placement greater 8 References: 2. Trerotola et al. J Vasc Interv Radiol 2007; 18:513-518 3. Naylor JAVA 2007; 12:1:29-31 4. VSN Market Research 5. Hostetter, R. et al JAVA 15:3, 114-123 6. Starr et al, Ann Surg, 1986; 673-676 7. Salmela et al. Acta Anaesthesiol Scand 1993; 37:26-28 8. Clinical data on file at VasoNova, Inc. 15 Doppler Principles for Tip Position Reducing Potential for Malpractice Diastolic Systolic How can you effectively reduce the potential for malpractice? inflow inflow By developing processes that promote consistent outcomes greater than 95% of the time SVC Pulse Doppler S Provide confirmation in timely manner with insertion while ruling D out arterial placement Put the tools in the hands of the inserter Flow in veins is pulsatile driven by heart cycle X-Ray – General location for terminal tip – Accurate most of the time – Is that good enough? hemodynamics ECG/EKG – Greater accuracy and precision, applicable to most patients A with P-wave Atrial ECG/EKG + Doppler – Achieves maximum accuracy, precision and safety, greatest application Contraction 3
Recommend
More recommend