REVIEW ARTICLE Asian Pacifjc Journal of Allergy and Immunology Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic Eakachai Prompetchara, 1,2,3 Chutitorn Ketloy, 1,2 Tanapat Palaga 4,5 Abstract As the world is witnessing the epidemic of COVID-19, a disease caused by a novel coronavirus, SARS-CoV-2, emerging genetics and clinical evidences suggest a similar path to those of SARS and MERS. Tie rapid genomic sequencing and open access data, together with advanced vaccine technology, are expected to give us more knowledge on the pathogen itself, including the host immune response as well as the plan for therapeutic vaccines in the near future. Tiis review aims to pro- vide a comparative view among SARS-CoV, MERS-CoV and the newly epidemic SARS-CoV-2, in the hope to gain a better understanding of the host-pathogen interaction, host immune responses, and the pathogen immune evasion strategies. Tiis predictive view may help in designing an immune intervention or preventive vaccine for COVID-19 in the near future. Key words: Coronavirus, immune response, COVID-19, immune evasion, immunopathology From: Corresponding author: 1 Center of Excellence in Vaccine Research and Development Tanapat Palaga (Chula Vaccine Research Center Chula VRC), Faculty of Medicine, E-mail: tanapat.p@chula.ac.th Chulalongkorn University, Bangkok 10330, Tiailand 2 Department of Laboratory Medicine, Faculty of Medicine, Chulalongkorn University, Bangkok 10330, Tiailand 3 Vaccines and Tierapeutic Proteins Research Group, the Special Task Force for Activating Research (STAR), Chulalongkorn University, Bangkok 10330, Tiailand 4 Department of Microbiology, Faculty of Science, Chulalongkorn University, Bangkok 10330, Tiailand 5 Center of Excellence in Immunology and Immune-mediated Diseases, Chulalongkorn University, Bangkok 10330, Tiailand Introduction Tie world experienced the outbreaks of coronavirus in- its likely origin, symptoms and the host immune responses to fection that threaten global pandemic in 2002-2003 by Severe combat the infection. Acute Respiratory Syndrome (SARS) and in 2011 by Middle With the rapid bedside-to-bench investigation, newly avail- East Respiratory Syndrome (MERS). In both cases, the caus- able tools such as next generation sequencing (NGS) and the ative agents (SARS-CoV and MERS-CoV, respectively) were open access information, key information on the clinical fea- newly identifjed coronavirus in the genus Betacoronavirus tures of the infected patients and the host immune responses with zoonotic origin. At the end of 2019, outbreak of another started to accumulate for reconstructing the jigsaw puzzle of coronavirus that causes respiratory-related illness was report- the epidemic piece by piece. 2 With its genome closely related ed in Wuhan, Hubei, China, a disease now offjcially called “the to SARS-CoV and MERS-CoV and the accumulated clinical Corona Virus Disease 2019; COVID-19” . Tie coronavirus that and experimental data on these previous viruses, one can hy- is the causative agent of this respiratory disease was identifjed pothesize and even predict how the host immune system may and its genome is fully sequenced. 1 Tie genomic sequence of deal with this particular virus and how the virus may evade SARS-CoV-2 showed similar, but distinct genome composition such host responses. Tiis review focuses on the immunol- of SARS-CoV and MERS-CoV. Since its fjrst reported case in ogy side of the infection using insights learned from the late 2019, the infection has spread to other regions in China outbreak of SARS-CoV and MERS-CoV. Based on the ac- and other countries, and the transmission rate, the mortality cumulated data and knowledge on the previous coronavirus rate and the clinical manifestation slowly emerged. However, infection, this review hopes to fjll the knowledge gap on hu- it will take months and maybe years until we will fully grasp man immune response to SARS-CoV-2 infection that may the whole picture of the characteristics of the pathogens and shed light on what may go wrong that leads to some fatalities. 1
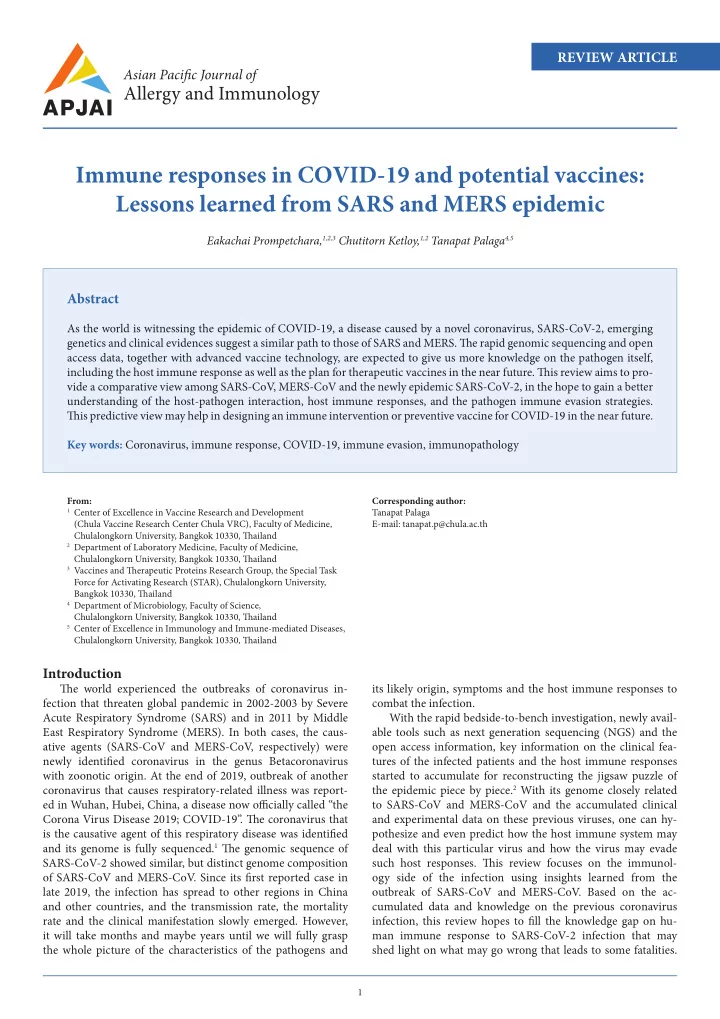
Asian Pac J Allergy Immunol 2020;38:1-9 DOI 10.12932/AP-200220-0772 Tiis insight may help in designing the appropriate immune 75,282 cases). 6 Although the fatality rate is far lower than that intervention for treatment and the prophylactic/therapeutic of SARS (9.14%) 7 and MERS (34.4%), 8 the accumulated con- vaccines against current coronavirus. fjrmed cases, within approximately 2 months afuer the out- break, markedly exceeded SARS, (8,096 cases, since 2002) Host-Pathogen Interaction: Emerging Profjles of SARS-CoV-2 and MERS (2,494 cases, since 2012), see Figure 1 . Tie high- Infection ly contagious nature of SAR-CoV-2 is probably due to the Investigation of emerging pattern or transmission charac- virus spreading via asymptomatic-infected individual which teristic of SAR-CoV-2 has surged afuer a burst of confjrmed has been reported in Germany. 9 Moreover, mathematical cases worldwide since December 2019. One of the initial re- models have estimated that the transmission that may occur ports stated that most of the laboratory-confjrmed infected during asymptomatic period of SARS-CoV and infmuenza were patients (27 out of 41 cases) had links to Wuhan seafood mar- approximately 5% and 40%, respectively. 10 Observation of 88 ket. 2 Identifjcation of the source or intermediate host of SAR- cases diagnosed during January 20-28, 2020 from individ- CoV-2 were attempted, focusing on animals normally traded uals with travel history to Wuhan, found that the mean in- within the market including snakes, birds and other small cubation period ranged from 2.1 to 11.1 days (mean = 6.4 mammals. However, to date, no specifjc animal association days), 11 which is similar to another study 5 and was in the same with SAR-CoV-2 has been conclusively identifjed. Tie most range with SARS-CoV and MERS-CoV. 11 Longer incubation likely intermediate host candidate is thought to be pangolins as periods of up to 24 days was also reported 12 but still under the coronavirus genetic sequences from the animals and from debate. WHO experts discussed during its press conference on humans infected during the outbreak showed a 99% match, February 10, 2020 that 24 days reported was either an outlier which was reported by the researchers at a press conference on observation or could possibly be due to double exposure. 13 February 7, 2020. 3 Identifjcation of SARS-CoV-2 tropism is also warranted. In parallel with intermediate host identifjcation, a study in In agreement with genome similarity with SARS, analysis of one family revealed that 6 patients who had travelled to Wu- nucleic acid sequence within the spike protein receptor-bind- han, had no direct contact with the market. Moreover, one of ing domain (RBD) has been predicted that SAR-CoV-2 might the family members became infected even without a trip to also use angiotensin-converting enzyme 2 (ACE2) as a cell Wuhan. Tie conclusion was that SAR-CoV-2 could be trans- receptor. 14 Tie study performed in vitro experiments which mitted from human-to-human, via respiratory droplets or could confjrm that SAR-CoV-2 used ACE2 for cellular entry. 15 close contact. 4 A larger study with 425 patients also confjrmed Because wild range of animal species (except rat and mouse) human-to-human transmission in which most of the patients express ACE2, it could support the observed cross-species and (200 out of 277) who were diagnosed during January 1–22, 2020, human-to-human transmission events. Demographic data and had never been exposed to either the Wuhan market or been emerging characteristic of SARS-CoV, MERS-CoV and SAR- in close contact with individuals with respiratory symptoms. 5 CoV-2 are summarized in Table 1 . According to the rapid spreading of SAR-CoV-2, WHO As SAR-CoV-2 is a novel human-infecting pathogen, re- issued a public health emergency of international concern cent studies also attempted to defjne more accurate infection (PHEIC) alarm on January 30, 2020. As of February 20, 2020, situation and to forecast the outbreak in the near future. By a total of 75,725 confjrmed cases were reported in at least 29 using a mathematical model to calculate the basic reproduc- countries worldwide with the fatality rate of 2.8% (2,126 out of tive number, R 0 , which is the average number of people that A 2,126/75,725* B 80,000 9.19% 34.4% 60,000 SARS-CoV MERS-CoV Number of cases 40,000 2.8% 20,000 744/8,096 8,000 6,000 SARS-CoV-2 858/2,494 4,000 2,000 0 SARS-CoV MERS-CoV SARS-CoV-2 Confjrmed cases Deaths Figure 1. Comparative data of (A) deaths/total cases and (B) mortality rate of SAR-CoV, MERS-CoV and SARS-CoV-2. Numbers on bar graphs represent death/confjrmed cases *Data obtained Feb 20, 2020, 9.53 am. 6 2
Recommend
More recommend