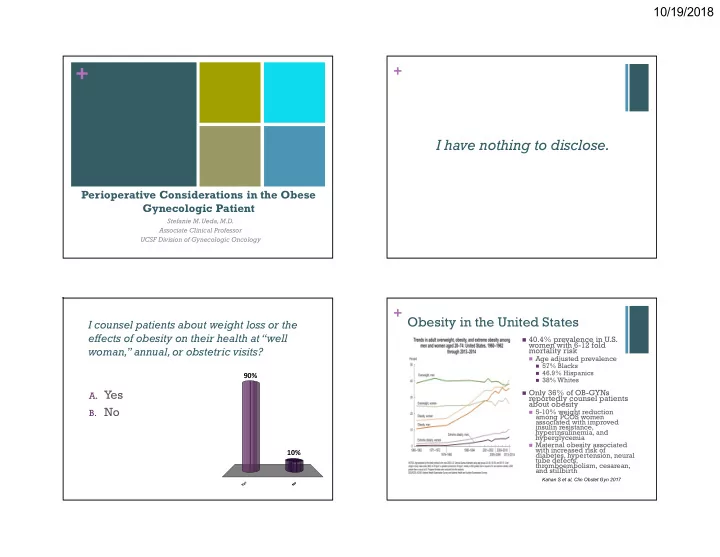
10/19/2018 + + I have nothing to disclose. Perioperative Considerations in the Obese Gynecologic Patient Stefanie M. Ueda, M.D. Associate Clinical Professor UCSF Division of Gynecologic Oncology + Obesity in the United States I counsel patients about weight loss or the effects of obesity on their health at “well 40.4% prevalence in U.S. women with 6-12 fold woman,” annual, or obstetric visits? mortality risk Age adjusted prevalence 57% Blacks 46.9% Hispanics 90% 38% Whites A. Yes Only 36% of OB-GYNs reportedly counsel patients about obesity B. No 5-10% weight reduction among PCOS women associated with improved insulin resistance, hyperinsulinemia, and hyperglycemia Maternal obesity associated with increased risk of 10% diabetes, hypertension, neural tube defects, thromboembolism, cesarean, and stillbirth Kahan S et al, Clin Obstet Gyn 2017 s o e N Y 1
10/19/2018 + + Pharmacotherapy and Surgery Weight Loss Reverses Co-Morbidities 4 FDA approved medications 1 5-10%sustained 5A’s Approach to Counseling Lorcaserin (Belviq) weight loss improves glycemic control, Phentermie-topiramate (Qsymia) triglycerides, blood Naltrexone-buproprion (Contrave) ASSESS Measure BMI pressure, LFTs,and Liraglutide (Saxenda) Identify co-morbidities chronic pain Discuss readiness for change Pharmacotherapy as adjunct to behavioral Medicare began counseling ADVISE Counseling benefits reimbursing obesity Continued long term if obtain at least 5% counseling in primary weight loss after 3 months care in 2011 AGREE Establish goals Maximum 22 visits Monitor nutrition & activity Bariatric surgery indicated in patients with (15 min) over 1 year BMI>40 or >35 with 1 comorbidity 2 contingent on ASSIST Problem solve barriers patients achieving 3 Average 2 year weight loss of 25% for Identify contributors/causes kg weight loss sleeve gastrectomy and 32% for Roux-en Y bypass ARRANGE Refer to dietitians, hospital Reducing caloric Meta-analysis shows weight loss in range based programs, behavioral intake by 500-750 of 10-15% calories/day providers 1 Kahan S et al, Clin Obstet Gyn 2017 2 Jensen MD et al, J Am Coll Cardiolo 2014 Kahan S et al, Clin Obstet Gyn 2017 + Cardiopulmonary Physiology in the Obese + Physiologic Changes of Obesity Cardiovascular Renal Increase in oxygen demand, cardiac output and stroke volume Higher inflammatory cytokines and endothelial Decrease in vascular volume increasing risk for heart failure, hypertension, dysfunction peripheral edema arrhythmia, and sudden death Gastrointestinal Respiratory Larger gastric volumes Reduced lung compliance, functional Lower gastric pH residual capacity, total lung volume, and Delayed stomach expiratory reserve emptying Increase work of breathing, oxygen consumption, and CO2 production Higher intra-abdominal pressures with increased Increase adipose deposition increases upper airway resistance risk of aspiration Higher likelihood of OSA Louie M et al, Curr Opin Obstet Gynecol 2016 Louie M et al, Curr Opin Obstet Gynecol 2016 2
10/19/2018 + Preoperative Evaluation + Pulmonary Optimization Inspiratory muscle training Exercise capacity assessment (<4 metabolic equivalents) may decrease postoperative complications 1 Preoperative EKG and CXR Possible referral to cardiology (echo and stress test) STOP-BANG serves as validated OSA screening tool 2 COPD or severe reactive airway disease Score 5-8 high risk for PFTs (FEV1/FVC<70% and FEV1>12% poorer prognosticators) moderate to severe OSA OSA testing (6.7% vs 2.6% complication rate) Higher risk for difficult intubation (20%), mask Elevated serum bicarbonate sensitive for elevated PaC02 levels ventilation (23%), and 1 year mortality (7.45%) Anesthesia evaluation CPAP and multimodal pain regimen to reduce opioids Screening for Type II DM if >45 that induce intermittent hypoxia HgbA1C (6.5-7%) 30-40º position with ISP Fasting blood sugar (<110) 1 Pouwels S et al, Resp Med 2016 2 hour postprandial (<140) 2 Nagappa M et al, Curr Opin Anesthiol 2017 Leonard KL et al, Surg Clin North Am 2015 + + Thromboembolic Prophylaxis Bowel Preparation Obese patient with at least moderate risk (3%) No routine bowel prep VTE incidence 2% and PE 0.5% Exacerbates cardiovascular and renal Intraoperative sequential compression devices recommended dysfunction Addition of heparin prophylaxis 1 2012-15 review of ACS-NSQIP in elective Cancer colorectal resections Age>40 Mechanical bowel prep alone showed no Pulmonary dysfunction significant benefit History of VTE Antibiotic bowel prep lowered Thrombophilia Surgical site infection (OR 0.63, p= 0.01) Anastomotic leak (OR 0.53, p=0.002) Systematic literature review of postoperative prophylaxis 2 Combination of mechanical and antibiotic LMWH 3000-4000 anti-Xa IU SC Q12 hours or SCDs acceptable for bowel prep reduced low risk obese patients Surgical site infection (OR 0.39, p<0.001) LMWH 4000-6000 anti-Xa IU SC Q12 hours for higher risk patients Wound dehiscence (OR 0.43, p=0.001) and consider extending for 10-15 days (age >55, BMI>50, history VTE, OSA, venous disease, pulmonary hypertension) Anastomotic leak (OR 053, P<0.001) Heterogeneous efficacy for IVC filter placement Klinger AL et al, Ann Surg 2017 1 Gould MK et al, Chest 2012 2 Venclauskas L et al, Eur J Anaesthesiol 2018 3
10/19/2018 + + Antibiotic Prophylaxis Intraoperative Positioning Higher risk for pressure Current recommendations for 3g ulcers and nerve injuries if >6-8 hours for patient >120 kg Lithotomy safe with 60 minutes prior to incision padded boot type stirrups Re-dose every 4 hours Buttocks slightly lower Pharmacokinetic study of 63 than edge of bed when shifted in Trendelenburg patients who received 2g cefazolin as surgical prophylaxis Tucking both arms with padding at elbows Fewer patients with BMI>35 achieved therapeutic levels (58% vs 75%, Bed extenders preferable p=0.20) to arm sleds Less patients with total body Anti-slide pad or bean weight>120 kg achieved therapeutic levels (55% vs 68%, p=0.28) bag with padded strap across chest BMI and TBW cut-offs poor indicators of benefit Maintaining pannus in caudad position or laterally Hites M et al, Int J Antimicrobial Agents 2016 to prevent port interference Scheib SA et al, J Minim Invasive Gynecol 2014 + + Port Placement and Insufflation Laparoscopic Entry More cephalad and lateral No entry clearly superior and placement with longer no difference in complication trocars up to 150 mm 1 rates Orogastric tube to prevent Consider reducing stomach distention insufflation pressures to 9-12 mm Hg and less Left upper quadrant entry if Trendelenburg to 30-50º to prominent pannus improve ventilation Hasson open technique requires Increased intra-abdominal pressure leads to increased more extensive dissection venous stasis, portal venous blood flow, and airway Veress needle (150 mm) entry pressure with decreased associated with higher rate of cardiac function and failed entry and preperitoneal respiratory compliance 2 insufflation 90 degree insertion relative to 1 Scheib SA et al, J Minim Invasive Gynecol 2014 abdominal wall 2 Demirel I et al, Obes Surg 2018 Scheib SA et al, J Minim Invasive Gynecol 2014 4
10/19/2018 + + Anesthetic Agents Intraoperative Ventilation Higher risk of difficult intubation Use of short acting anesthetics like (15.8% with BMI>30 compared to propofol, desflurane, and sevoflurane 5.8% in general population) 1 because of rapid elimination Awake videolaryngoscopy (up to Propofol dosed according to lean 96% success rate) body weight 25º head up induction Apneic oxygenation with nasal O2 Desflurane may reduce mean time to extubation over sevoflurane 1 PEEP with recruitment maneuvers decreases atelectasis and improves Use of succinylcholine over other PaO2/FiO2 ratio as well as lung muscle relaxants compliance No significant differences in PaO2 Increases tidal volumes or FiO2 with pressure or volume Dilates pharyngeal isthmus controlled strategies Dosed by total body weight CPAP postoperatively reduces reduces atelectasis and pneumonia Kiss T et al, Curr Opin Crit Care 2016 on Cochrane review Pouwels S et al, Resp Med 2016 + Fluid Management + Wound Closure No need to administer extra volume to obese patients Wound separation and Goal urine output 0.5-1 ml/kg/h infection rate as high as 37% Each extra liter of fluid increases risk of in gynecology patients postoperative symptoms ~16-32% No difference in wound Goal directed fluid therapy with complications in obese hemodynamic parameters decreases women undergoing cesarean Length of stay or gynecologic surgery with Incidence of respiratory failure staple or subcuticular Surgical site infection closure 1,2 Postoperative nausea and vomiting Worse cosmetic score, darker scar color, and more Dynamic indicators such as pleth skin marks with staples variability index (PVI) may be superior Overall patient satisfaction to CVP or PCWP similar 250-500 mL boluses Less fluid infusion intraoperatively 1 Zaki MN al, AJOG 2018 No difference in renal function 24-48 2 Kuroki LM et al, Obes Surg 2018 hours postoperatively Demirel I et al, Obes Surg 2018 5
Recommend
More recommend