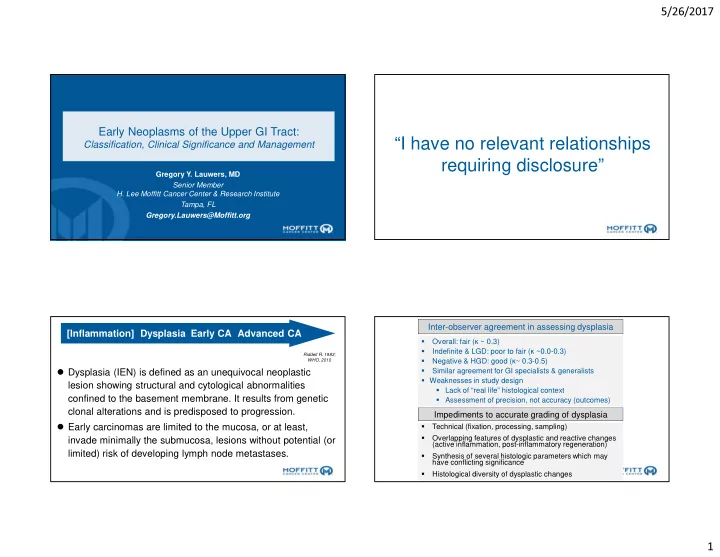
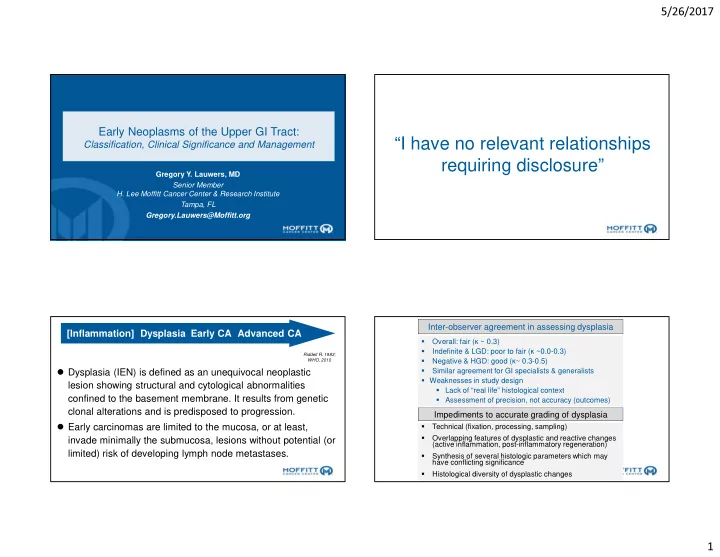
5/26/2017 Early Neoplasms of the Upper GI Tract: “I have no relevant relationships Classification, Clinical Significance and Management requiring disclosure” Gregory Y. Lauwers, MD Senior Member H. Lee Moffitt Cancer Center & Research Institute Tampa, FL Gregory.Lauwers@Moffitt.org Inter-observer agreement in assessing dysplasia [Inflammation] Dysplasia Early CA Advanced CA Overall: fair ( ĸ ~ 0.3) � Indefinite & LGD: poor to fair ( ĸ ~0.0-0.3) Riddell R. 1983; � WHO, 2010 Negative & HGD: good ( ĸ ~ 0.3-0.5) � � Dysplasia (IEN) is defined as an unequivocal neoplastic Similar agreement for GI specialists & generalists � � Weaknesses in study design lesion showing structural and cytological abnormalities � Lack of “real life” histological context confined to the basement membrane. It results from genetic � Assessment of precision, not accuracy (outcomes) clonal alterations and is predisposed to progression. Impediments to accurate grading of dysplasia � Early carcinomas are limited to the mucosa, or at least, Technical (fixation, processing, sampling) � Overlapping features of dysplastic and reactive changes invade minimally the submucosa, lesions without potential (or � (active inflammation, post-inflammatory regeneration) limited) risk of developing lymph node metastases. Synthesis of several histologic parameters which may � have conflicting significance Histological diversity of dysplastic changes � 1
5/26/2017 Esophageal carcinoma Early Neoplasms of the Upper GI Tract ADENOCARCINOMA OF THE DISTAL ESOPHAGUS • Squamous intraepithelial neoplasia [US] 5 4 • BE: classic and phenotypic variants of 3 dysplasia 2 1 0 • Gastric dysplasia and early gastric cancer Age-standardized death rates from esophagus cancer by country (per 100,000 inhabitants), WHO, 2010 Esophageal intraepithelial neoplasia Normal Regenerative epith LG- IEN HG IEN Invasive Esoph. with atypia /CIS Carcinoma Structural features Cytological features Increased cellular density Nuclear enlargement and pleomorphism Intercellular edema Nuclear overlaping Loss of differentiation/ surface Dyskeratosis normal LGIEN HGIEN CIS Invasive ca maturation Loss of cellular polarity Hyperchromasia Regular and irregular neoplastic buds Conspicuous nucleoli lamina propria lamina propria lamina propria lamina propria lamina propria • Progression: 25% & 75% of pts with LGIEN and HGIEN Sharp demarcation /Oblique line Increased and atypical mitoses develop inv. CA within10 yrs (5% for patients w/ esophagitis) Kobayashi M, et al. Oncology 2006; 71: 237-245 2
5/26/2017 Oblique line, increased cellular density, loss of polarity Diagnostic clue : oblique line Non-neoplastic Neoplastic Loss of polarity & nuclear atypia LGIEN lamina propria 3
5/26/2017 HGIEN lamina propria lamina propria CIS Carcinoma in situ Basal layer type p53 IHC & p53 mutation of esophageal Ki-67 lesions Histology IHC+ Mutation+ Mutation+/I Mutation- HC+ /IHC+ HGD/CIS 86% 71% 83% 17% LGD 81% 67% 82% 18% p53 RAE 0% 0% 0% 0% NE 0% 0% 0% 0% Proportions of (+) p53 IHC and p53 mutation show no differences between HGD/CIS & LGD 4
5/26/2017 Superficially invasive Superficially invasive Invasive CA. lamina propria Lymphatic invasion & LN metastasis in esophageal carcinoma T1a-LMP (M2) T1a-EP T1a-LPM T1a-MM SM1 SM2 SM3 (M1) (M2) (M3) (SM1) (SM2) (SM3) EP EP LPM LPM MM SM MM SM MP M1 M2 M3 SM1 SM2 SM3 Lymphatic 0% 5% 35% 54% 72% 91% permeation Lymph node 0% 0% 8% 17% 28% 49% metastasis Makutuchi H, et al. Rinsho Shoukakinaika12: 1749-1756, 1997. 5
5/26/2017 Other indication for surgery: T1a-MM (M3) Low grade IEN or � Lymphatic permeation reactive atypia? � Positive deep [vertical] margin • Enlarged nuclei • Little nuclear variety in shape • Intraepithelial lymphocytes • Limited within the lower half • No oblique line MM Re-biopsy after 4 w of PPI Basal cell Hyperplasia: proliferation > 15 % of the total thickness of epith. • High cell density, but N polarity is maintained and atypia is absent. • Reactive change reflecting disturbances in maturation of squamous epithelium. Pseudoepitheliomatous hyperplasia 6
5/26/2017 Management of early squamous neoplasms Size & endoscopic findings Histology Management < 5 mm Non-neoplastic Follow up or regular unstained area LG-IEN 5 - 10 mm, Mostly LG-IEN Endoscopic resection regular unstained area F-up q. 6 months Biopsy, at least in number 5 – 10 mm, LG-IEN Endoscopic resection irregular unstained area or HG-IEN/CIS Follow up > 10 mm, HG-IEN/CIS Endoscopic resection suspicious of carcinoma Any size or shape Invasive SCC Surgical resection Chemo / radiation Normal Unequivocally neoplastic lesions Barrett Esoph. LGD HGD Intramucosal CA NEGATIVE LOW-GRADE DYSPLASIA HIGH-GRADE DYSPLASIA • Resemble sporadic • Range of • Marked architectural adenomas epithelia from distortion • Lack of maturation truly normal, • Lack of maturation & top-down pattern normalized, • Marked nuclear • Limited glandular reactive and stratification distortion regenerative • Pencil-shape • Marked nuclear • Diagnosis of hyperchromatic enlargement dysplasia is nuclei • Marked nuclear based on • Limited nuclear hyperchromasia recognition of stratification • Mitoses onsurface what is perceived • Reduced as not dysplasia differentiation • Reduced differentiation • Increased • Increased proliferation proliferation • p53 overexpression or • Clonal character loss no indefinite low grade high grade SQUAMOUS INTESTINALIZED EPITHELIUM EPITHELIUM 7
5/26/2017 Importance of early detection Interobserver variation Age at dx of BE: 61.4yrs Age at cancer dx:66.4yrs 4 LGD 18 HGD 2 Intramucosal CA Age at dx of BE:72.6yrs Age at cancer dx:78.9yrs My diagnosis: High grade dysplasia Corley DA . Gastroenterology ‘ 02 Montgomery E. Hum Pathol 2001 Interobserver variation 3 TINED 3 Indefinite 8 LGD 9 HGD 1 Intramucosal CA My diagnosis: intramucosal CA Montgomery E. Hum Pathol 2001 8
5/26/2017 High-grade dysplasia Why is this high-grade dysplasia? Low-grade dysplasia Retrospective 127 esophago-gastrectomies performed for HGD, or HGD suspicious for CA [CA present in17% of HGD and 74% of HGD/S cases] Histologic feature CA in resection Cribiform/solid growth 73% (33/45) Dilated tubules/necrotic 79% (23/29) debris Ulcerated HGD 83% (19/23) Neutrophils in dysplasia 80% (16/20) Invasion of sq. epith 100% (5/5) None of the above 0 (0/16) 1 of the above 39% (7/18) 2 of the above 83% (10/12) 3 of the above 87% (13/15) 4 of the above 88% (7/8) Zhu W. Am J Clin Pathol 2009;132 9
5/26/2017 Reactive changes mimicking dysplasia Reactive changes or dysplasia? Scattered intra-epithelial inflammation Stromal infla mmation / maturing granulation tissue Nuclear and cellular uniformity Surface maturation Various types of dysplasia Serrated non-Adenomatous Type 2 [foveolar] HGD in the bed of ulcerated BE 10
5/26/2017 Non-adenomatous type dysplasia Non-adenomatous type dysplasia in BE 10 Year Follow-up Maximum dx upon Follow-up Dysplastic N Low-grade High-grade Carcinoma Variant Nonadenomatous 18 0% 78% 17% Adenomatous 24 25% 54% 21% Low-grade 13 46% 31% 23% High-grade 82% 18% 11 Prevalence:6.7% (goblet cells in 62%) Rucker-Schmidt et al. Am J Surg Pathol 94% assoc. typical dyspl. [HGD:+] 2009;33(6):886-93 High rate DNA abnormalities Modern Pathology; 2010-23:834-843 Progression to cancer of various types of dysplasia Prevalence:46%.(HGD:58%) (adjacent IM: 53%) (41 resections w/ dysplasia w or w/o associated inv. ACA) Association with Progression to Dysplasia Conventional Conventional cancer LGD HGD Conventional LGD 1 (5%) (N=22) Conventional HGD 12 (75%) (N=16) Foveolar Dysplasia 4(24%) 13(76%) 8 (47%) (N=17) Serrated Dysplasia 3(50%) 3(50%) 3 (50%) (N=6) HGD LGD Srivastava et al, USCAP 2010 Adenomatous & Hybrid Dysplasia: Prevalence:27%.(HGD:91%;100%) (adjacent IM: 100%/82%%) 11
5/26/2017 Basal Crypt Dysplasia Basal Crypt Dysplasia Can we-reliably-recognize BCD? • 40 bx: 10 BE,9 BCD,10 LGD,9 HGD,2 IMCa [ selected by the index pathologist ] – 5 (blinded) GI pathologists. K for IOV for entire cohort – :0.44 (moderate) • [IMC (K=0.65)-LGD (K=0.31)] • No differences in reproducibility of Basal Crypt Dysplasia (K=0.44)- LGD (K=0.31) or HGD (K=0.46) • When disagreement w/ index diagnosis regarding assessment of BCD (n=17/45 readings), most diagnosed either LGD or HGD • Prevalence:7.3% Metaplastic atypia Metaplastic atypia • 87% have prior or concurrent dysplasia or CA rather than BE w/o dysplasia. • Association particularly significant w/ regard to the assoc. w/ HGD (P=0.004). Coco et al, 2011 Am J Surg Pathol Molecular anomalies & natural history of basal crypt dysplasia DNA abnormalities in basal crypt cells Compared w/ BE, BCD shows: ↑ prevalence rate of p53 positivity (60% vs.13%, P<0.02) ↑ total & basal crypt Ki-67 prolifer ation rate (P<0.001) (similar to LGD or HGD ) Clonal identity ( CDKN2A mutations) Recurring issue w/ basal crypt dysplasia Zhang X Am J Surg Pathol ’ 08; Lomo LC Am J Surg Pathol ’ 06; Khan S. J. Pathol 2013;231; Srivastava A. USCAP 2011 12
Recommend
More recommend