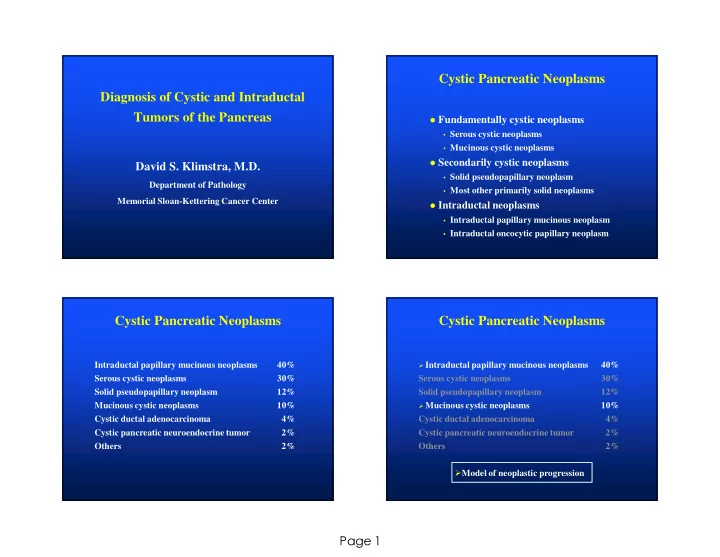
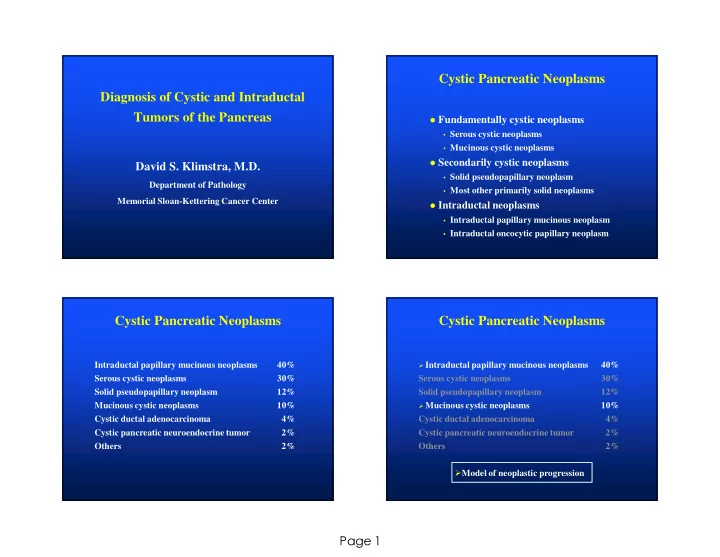
Cystic Pancreatic Neoplasms Diagnosis of Cystic and Intraductal Tumors of the Pancreas � Fundamentally cystic neoplasms • Serous cystic neoplasms • Mucinous cystic neoplasms � Secondarily cystic neoplasms David S. Klimstra, M.D. • Solid pseudopapillary neoplasm Department of Pathology • Most other primarily solid neoplasms Memorial Sloan-Kettering Cancer Center � Intraductal neoplasms • Intraductal papillary mucinous neoplasm • Intraductal oncocytic papillary neoplasm Cystic Pancreatic Neoplasms Cystic Pancreatic Neoplasms Intraductal papillary mucinous neoplasms 40% � Intraductal papillary mucinous neoplasms 40% Serous cystic neoplasms 30% Serous cystic neoplasms 30% Solid pseudopapillary neoplasm 12% Solid pseudopapillary neoplasm 12% Mucinous cystic neoplasms 10% � Mucinous cystic neoplasms 10% Cystic ductal adenocarcinoma 4% Cystic ductal adenocarcinoma 4% Cystic pancreatic neuroendocrine tumor 2% Cystic pancreatic neuroendocrine tumor 2% Others 2% Others 2% � Model of neoplastic progression Page 1
Ductal Adenocarcinoma: Ductal Adenocarcinoma of the Pancreas Survival after Resection Genetic Features 1.0 � Negative Lymph Nodes (n = 263) � K- ras mutations (95%) � Positive Lymph Nodes (n = 411) .8 � p16 abnormalities (90%) Proportion Surviving .6 � p53 mutations (60%) � DPC4 / Smad4 mutations (55%) .4 � Her2/ neu overexpression (95%) .2 � BRCA2 mutations (5%) � STK11/LKB1 mutations (5%) 0.0 0 20 40 60 80 100 120 140 160 180 200 � hMLH-1, hMSH-2 mutations (5%) MONTHS � Promotor methylation of numerous genes � MSKCC 10/15/1983 - 4/14/2002 n = 674 p = 0.0003 Ductal Adenocarcinoma: Genetic Features � K- ras mutations (95%) � p16 abnormalities (90%) � p53 mutations (60%) � DPC4 / Smad4 mutations (55%) � Her2/ neu overexpression (95%) � BRCA2 mutations (5%) � STK11/LKB1 mutations (5%) � hMLH-1, hMSH-2 mutations (5%) Page 2
Precursors to Invasive Ductal Adenocarcinoma • Pancreatic Intraepithelial Neoplasia (PanIN) • Intraductal Papillary Mucinous Neoplasms • Mucinous Cystic Neoplasms PanIN Pancreatic Intraepithelial Neoplasia: Pancreatic Intraepithelial Neoplasia Background • Metaplastic and proliferative lesions long recognized • Some common, age-related, often incidental • Others more associated with invasive ductal PanIN 1B PanIN 1A adenocarcinomas • Spectrum of intraepithelial lesions • Morphologic progression: metaplasia->hyperplasia->dysplasia • Accumulation of genetic abnormalities • “PanIN” terminology proposed, 1994 � Target for earlier detection of pancreatic carcinoma PanIN 2 PanIN 3 Page 3
Molecular Alterations in PanINs PanINs in Autopsy Studies Kozuka* Mukada** 1979 1982 Invasive PanIN 1A PanIN 1B PanIN 2 PanIN 3 Carcinoma n 1174 206 n Invasive carcinoma 24 (2.0%) 1 (0.5%) Invasive carcinoma K- ras 35% 45% 65% 85% 90% Simple hyperplasia 213 (18.1%) 90 (43.7%) Hyperplasia p53 0% 0% <5% 20% 55% Papillary hyperplasia 78 (6.6%) 58 (28.2%) Mild dysplasia HER-2/ neu 82% 86% 92% 100% 69% Atypical hyperplasia 13 (1.1%) 10 (4.9%) Moderate-severe dysplasia p16 24% 19% 55% 71% 95% 6 (2.9%) Carcinoma in situ DPC-4 0% 0% 0% 31% 55% * Cancer 1979; 43:1418-1428 ** Tohoku J Exp Med 1982; 137:115-124 From: Wilentz et al., Cancer Res 60: 2002, 2000. Pancreatic Intraepithelial Progression of Intraductal Neoplasia (PanIN) Neoplasia to Invasive Carcinoma • THREE cases reported • All had documented CIS (PanIN 3) in resection specimens with involvement of margins • Associated with invasive carcinoma: new carcinoma after 9 yrs • Associated with pancreatitis and pseudocyst: carcinoma after 10 yrs • Associated with pancreatitis: carcinoma found 17 months later • Evidence of progression • Difficulty of temporal follow-up of intraductal lesions Brat et al., Am J Surg Pathol 1998; 22: 163-9. Page 4
PanINs: Translation to the Issues Regarding PanINs Surgical Pathology Report � PanI Neoplasm � Molecular phenotype emerging � Reflects clonal nature and expression of cancer associated genes � Natural history largely unknown � Does not mean “requires clinical treatment” � PanINs 1 and 2 � Identification at clinical level difficult � Common incidental findings � Generally not reported � PanIN 3 � Need measurable markers of late stage preinvasive � Strongly suspected to be significant neoplasia (PanIN 3) � However, “the clinical significance and therefore appropriate � Need clinically detectable model for preinvasive management have not been established” (yet) neoplasia Intraductal Papillary-Mucinous Neoplasms � Uncommon tumors of pancreatic ducts with papilla formation and mucin hypersecretion � Clinically detectable � Often lack invasive carcinoma (65-75%) � Histologic similarities with PanINs � (?) Same molecular pathway as PanINs and conventional ductal adenocarcinoma Page 5
Intraductal Papillary-Mucinous Neoplasms: Intraductal Ultrasound Hara et al. Gastroenterology 2002; 122: 34 Page 6
Page 7
Intraductal papillary mucinous neoplasm with invasive colloid carcinoma Intraductal papillary mucinous neoplasm with invasive tubular adenocarcinoma Development of Carcinoma in IPMNs Intestinal type papillae Pancreatobiliary type papillae Colloid carcinoma Tubular carcinoma Page 8
Intraductal Papillary Mucinous Neoplasms: IPMN: Survival Classification WHO 2010 AFIP Fascicle 1.0 1.0 n = 32 n = 32 IPMN with low grade dysplasia IPMN with low grade dysplasia .8 .8 Cumulative Survival Cumulative Survival n = 13 .6 .6 IPMN with intermediate grade IPMN with moderate dysplasia n = 30 .4 .4 dysplasia n = 17 .2 .2 IPMN with high grade dysplasia IPMN with high grade dysplasia p = 0.01 p = 0.008 0 0 0 24 48 72 96 120 144 168 192 0 24 48 72 96 120 144 168 192 IPMN with an associated IPMN with an associated Time (months) Time (months) invasive carcinoma invasive carcinoma non-invasive ( ) non-invasive ( ) invasive colloid carcinoma (- - - -) invasive (- - - -) invasive tubular carcinoma ( - ) Papilla Types in IPMNs Intraductal Papillary-Mucinous Gastric Intestinal Pancreatobiliary Oncocytic Neoplasms: Main vs. Secondary Ducts • 70% involve main duct, 30% confined to secondary (branch) ducts • Secondary duct type confined to head/neck • Secondary duct type in younger patients • Secondary duct type less aggressive • Main duct type: 20% CIS, 37% invasive carcinoma • Secondary type: 15% CIS, 0% invasive carcinoma Terris et al., Am J Surg Pathol 2000; 24: 1372-7. Page 9
Intraductal Tubulopapillary Neoplasm Intraductal Oncocytic Papillary Neoplasm of the Pancreas � Also reported as “Intraductal Tubular Carcinoma” � Approximately 35 cases reported � Mean age = 54 yrs (range = 25-72); F > M � Symptoms: chronic pancreatitis � Location: head > tail; 30% diffuse involvement � Favorable outcome Tajiri et al. Pancreas 2004; 29: 116-122 Yamaguchi et al. Am J Surg Pathol 2009; 33: 1164-1172 Klimstra et al. Am J Surg Pathol 2013; (in press) C.B.D. P.D. Amp. Page 10
Intraductal Neoplasms: Immunohistochemistry Keratins Glycoproteins Cam5.2 100 CEA (m) 85 AE1:AE3 95 CA19-9 90 CK7 70 B72.3 50 CK19 85 CK20 30 Lineage Markers Chromogranin (35) Synaptophysin (35) Trypsin 0 Chymotrypsin 0 Page 11
MUCs in Pancreatic Neoplasia Mucin Expression in MUC1 MUC2 Pancreatic Ductal Neoplasia � Mammary type mucin � Intestinal (goblet) type mucin � Maintenance of lumen formation � Protective function � Inhibitory role in cell-cell, cell- � Mucinous change common in neoplasia � Gel formation stroma interaction � Tumor suppressor activity � Inhibits cytotoxic immunity against � Considered as a marker of “indolent tumor cells phenotype” in pancreas ca. � Activation of tumorigenesis pathways � Increase in normal mucins � Considered as a marker of � CA19-9 “aggressive phenotype” � Expression of tumor-associated glycoproteins � CEA, B72.3, CA125, CA72-4, CA15-3 � Mucins are secreted Tubular (conventional ductal) ca. Colloid (mucinous non-cystic) ca. Morphologic Subtypes of IPMNs: Pancreatobiliary Type MUC1 MUC2 MUC1 MUC2 MUC1: 90% of cases MUC1: 0% of cases MUC5AC MUC2: 1% of cases MUC2: 100% of cases Page 12
Morphologic Subtypes of IPMNs: Morphologic Subtypes of IPMNs: Intestinal (Villous) Type Gastric Foveolar Type MUC1 MUC1 MUC2 MUC2 MUC5AC MUC5AC MUC Expression in Pancreatic Neoplasia CDX2 in Pre-invasive Neoplasia � IPMN Tubular Colloid IPMN IPMN IPMN PanIN Ca Ca Int. PB Gastric � Gastric: 0/17 (0%) � Intestinal: 12/13 (95%) � Pancreatobiliary: 0/9 (0%) MUC1 +++ - - +++ - +++ � Oncocytic: 0/2 (0%) � PanIN All: 2/23 (9%) � MUC2 - +++ +++ - - - p = 0.000001 Page 13
Recommend
More recommend