ROLE OF PRIMARY CARE IN MANAGING Azlina Amir Abbas Dept of Orthopaedic Surgery HIP & KNEE OSTEOARTHRITIS Faculty of Medicine, University of Malaya
Most common cause of joint pain Functional limitation and reduced quality of life
SITES
CLASSIFICATION Primary Joint dysplasia DDH, Perthe’s, Blount’s disease No obvious cause Trauma Fractures involving articular surface Secondary Joint instability After certain predisposing factors Occupation Obesity
FAILURE OF CHONDROCYTES TO REPAIR DAMAGED CARTILAGE NORMAL OSTEOARTHRITIS
CLINICAL FEATURES
DIAGNOSIS Diagnose osteoarthritis clinically without investigations if a person: is 45 or over and has activity-related joint pain and has either no morning joint-related stiffness or morning stiffness that lasts no longer than 30minutes. Be careful of atypical features in history and physical examination NICE Guidelines: OA Care & Management 2014
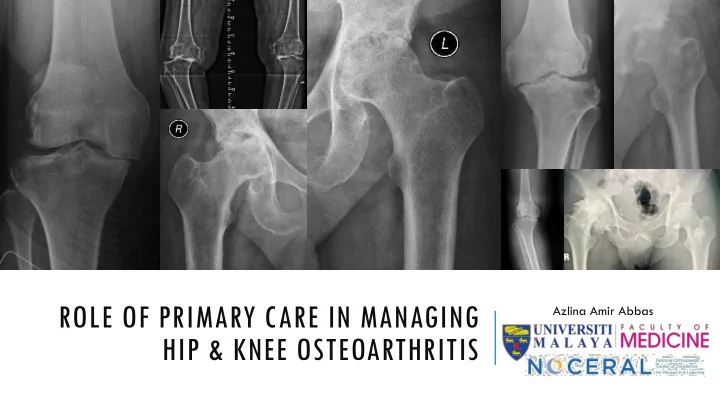
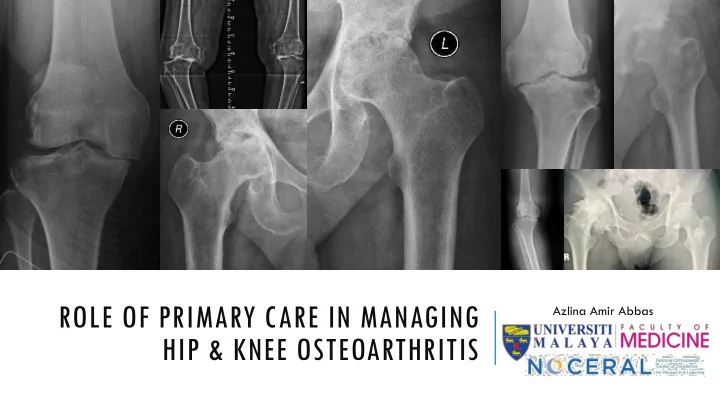
BASIC INVESTIGATIONS: Weight-bearing films RADIOGRAPHS - KNEE
BASIC INVESTIGATIONS: Pelvis RADIOGRAPHS - HIPS
WHAT ARE YOU LOOKING FOR IN RADIOGRAPHS? Reduction in joint space Osteophytes Subchondral sclerosis Subchondral cysts
OTHER INVESTIGATIONS? Generally not necessary If suspect secondary OA MRI Blood investigations: Inflammatory arthritis, Septic arthritis Joint aspiration for FEME/C&S: large effusion, gout, septic arthritis CT CT or MRI: post-traumatic, congenital deformity
RED FLAGS! Infection Needs immediate/early Instability referral Fracture
Mood Expectations Occupation TREATMENT PRINCIPLE: Comorbid- Sleep ities PATIENT-CENTRED Holistic Approach CARE Pain Social/ Take into account individual needs and Assessment Function preferences Health Relation- beliefs ships NICE Guidelines: OA Care & Management 2014
NON-OPERATIVE TREATMENT
PAIN RELIEF: THE IDEAL Works quickly Lasts a long time Causes few side effects Can be used alongside other pain relievers Does not have physiological effects eg on: • Bleeding • Blood pressure • Renal function • Cognitive or other CNS effects
WHO PAIN LADDER
WHO PAIN LADDER
HOW NSAIDS & COXIBS WORK Prostaglandin Pathway • nsNSAIDs inhibit COX-1 and COX-2 • COXIBs inhibit COX-2 only Damaged joint tissue Inflammatory chemical mediators Nociceptive afferent fiber Spinal cord
GASTROINTESTINAL RISK WITH NSNSAIDS/COXIBS Pooled Relative Risks and 95% CIs of Upper Gastrointestinal Complications 100 Pooled relative risk log scale 18.5 11.5 10 7.4 4.4 4.1 4.1 4.1 3.9 3.8 3.5 3.3 2.9 2.3 1.8 1.4 1.5 1 0.1 NSAIDs CI = confidence interval; coxib = COX-2 inhibitor; NSAID = non-steroidal anti-inflammatory drug; nsNSAID = non-selective non-steroidal anti-inflammatory drug Castellsague J et al. Drug Saf 2012; 35(12):1127-46.
NSNSAIDS/COXIBS AND CARDIOVASCULAR RISK Composite includes non-fatal myocardial infarction, non-fatal stroke, or cardiovascular death compared with placebo; chart based on network meta-analysis involving 30 trials and over 100,000 patients. Coxib = COX-2 inhibitor; nsNSAID = non-specific non-steroidal anti-inflammatory drug Trelle S et al. BMJ 2011; 342:c7086.
Looks like endorphins HOW OPIOIDS AFFECT PAIN Binds to opioid receptors in the brain, spinal cord, and GI tract INTERACTION WITH THE MU ( Μ ) OPIOID RECEPTOR AS THE Release of dopamine – block pain transmission to PRIMARY TARGET brain Modify perception, modulate transmission Brain and affect transduction by: Altering limbic system activity; Perception modify sensory and affective pain aspects Activating descending pathways that modulate transmission in spinal cord Affecting transduction of pain stimuli to nerve impulses Descending Ascending Transmission Transduction modulation input Nociceptive afferent fiber Spinal cord Reisine T, Pasternak G. In: Hardman JG et al (eds). Goodman and Gilman’s: The Pharmacological Basics of Therapeutics. 9th ed. McGraw -Hill; New York, NY: 1996; Scholz J, Woolf CJ. Nat Neurosci 2002; 5(Suppl):1062-7; Trescot AM et al. Pain Physician 2008; 11(2 Suppl):S133-53.
DIFFERENT MODE OF ACTION: OPIOIDS VS NSAIDS/COXIBS Central Nervous System Pathway • Opioids have no effect on COX enzyme. Prostaglandin Pathway • nsNSAIDs inhibit COX-1 and COX-2 • COXIBs inhibit COX-2 only
Opiates are safer for GI Respiratory CNS
OPIOIDS: SIDE EFFECTS Common: Confusion, drowsiness, hallucinations, bad dreams, dry mouth, nausea, vomiting, constipation Less common: Pruritus, sweating, opioid-induced hyperalgesia, myoclonus, delirium Respiratory depression rare if titrated carefully to individual patient response Side effects may become apparent as the opioid dose is increased. May be managed with other medications, e.g. antiemetics/antipsychotics but sometimes they persist or become intolerable and thus dose-limiting
Opiates are useful where alternatives are contraindicated or not tolerated or don’t work Opiates can be a nightmare if used in the wrong clinical context Especially in chronic pain syndromes Emphasizes the importance of the comprehensive pain assessment and using a holistic model OPIATES: USE WITH CAUTION
HOT, COLD, ELECTRO- THERAPIES Adjunct Heat helps soothe stiff joints and relax muscles. Cold helps numb sharp pain and reduce inflammation TENS: stimulating nerves closes a "gate" mechanism in the spinal cord, and that can help eliminate the sensation of pain
PROTECT JOINT FROM OVERLOADING Weight loss weight loss of 10% or more over 18 months led to a 50% reduction in pain and significant improvements in mobility for people with arthritic knees weight loss of 20% or more led to an additional 25% reduction in pain (Messier et al, Arthritis Care & Research 2018)
EXERCISES / PHYSIOTHERAPY Low impact Local muscle strengthening Hip: Hip abductors Knee: Quadriceps Mobilization exercises Improve general aerobic fitness
SUPPLEMENTS? Glucosamine etc Viscosupplementation: Intra-articular hyaluronic acid injections
STEROIDS – ORAL & INJECTIONS? Local Adverse Reactions Altered skin pigmentation Atrophy of subcutaneous and periarticular tissue Tendon rupture, tendon attrition Cartilage damage
SURGICAL TREATMENT
INDICATION Pain not responding to conservative treatment Mechanical pain/symptoms NOT EVERY PATIENT WITH OSTEOARTHRITIS NEEDS SURGERY! Severe deformity Reducing/poor/unacceptable Quality of life
SPEEDING THINGS UP Optimise any comorbid conditions Nutrition Obesity Diabetes mellitus HbA1C < 8% Blood pressure No history of traditional medication use/ prolonged steroid ingestion – Cushing syndrome No source of infection
SURGICAL INTERVENTIONS Arthroscopic washout Osteotomy – realignment procedure NOT EVERY PATIENT WITH OSTEOARTHRITIS NEEDS JOINT REPLACEMENT!
SURGICAL INTERVENTIONS Joint replacement
SOME (MIS)CONCEPTIONS ABOUT JOINT REPLACEMENT SURGERY – THE MALAYSIAN CONTEXT I won’t be I’m too old for able to walk joint after surgery replacement The implant You are going only lasts 5 to chop off years half my bone The surgery is The implant very painful The surgery is very and has many heavy dangerous complications
EDUCATION Enhance understanding of the condition and its management, and to counter misconceptions On-going – not just one-off
WE ARE A TEAM! Managing patients with osteoarthritis is a team effort Treatment: Non-operative & Operative Always attempt non-operative unless severe functional limitation or pain Refer for surgery before there is prolonged and established functional limitation and severe pain Education and information sharing is an integral part of the management CONCLUSION EMPOWER YOUR PATIENTS! Thank you. azabbas@um.edu.my
Recommend
More recommend