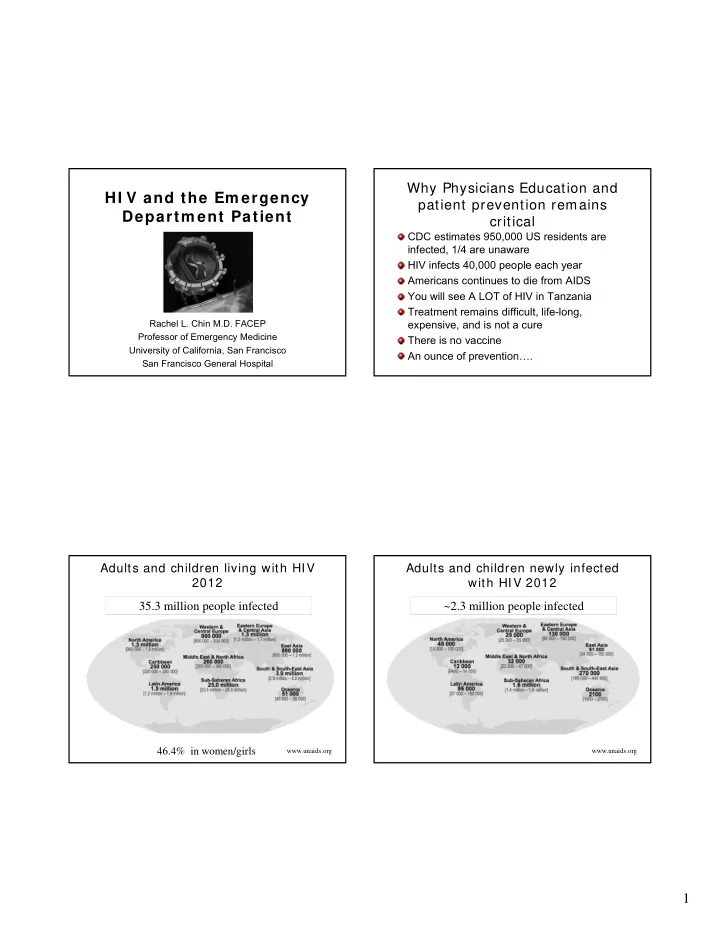
Why Physicians Education and HI V and the Em ergency patient prevention remains Departm ent Patient critical CDC estimates 950,000 US residents are infected, 1/4 are unaware HIV infects 40,000 people each year Americans continues to die from AIDS You will see A LOT of HIV in Tanzania Treatment remains difficult, life-long, Rachel L. Chin M.D. FACEP expensive, and is not a cure Professor of Emergency Medicine There is no vaccine University of California, San Francisco An ounce of prevention…. San Francisco General Hospital Adults and children living with HIV Adults and children newly infected 2012 with HIV 2012 35.3 million people infected ~2.3 million people infected 46.4% in women/girls www.unaids.org www.unaids.org 1
Adults and children Death from AIDS 2012 Rise of HI V infection ~1.6 million deaths Safe sex fatigue: decrease condom use, increased unprotected sex www.unaids.org Rise of HI V infection Safe sex fatigue: decrease condom use, increased unprotected sex Medications (HAART/ART) 2
3
Rise of HI V infection Safe sex fatigue: decrease condom use, increased unprotected sex Medications (HAART/ART) Increased access to sex: internet, circuit parties, public sex venues Increased recreational drug use, esp crystal methamphetamines and ecstasy Rise of HI V infection Safe sex fatigue: decrease condom use, increased unprotected sex Medications (HAART) Increased access to sex:internet, circuit parties, public sex venues Increased recreational drug use, esp crystal methamphetamines and ecstasy Viagra Viagra + Ecstasy = Sextasy 4
Case # 1 Objectives Learn how to recognize subtle complaints in the most 28 year old HIV positive man complains of dry common life-threatening AIDS infections. cough for 2-4 weeks and fevers. He has no Identify what tests may be helpful in the diagnosis of history of Opportunistic Infection (OI ’ s) and the most common OI in the US. takes no medicines. Normal Vital signs. O 2 saturation 95%. CXR clear. Summarize the treatment and management of these OI ’ s. Learn about the adverse effects of HIV-Therapy Become aware of drug induced metabolic changes and Immune Reconstitution Syndrome What is the Stage of HIV infection? Returns 10 days later with diffuse pneumonia Defined by CD4 count: and goes to the ICU with the diagnosis of PCP. • Early: CD4 > 500/mm 3 • Intermediate: CD4 200-500/mm 3 What could have changed this management? • Late: CD4 < 200/mm 3 What was the stage of the HIV infection? • ?Very Late: CD4 < 50/mm 3 5
Viral Load Monitors therapy Always need CD4 count in your decision making It is essential in suggesting the medications are not working either to < 200 and no PCP prophylaxis, all URI ’ s • non-adherence need close follow up • drug interactions > 200 or on prophylaxis (and compliant), then • malabsorption bronchitis • mutations Pulmonary disease is one of the most common HIV-related emergencies PCP is the leading AIDS-defining condition in the United States Absolute lymphocyte count (ALC) Pneumocystis jiroveci ( “ yee row vet zee ” - • < 950 x 10 6 cells/ μ L - CD4 < 200 x 10 6 cells/ μ L formerly carinii) pneumonia Pretest probability CDC. HIV/ AIDS Surveillance Reports Academic Emergency Med 2011;18:385-389 Emerging Infectious Diseases 2002;8(9):891-896 6
P neumo c ystis jiroveci PCP Chest Radiographic P neumonia Presentation Bilateral > Unilateral, Symmetric > Asymmetric Clinical presentation Pattern • CD4 cell count ≤ 200 cells/mm 3 • Interstitial (reticular) or granular • Symptoms: fever, DOE, dry cough , fatigue • Alveolar (consolidation) • Duration: >2-4 weeks • Cyst(s) • Signs: Nonspecific • Normal • Labs: Serum LDH often elevated • Pneumothorax Atypical • Intrathoracic adenopathy • Pleural effusion(s) PCP Chest Radiographic Treatment Presentation Trimethoprim-sulfamethoxazole Clindamycin + Primaquine Trimethoprim + Dapsone Atovaquone Pentamidine Treat for 21 days followed by prophylaxis • Steroids 40 mg PO BID if Pa02 < 70 mm Hg 7
Bacterial Pneumonia Case # 2 Clinical presentation 28 year old HIV + man complains of headache. No medications. • CD4 cell count: any • Symptoms: Fever, SOB, chest pain, productive What do you need to know? cough w/ purulent sputum Is his HIV infection early, intermediate, or • Duration: 3-5 days late? • Signs: Focal lung findings CD4 < 100, need LP to rule out cryptococcal • Labs: WBC often (relatively) elevated meningitis Cryptococcal meningitis CNS Emergencies Clinical presentation Cryptococcal meningitis • Signs: ± meningeal Cryptococcal signs neoformans is the most • Dx: common fungus • CT/MRI usually responsible for infections negative in patients with AIDS. • CSF CrAg + > 90-95% Clinical presentation Treatment • CD4 < 100 cells/mm 3 • Ampho B +/- Flucytosine • Symptoms: fever, for 2 wks headaches • Oral fluconazole for chronic suppressive • Duration: weeks to therapy months • Manage increased ICP, hydrocephalus, seizures 8
Cerebral Toxoplasmosis CNS Emergencies Diagnosis Cerebral Toxoplasmosis • CT/MRI: multiple ring- enhancing lesions Toxoplasma gondii, a parasite, is the most • Inferred by response common cause of focal brain lesions in to empiric therapy people with AIDS Treatment Clinical presentation • Pyrimethamine, • CD4 < 200 cells/mm 3 sulfadiazine, folinic • Symptoms: headache, fever, AMS, focal signs acid over days to weeks • Expect clinical and • Signs: seizures (25%-50%), focal signs over days radiologic to weeks improvement in 2 • Labs: Toxo titers usually positive weeks Ocular Emergencies Ocular Emergencies CMV retinitis is the most common vision- threatening condition in people with AIDS Clinical presentation • CD4 < 50 cells/mm 3 • Symptoms: blind spots, peripheral visual field loss, flashing lights, floaters, decreased or blurred vision 9
Prophylaxis and Treatment of Ocular Emergencies OI ’ s- What ’ s New? Cessation of primary prophylaxis for PCP Treatment • Short-term data CD4 > 200 for 3-6 months, no PCP • Goal is to slow down progression, prevent further Cessation of prophylaxis for disseminated MAC spread of the infection in the retina and preserve • CD4 > 100-200 visual function • Valganciclovir, foscarnet, and cidofovir Cessation of treatment of CMV retinitis, • CD4 > 200 • Prophylaxis Prophylaxis for HSV (genital or oral) • Outbreaks up-regulate HIV viral production and can threaten HIV viral suppression, shed both HSV and HIV CDC, MMWR Therapies currently on market HAART/ ART Nucleoside and Protease inhibitors: NNRTI ’ s: nucleotide RTIs • Indinavir, IDV • Delavirdine (DLV) • Zidovudine, AZT ( Retrovir ) ( Crixivan) • Nevirapine, NVP • Abacavir, ABC ( Ziagen ) Highly active antiretroviral therapy/ • Saquinavir, SQV ( Viramune) • Lamivudine, 3TC ( Epivir ) ( Invirase, hgc ) • Efavirenz, EFV antiretroviral therapy • Didanosine, ddI ( Videx ) • Nelfinavir, NFV ( Sustiva) • Stavudine, d4T ( Zerit ) ( Viracept) Combination of at least 3 drugs • Etravirine* • Tenofovir, TFV ( Viread ) • Amprenavir, APV (Intelence) • Emtricitabine, FTC Standard of care ( Agenerase) ( Emtriva ) Fusion • Atazanavir, ATZ • Combivir (AZT/3TC) inhibitors: • (Reyataz) Trizivir (AZT/3TC/ABC) • Enfuvirtide, ENF • Fosamprenavir, FPV • Epzicom (3TC/ABC) or T20 ( Fuzeon) (Lexiva) • Truvada (FTC/TFV) Combination • Kaletra CCR5 receptor • A tripla (lopinavir/ritonavir) antagonist (EFV/FTC/TFV) • Tipranavir ( Aptivus) • Maroviroc (Selzentry)* • Darunavir ( Prezista)* Integrase inhibitor *Approved in past year • Raltegravir (Isentress)* Orange text – combination agents 10
Case # 3 Case # 3 135 103 3 84 40 year old HIV positive woman complains of Labs 4.5 12 0.5 diffuse RUQ pain, anorexia, nausea, and malaise. No history of gallstones or alcohol. SGOT-85, SGPT-63, Alk phos-239 She is on HIV medications. CD4 400/mm 3 . Lipase 342 Ultrasound showed no stones CT scan showed a fatty liver Case # 3 Mitochondrial toxicity She was treated for pancreatitis, floor bed Lactic acidosis with or without hepatic was ordered. One of her medications were steatosis stavudine (d4T). • May be sudden or gradual onset What was missed was lactic acidosis with • Signs and sx: nausea, vomiting, abdominal pain, hepatic steaotosis associated with weight loss, malaise, fatigue, SOB, occ. fevers, nucleoside reverse transcriptase (NRTI) diarrhea, tachycardia and tachypnea medication. Her lactate level was 9.2. • Labs: abnormal LFTs, moderate to severe Transferred to an ICU bed. acidosis (lactate > 5 mmol/L) Bicarb continued to drop to 10 despite IVF • mortality 80% in lactate levels > 10 mmol/L with bicarbonate. 11
Emergencies Related to HIV www.aidsmeds.com Therapy Mitochondrial toxicity • Lactic Acidosis Pancreatitis Rash by Non-Nucleoside Reverse Transcriptase Inhibitors Drug interactions HIVinsite.com www.epocrates.com 12
Recommend
More recommend