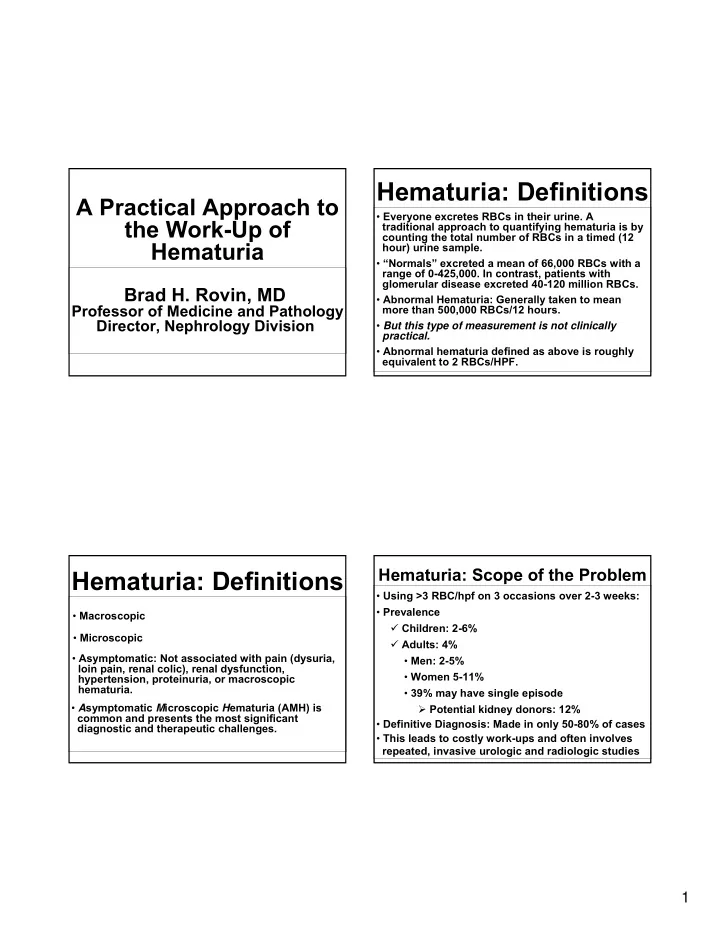
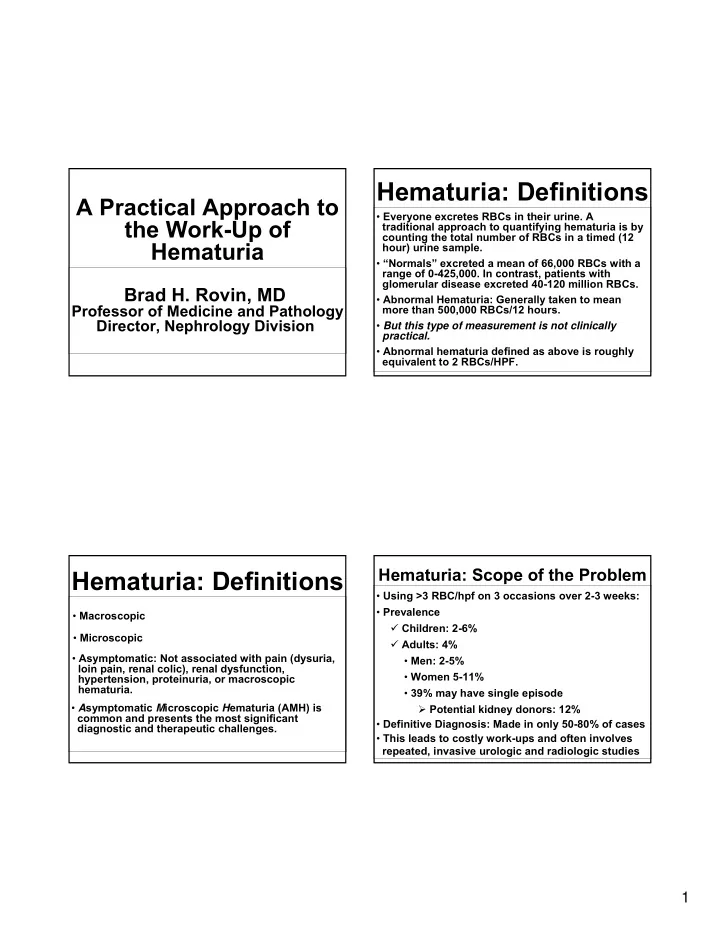
Hematuria: Definitions A Practical Approach to • Everyone excretes RBCs in their urine. A the Work-Up of traditional approach to quantifying hematuria is by counting the total number of RBCs in a timed (12 Hematuria hour) urine sample. • “Normals” excreted a mean of 66,000 RBCs with a range of 0-425,000. In contrast, patients with glomerular disease excreted 40-120 million RBCs. Brad H. Rovin, MD • Abnormal Hematuria: Generally taken to mean Professor of Medicine and Pathology more than 500,000 RBCs/12 hours. Director, Nephrology Division • But this type of measurement is not clinically practical. • Abnormal hematuria defined as above is roughly equivalent to 2 RBCs/HPF. Hematuria: Scope of the Problem Hematuria: Definitions • Using >3 RBC/hpf on 3 occasions over 2-3 weeks: • Prevalence • Macroscopic � Children: 2-6% • Microscopic � Adults: 4% • Asymptomatic: Not associated with pain (dysuria, • Men: 2-5% loin pain, renal colic), renal dysfunction, • Women 5-11% hypertension, proteinuria, or macroscopic hematuria. • 39% may have single episode • A symptomatic M icroscopic H ematuria (AMH) is � Potential kidney donors: 12% common and presents the most significant • Definitive Diagnosis: Made in only 50-80% of cases diagnostic and therapeutic challenges. • This leads to costly work-ups and often involves repeated, invasive urologic and radiologic studies 1
Approach to Hematuria - Confirm True Hematuria Glomerular Hematuria-Characteristics • False positive dipstick: The dipstick relies on oxidation of an organic peroxide on the test strip Acanthocytes: by the peroxidase-like activity of hemoglobin. This 98% specific, 52% sensitive can be mimicked by myoglobin, povidone-iodine, if >5% of RBCs in a urine H 2 O 2 , bacterial peroxidases. sample; sensitivity >80% if found in 3 consecutive • False negative dipstick: Presence of ascorbic acid urine samples (supplements), formaldehyde (preservative), low pH. Not inducible by changes in • Dipstick sensitivity-93-100%, specificity-60-80%: pH, osmolality Negative predictive value ~98%. (Schroder, BMJ, 1994; Huussen, Neth J Med, 2004) Endogenous Globins, porphyrins Pigmenturia Exogenous Beets, rhubarb, phenothiazines Note: Alkaline urine dissolves casts! Use Urine Microscopy to Verify RBCs Approach to Hematuria Glomerular Hematuria-Differential Diagnosis Identify Origin of the Blood Glomerular Hematuria Non-Glomerular Hematuria Basket- < 250 nm weave Micro- or Macroscopic Micro- or Macroscopic Normal IgA Nephropathy Thin GBM Alport’s Abnormal Morphology Normal Morphology Proteinuria, active sediment Isolated Finding PMN May be familial - Check first degree relatives Humps - Look for hearing loss Post-Infectious Systemic Inflammatory/Vasculitides 2
Effect of Proteinuria on the Renal Biopsy for Hematuria? Differential Diagnosis of Hematuria YES NO Proteinuria Present ( ≥ 500 mg/day) No Proteinuria Microscopic Hematuria in 135 patients: Abnormal Renal Fxn (Cr ≥ 1.3) Normal (stable) Renal Fxn Proteinuria <0.3 g/d Proteinuria up to 2.4 g/d Possible Systemic Process No Systemic Process Thin GBM 43% IgAN 46% Potential Kidney Donor IgAN 20% FSGS 13% RATIONALE FOR NOT DOING A BIOPSY: The Normal 37% Membranous, MPGN, AIN glomerular diseases that are most likely to Acute prolif, Alport’s cause isolated hematuria have no proven treatments, and in the absence of proteinuria Hall et al, Clin Nephrol, 2004 carry an excellent renal prognosis Natural History of Hematuria in 49 Pathologic Diagnosis of Hematuria Patients with Negative Urologic Evaluation Microscopic Hematuria in 165 patients Presentation IgAN Thin GBM Normal* Misc** with no other renal or systemic findings: # of patients 12 13 20 4 Pathologic Diagnosis % of Patients Mean Age 30 35 30 44 None 53 (but 13%-no EM) Macroscopic Hematuria 6 1 10 1 IgAN 30 Cr Clearance 109 115 113 93 Thin GBM 4 11 Year Follow-up Mesangial Proliferation 7 Hematuria 10 13 7*** 3 FSGS 3 Cr Clearance 100 110 113 75 *Mean Duration Hematuria 4 years; ** Int Nephritis (3), FGS (1); ***5 of the 7 patients HTN, Membranous, Int Nephritis 3 developed stones over the 11 year follow-up, suggesting they may have had crystaluria to start. Topham et al, Q.J. Med., 7:329:1994 Niewuhof et al., KI, 49:222, 1996 3
Non-Glomerular Hematuria- Proteinuria Changes Everything Differential Diagnosis In IgAN: • Nephrolithiasis Proteinuria (g/d) ESRD over 7-10yrs (also hypercalcuria, hyperuricosuria) 0.3-0.99 10% • Malignancy 1-1.99 25-35% • Infection 2-2.99 40% • BPH >3 60% • Cysts (non-simple) Hall et al, Clin Nephrol 2004 Natural History of Hematuria: Is Screening for Non-Glomerular Hematuria- Microscopic Hematuria Recommended? Differential Diagnosis Iseki et. al. (Kidney Int., 49:800, 1996) screened 107,192 subjects in Japan with a single urine dipstick, and found that the incidence of hematuria increased linearly with age: 18-29 >80 • Anatomic Lesions Men 0.9% 8.5% � A-V fistula/malformation Women 7.3% 15.3 � Angiomyolipoma Ten years after the original dipstick the prevalence of ESRD was � Hemangioma determined and the odds ratio for ESRD calculated: � Renal variceal veins Men vs. Women 1.4 Hematuria vs. no hematuria 2.3 Proteinuria vs. no proteinuria 14.9 This low, but increased risk suggests patients with an incidental finding of microscopic hematuria should be followed for any indication (proteinuria, hypertension) of developing renal disease. 4
Non-Glomerular Hematuria- Hematuria in Adults Differential Diagnosis Diagnosis Microscopic Macroscopic • Hematologic Issues (n>2000) (n>1200) Cancer 2.3-5% 23% � Coagulopathy � Intrinsic Nephrolithiasis 5% 5-11% � Iatrogenic (58% may have underlying Infection 1.7-4% 33% urinary tract disease) BPH 3-13% 13% � Platelet dysfunction Intrinsic Renal 2-11% - � Hemoglobinopathy No Diagnosis 43-57% 8-21% Sutton, JAMA, 263:2475, 1990; Boman, Scand J Urol Neph, 2001; Murakami, J Urol, 144:49, 1990, Sultana, Br J Urol, 78:691,1996 Non-Glomerular Hematuria- Approach to Patients with Asymptomatic Differential Diagnosis Non-Glomerular Hematuria + Image Upper Tract Appropriate Referral • Other Helical CT (MRI?)>US>IVU - + � Ischemia/infarct Cytology (??) Cystoscopy -virtual (SENS=55%;SPEC=99%) cystoscopy? - � Emboli - Age <40, no risk Age >40 or risk factors � Exercise factors for bladder CA for bladder CA � Malignant hypertension - R/O crystaluria, Cystoscopy prostate exam - - - Consider angiogram Observation 5
Imaging of the Upper Urinary Tract Hematuria in Adults-Cancer as a Function of Age, Symptoms, and Degree Traditionally, upper tract imaging has been done with IVU or US US vs CT for Small Lesions IVU vs Helical CT for Hematuria 35 Size (mm) US CT Lesions missed by IVU but found by CT in 74 patients with negative work-up 30 <5 0% 47% Papillary Necrosis 25 25 5-10 21% 60% Calculi (including sponge) 28 10-15 28% 75% 20 Cancer 15-20 58% 100% 15 -renal cell 6 20-25 79% 100% Cancer (%) -transitional cell 3 25-30 100% 100% 10 Angiomyolipoma/cyst 4 For small lesions CT is superior than US 5 Infarction 3 0 Vascular anomalies 5 GH<50 GH>50 AMH<50 AMH>50 SMH<50 SMH>50 Jamis-Dow et. al., Radiology, 1996 Lang et. al., Urology, 2003. ACCURACY of CT estimated at 98.3%; IVU 80.9% (Sears et. al., J. Urol., 2002) The combination of US+IVU vs CT has not been assessed Sultana et al, Br. J. Urol., 78:691, 1996 Risk Factors for Urothelial Cancers When No Diagnosis is Made • Age (>40) • Sex (males >> females) • Smoking • If no diagnosis is made after initial evaluation, patients should be followed every six months • Episodes of macroscopic hematuria • Irritative voiding symptoms; previous GU history • It is not clear how often to repeat urologic studies. In one large study of 225 patients (Murakami et al, • Exposure to aromatic amines/benzenes 1990) 91% of the serious (eg cancer, stones) • Pelvic radiation lesions were found at the initial visit. • Exposure to cyclophosphamide • An additional 9% (22 cases, 4 malignancies) were • Phenacetin use (heavy) discovered over the next 1.5 years with extensive urologic testing every 6 months. • Exposure to aristolochic acid (herbal weight-loss) • Parasitic infection ( Schistosoma haematobium) 6
Why do we care about proteinuria? Approach to • Second most important parameter after Proteinuria GFR to evaluate kidney function � Present in early kidney disease • Even before decline in GFR or ↑ serum Rosemarie Shim, MD, MS creatinine Assistant Professor � Key risk factor for loss of kidney function • Marker for severity of CKD, Division of Nephrology hyperfiltration, ongoing injury � Risk factor for CVD and CV mortality • Generalized endothelial dysfunction ‘Clinical evaluation of kidney function.’ Hsu, C-Y. Primer on Kidney Diseases, 2005 Objectives Detection of Proteinuria • Dipstick urinalysis • Define abnormal proteinuria � Rough estimation of urinary protein • Review detection of proteinuria excretion • Classify degree of proteinuria • Spot urine protein/creatinine ratio • When to refer to a nephrologist - � Good correlate to 24 hour urinary recognition of an urgent referral protein excretion • Review differential diagnosis • 24 hour urine collection • Review diagnostic workup � Precise quantification 7
Recommend
More recommend