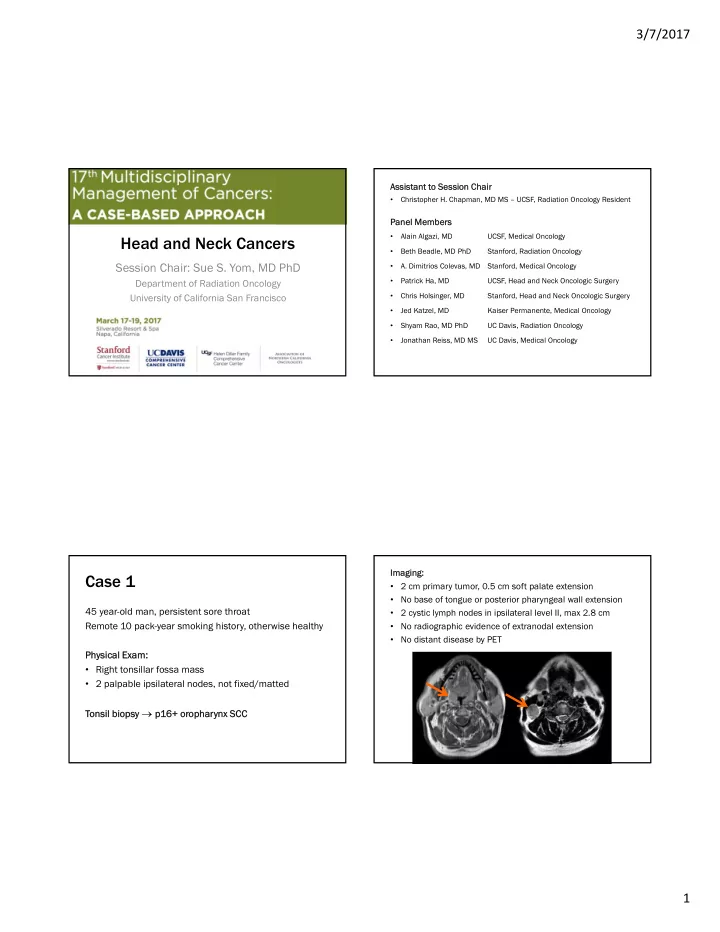
3/7/2017 Assi Assistant t t to Sess Session Chair Chair Christopher H. Chapman, MD MS – UCSF, Radiation Oncology Resident • Panel Membe nel Members Alain Algazi, MD UCSF, Medical Oncology Head and Neck Cancers • Beth Beadle, MD PhD Stanford, Radiation Oncology • Session Chair: Sue S. Yom, MD PhD A. Dimitrios Colevas, MD Stanford, Medical Oncology • Patrick Ha, MD UCSF, Head and Neck Oncologic Surgery Department of Radiation Oncology • Chris Holsinger, MD Stanford, Head and Neck Oncologic Surgery University of California San Francisco • Jed Katzel, MD Kaiser Permanente, Medical Oncology • Shyam Rao, MD PhD UC Davis, Radiation Oncology • Jonathan Reiss, MD MS UC Davis, Medical Oncology • Imagi Imaging: Case 1 • 2 cm primary tumor, 0.5 cm soft palate extension • No base of tongue or posterior pharyngeal wall extension 45 year-old man, persistent sore throat • 2 cystic lymph nodes in ipsilateral level II, max 2.8 cm Remote 10 pack-year smoking history, otherwise healthy • No radiographic evidence of extranodal extension • No distant disease by PET Physical Exam: Ph ysical Exam: • Right tonsillar fossa mass • 2 palpable ipsilateral nodes, not fixed/matted biopsy p1 Tonsil b To p16+ or 6+ orop opharynx SCC SCC 1
3/7/2017 ST STAGING AJCC 7 th Ed. AJCC 8 th Ed. cT1 N2b M0 stage IVA cT1 N1 M0 stage I AJCC 8 th ed. Clinical nodal stage: p16+ oropharynx • cN1 cN1: Ipsilateral node(s), all ≤ 6 cm • cN2 cN2: Bilateral/contralateral node(s), all ≤ 6 cm • cN3 cN3: Any node > 6 cm Question 1.1 ST STAGING This patient is not interested in surgical options. AJCC 7 th Ed. AJCC 8 th Ed. Treatment recommendation? cT1 N2b M0 stage IVA cT1 N1 M0 stage I 1. Radiation with concurrent cisplatin 2. Radiation with concurrent cetuximab Clinical Stage Grouping: p16+ oropharynx 3. Induction chemotherapy then carboplatin-RT 7 th Ed. 8 th Ed. 4. Induction chemotherapy then cetuximab-RT cN0 cN1 cN0 N1 cN2 cN2 cN3 N3 cN0 cN1 cN0 N1 cN2 cN2 cN3 N3 5. Radiation alone cT0 cT0 cT0 cT0 III III IV IVA IVB VB I II III III cT1 cT1 cT1 cT1 I III III IV IVA IVB VB I I II II III III cT2 cT2 cT2 cT2 I I II II III III II II III III IVA IV IVB VB cT3 cT3 cT3 cT3 III III III III IVA IV IVB VB II II II II II II III III cT4 cT4 III III III III III III III III cT4a cT4a IV IVA IVA IV IVA IVB VB 2
3/7/2017 Paradigm RTOG 10-16: Phase III Trial of Radiotherapy ICT CRT Plus Cetuximab versus Chemoradiotherapy Carboplatin (every week) CR Daily RT (days 1-5) in HPV-Associated OPSCC Docetaxel 7 weeks R Cisplatin A Paradigm 5-FU N Stage III/IV SCCHN every 3 weeks, 3 cycles Docetaxel (every week for 4 wks) D OPSCC p16+ IHC • Oral cavity, Daily/twice-daily RT (days 1-5) PR O All M0 stages oropharynx, 6 weeks M hypopharynx, larynx I • Expected N=330 Cisplatin (weeks 1, 4) Z Daily/twice-daily RT (days 1-5) E 6 weeks p16 central review Stratification by T/N stage, KPS, Smoking DeCIDE ICT CRT R RANDOMIZE Docetaxel (day 1) A Cisplatin (day 1) N DeCIDE 5-FU (days 1-5) D Chemotherapy and RT- O every 3 weeks, 2 cycles Docetaxel (day 1) naïve SCCHN Accelerated IMRT Accelerated IMRT M 5-FU (days 0-4) • Expected N=400 I Hydroxyurea (days 0-4) 70 Gy in 6 weeks 70 Gy in 7 weeks Z Cisplatin 100 mg/m 2 x 2c Twice-daily RT (days 1-5) Cetuximab 8 doses E every 2 weeks, 5 cycles Two randomized phase III studies of E1308: Phase II Trial of Induction Chemotherapy Followed Reduced-Dose Radiation and Weekly Cetuximab in Patients induction + chemoRT vs chemoRT with HPV-associated Resectable OPSCC in U.S. : Marur et al., J Clin Oncol 2016 Paradigm 80 patients with HPV/p16+ stage III-IV OPSCC IC cisplatin/paclitaxel/cetuximab x3c DeCIDE 70% CR 54 Gy / 27 frx with concurrent cetuximab 30% < CR 69.3 Gy / 33 frx with concurrent cetuximab All patients: 2-yr PFS 78%, 2-yr OS 91% All reduced dose patients (n=51) ≤ 10 pk-yr and < T4N2c (n=27) 2-yr PFS 80% 2-yr OS 94% 2-yr PFS 95% 2-yr OS 95% 3
3/7/2017 NRG HN-002: A Randomized Phase II Trial for Patients with p16 Positive, Non-smoking Associated, Locoregionally Advanced Oropharyngeal Cancer OPSCC p16+ IHC ≤ 10 pk-yr smoking hx T1-2, N1-2b or T3, N0-2b p16 central review Stratification by unilateral vs. bilateral RT Patient changes his mind, now wants surge surgery: y: Trans ansoral surg urgical cal rese resect ction (T (TOR ORS) S) RANDOMIZE with ipsilateral selective neck dissection Final P Final Pathol tholog ogy: y: 60 Gy in 6 weeks 60 Gy in 5 weeks 2.5 cm tumor, no PNI/LVI Cisplatin 40 mg/m 2 weekly (no chemotherapy) 4/25 +LN, largest 3 cm with 1 mm extra-nodal extension Clear margins (> 5 mm) 44 44% % of of RTOG 1 OG 10-1 -16 popula population on eli eligible. Clos Closed t to accru accrual. Number er o of Po Positiv sitive No Nodes is s is STAGING ST Superior t Sup to L Lymph N Node de Ratio and A Rati and AJCC CC N N Stagi Staging g for r Overall Survival AJCC 7 th Ed. AJCC 8 th Ed. Progno nosi sis o s of Surgically rgically Tr Treated H HNSCC pT2 N2b M0 stage IVA pT2 N1 M0 stage I Roberts et al., Cancer 2016 AJCC 8 th ed. Pathological nodal stage: p16+ oropharynx • pN1 pN1: 4 or fewer involved nodes SEER analysis 12,437 patients • pN2 pN2: More than 4 involved nodes treated 2004-2012 Overall Survival • pN3: … pN3: … no pN3 f no pN3 for r p1 p16+ 6+ 4
3/7/2017 Question 1.2 ST STAGING • 2.5 cm tumor, no PNI/LVI AJCC 7 th Ed. AJCC 8 th Ed. • 4/25 +LN, largest 3 cm with 1 mm extra-nodal extension pT2N2bM0 stage IVA pT2N1M0 stage I • Clear margins (> 5 mm) What adjuvant therapy would be recommended? Clinical Stage Grouping: p16+ 1. Concurrent chemoradiation with CDDP 100 mg/m 2 Q3 wks oropharynx 8 th Ed. 7 th Ed. 2. Standard radiation therapy alone (60-66 Gy) pN0 pN0 pN1 N1 pN2 pN2 pN3 N3 pN0 pN0 pN1 N1 pN2 pN2 3. Dose de-escalated radiation alone (50 Gy) pT0 pT0 pT0 pT0 4. None/observation III III IVA IV IVB VB I I I II pT1 pT1 pT1 pT1 I III III IVA IV IVB VB I I I I II pT2 pT2 pT2 pT2 II II III III IV IVA IVB VB I I I I II pT3 pT3 pT3 pT3 III III III III IVA IV IVB VB II II II II III III pT4 pT4 II II II II III III pT4a pT4a IVA IV IVA IVA IV IVB VB ECOG 3311: Phase II Randomized Trial of TORS EORTC 22931 / RTOG 9501 Combined Analysis Followed by Low-Dose or Standard-Dose IMRT Bernier et al., Head Neck 2005 in Resectable p16+ Locally Advanced OPSCC Lo Low Ri w Risk: Observation pT1-2N0-1 Margin ≥ 3 mm R Int Intermed rmediate: A IMRT N p16+ OPSCC Margin < 3mm 50 Gy / 25 Fx D TORS + Neck ≤ 1 mm ECE O cT1-3, N1-2b Dissection pN2a-b M (No T1N1) PNI I Z LVI IMRT E 60 Gy / 30 Fx Unknown: Unk n: pN2c or N3 High Hi gh Ri Risk sk: Pos. Margins IMRT 66 Gy / 33 Fx CDDP 40 mg/m 2 Qwk > 1 mm ENE E3311 INV v.08/15/16 ≥ 5 +LN ecog-acrin.org 5
3/7/2017 Question 1.3 • The patient receives adjuvant cisplatin chemoradiation • 6 months follow-up: new back pains Systemic therapy choice? • PE PET-CT CT: 2 : 2 li liver m r metas tastases, ases, no bo bony metastasis tastasis 1. Docetaxel • MRI Brain: no evidence of intracranial metastases 2. Cisplatin/5FU/Cetuximab • KPS 80% 3. Nivolumab 4. Pembrolizumab Nivolumab for Recurrent Squamous-Cell EXTREME Carcinoma of the Head and Neck R. L. Ferris et al., NEJM, Nov. 2016 N = 442 361 patients Untreated recurrent or metastatic • squamous-cell carcinoma of the head Progression within 6 months of • and neck platinum chemotherapy No brain metastases • 220 pts: cisplatin 100 mg/m2 or Randomized to: • carboplatin AUC 5 mg/ml-min, plus – nivolumab (3 mg/kg Q2wks) fluorouracil 1000 mg/m2 x 4 days x 6 cycles – other single agent therapy (MTX, docetaxel, cetuximab) 222 pts: same chemotherapy plus 1 year 1 ar OS 36% vs. 1 OS 36% vs. 16.6% .6% • cetuximab 400 mg/m2 loading then Grad Grade 3-4 3-4 toxic xicity: 13% vs. % vs. 35% 35% 250 mg/m2 weekly until disease • progression Greater effect if PD-L1 ≥ 1% • (non-significant) Vermorken et al, N Engl J Med 2008; 359:1116-1127 6
Recommend
More recommend