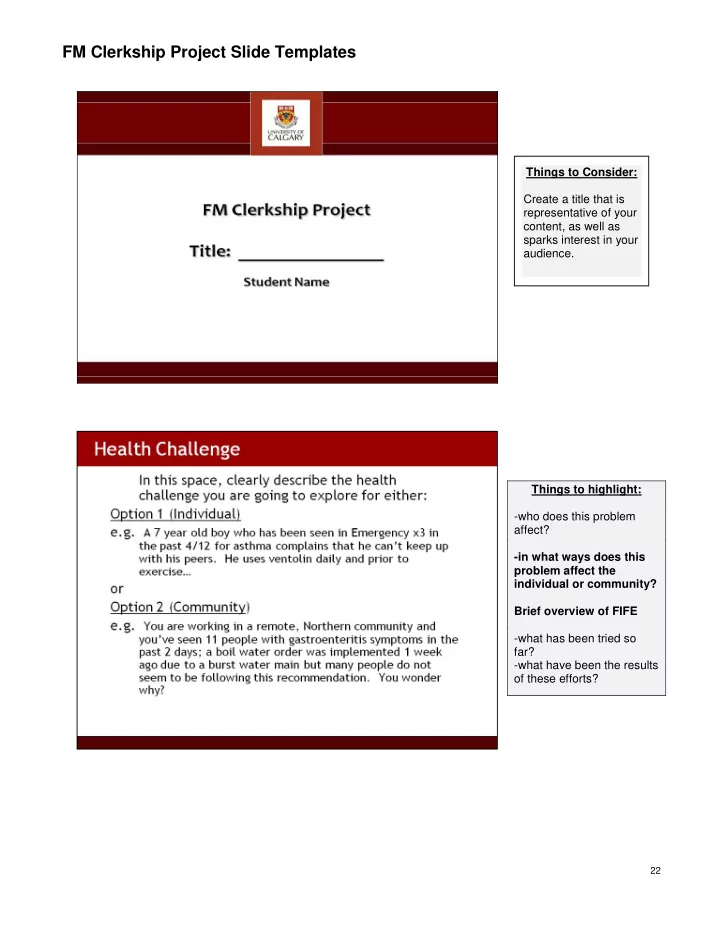
FM Clerkship Project Slide Templates Things to Consider: Create a title that is representative of your content, as well as sparks interest in your audience. Things to highlight: -who does this problem affect? -in what ways does this problem affect the individual or community? Brief overview of FIFE -what has been tried so far? -what have been the results of these efforts? 22
Things to Consider: - PICO structure to refine your question ( P atient/ P opulation or P roblem, I ntervention, C omparison intervention, O utcomes) -searching databases and journals that are relevant to Family Medicine , Population Health, and the identified health challenge -see http://libguides.ucalgary .ca/family_med Appendix 5 below -Level of available evidence (Sackett‟s criteria 1-5) and critical appraisal of resources used Things to Consider: - Patient-Centred Clinical Method “PCCM”(Stewart et al, 2003) - Proximal factors in context : family, financial security, education, employment, leisure, and social support Distal factors in context: community, culture, economics, healthcare systems, socio-historical, geography, the media and ecosystem health -more thorough exploration of FIFE 23
Things to Consider: Any features of the community which (may) have an impact on the Health Challenge, creating a barrier or a bridge to wellness. e.g. -availability of indoor recreation space, including hours, universal accessibility (wheelchair ramps), cost -community bylaws regarding snow clearance if health challenge -outdoor air quality related to agriculture or other industry Things to consider: -revisiting your initial literature search (“What‟s known in the Univ erse”) and apply what you‟ve learned about your patient‟s key contextual features to refining and/or re-directing your search. -exploring government documents; community medicine, anthropology or sociology literature; community-based resources 24
Things to Consider: - ”benefits” may include reduced mortality, preserved function, improved quality of life, etc… - ”drawbacks” may include financial cost, adverse effects of medications, time commitment, etc… -if available and relevant to your individual or community health challenge, include quantitative expressions of benefit/drawbacks, e.g. NNT, Absolute risk reduction Things to Consider: - this should be done at a follow- up visit, after you‘ve searched the literature -PCCM identifies 3 Key steps to Finding Common Ground with patients: 1. ―Defining the problem‖ in terms that include both the disease process and patient‟s illness experience 2. ―Establishing the goals and priorities of management‖ putting the patients values at the forefront 3. ―Identify ing the roles to be assumed by both patient and doctor‖ ie. who will do what and what to do if the unexpected happens (safety nets) For a Community Health Challenge, outline specific interventions that you can justify to your peers that make sense for the health challenge and community context you‟ve presented and if possible, discuss these with someone representative of the community under study. 25
Some concepts to consider when doing your project… A. Narrative Approach We all use stories to make sense of our experiences. The more stressful the experience, the more we need to tell and re-tell our story. When physicians listen intently, by using reflective methods and empathy, they build the patient‟s trust and can begin the process of healing. Phrases that invite patients to tell their stories, such as “Tell me, from when this first started, what you‟ve been noticing…”, give pati ents the opportunity to provide detailed information that naturally integrates the description of the disease process and their unique illness experience. A careful and active listener, who is skilled in this approach, can efficiently gather the information needed to understand “the whole person” (see below) while developing strong rapport with their patient. An excellent example of a patient‟s narrative can be found at: http://www.vancouversun.com/health/Cancer+best+thing+that+ever+happened/2752354/story.html B. Understanding the ―Whole Person‖ -requires integration of 3 concepts: 1.) Disease Process -the biophysical nature of the health challenge is revealed by conventional clinical methods which focus on History, Physical Exam, lab tests and other investigations. AND 2.) Illness Experience - “FIFE”, an approach used in pre -clerkship Med Skills, can be used to think about an individual‟s unique experience of illness, FIFE: Feelings about being ill (including Fears) Ideas about the illness- the patient‟s explanatory model and the meaning of the illness Functional impact of the illness Expectations of the visit/physician (see Calgary-Cambridge Guides 1 and 2 (CCG), Appendix 2 and 3) AND Context : 3.) - many elements of a patient‟s context may be revealed by a conventional “Personal Social History”, including occupation, home situation and habits. The ―Patient -Centred Clin ical Method‖ (PCCM) (Stewart et al, 2003), pioneered in the 1980‟s and ever -evolving, encourages a richer understanding of an individual‟s or community of patients‟ “context” . This typically requires several visits over time (continuity of care really hel ps here…) and preceptors may be able to provide much of this detail. . The PCCM recognizes the key role of: a. Proximal factors in context include personality, current life stage, past experiences, spirituality, family dynamics, financial security, education, employment, leisure, and social support. b. Distal factors in context include community, culture, economics, healthcare systems, socio- historical, geography, the media and ecosystem health. For further details of PCCM: 1. Appendix 4 of Core Doc 2. “Patient - Centred Medicine: transforming the clinical method” M Stewart et al, 2003 on reserve in the Health Sciences Library; a useful excerpt from this text is at http://www.uwo.ca/fammed/ian/patcen.htm 3. Patient-Centred Interviewing Parts I to III http://www.ncbi.nlm.nih.gov/pmc/issues/162784/ 4. “Tell me about yourself: The Pat ient- Centered Interview” F Platt et al, Ann Intern Med. 2001; 134: 1079-85 http://www.annals.org/content/134/11/1079.full.pdf+html 26
Recommend
More recommend