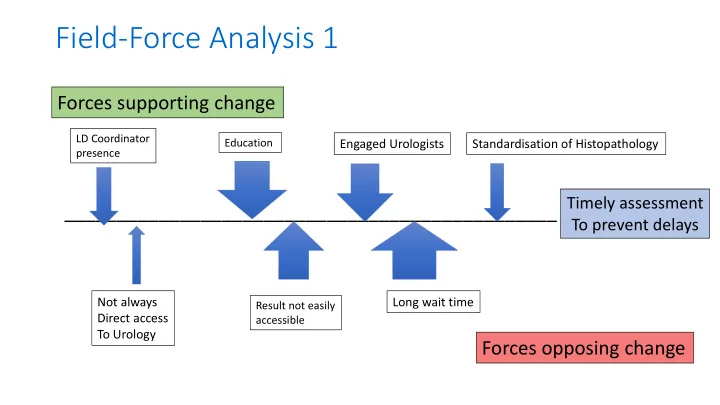
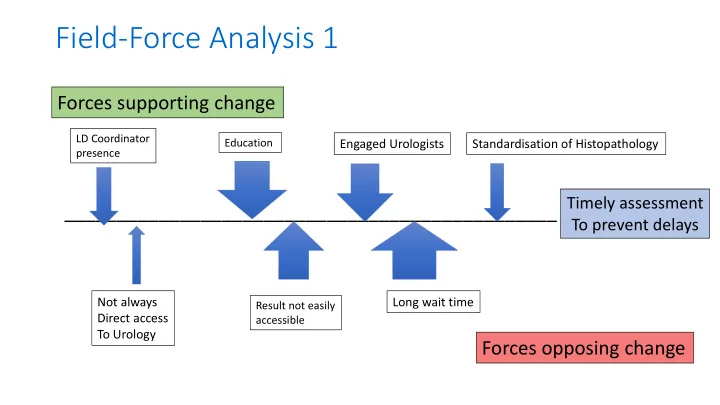
Field-Force Analysis 1 Forces supporting change LD Coordinator Education Engaged Urologists Standardisation of Histopathology presence _______________________________________________ Timely assessment To prevent delays Not always Long wait time Result not easily Direct access accessible To Urology Forces opposing change
Field-Force Analysis 2 Forces supporting change Timing of More LD coordinator Peer support One stop investigation Referral centre LD Nephrology Lead time clinics _______________________________________________ Effective streamlined Donor care pathway Timing of suspension Lack of I.A Funding Lack of Mental LD Donor coordinator asked to From DD list within admin Health support Provide recipient o/c pathway Support to Forces opposing change process screening
Field-Force Analysis 3 Forces supporting change Statement to National H&I Patient record. interpret results/ Good communication between Names/linked Diff units working up, 2 nd TX Standardisation of Engage H&I labs tissue typist Referring and transplant centres Standardisation of report XM in UK _______________________________________________ Prompt identification Of best donor Competing priorities IT issues to Standardisation Capacity/ Cost For lab (deceased donor) Of practice/timing view results Staffing Of tissue typing for sharing Scheme matches Forces opposing change
Field-Force Analysis 4 Forces supporting change Patient will Financial Professional Efficiency input die goodwill _______________________________________________ Address 18-month pathways Financial Available LDK Guidelines (???) lessons input staff Forces opposing change
Field-Force Analysis 5 Forces supporting change Good Culture – 1 stop clinic or MDT pre-book/reserve tests communication very keen Less visits _______________________________________________ Resources for Finances Isotope GFR Timing of e.g. CT surgeons MDT Forces opposing change
Field-Force Analysis 6 Forces supporting change Maximising Universal Clinician Joint education/ Consistent care contact time RRT referral attitude Team work _______________________________________________ Start core donor pathway earlier Mutually Divided/specific Clinician exclusive responsibility attitudes pathways Forces opposing change
Field-Force Analysis 7 Forces supporting change Transplant Good working Funding/time first relationships _______________________________________________ Speed up external/ internal referral Altruistic donors/ Healthy Funding/time Whole hospital education Mental Health individual communication direct benefit Forces opposing change
Field-Force Analysis 8 Forces supporting change Donor Donor and recipient Health screen Letters back for healthcare Virtual cross match seen together on first visit HLA report questionnaire _______________________________________________ Better communication – HCP/Recipient/Donor Report back needed Timing for Antibodies leads Communication lines between Delays in recipient in plain English To delays in tissue typing Feeder units to transplant centres work up – easy to understand results back Forces opposing change
Field-Force Analysis 9 Forces supporting change 3 monthly Length of time Lab availability & recipient antibody For cross match Cheaper equipment screening result Speeding up _______________________________________________ Initial cross match Lots of samples May need extra Remembering to take Patients may being taken in wrong screen for sensitized screening sample need extra visit containers recipients every 3 months if virtual not enough (reminder required Forces opposing change From lab)
Field-Force Analysis – Blank Template Forces supporting change Factor 2 Factor 3 Factor 1 Factor 4 Factor 5 _______________________________________________ The proposed change Factor 2 Factor 3 Factor 4 Factor 5 Factor 1 Forces opposing change
Recommend
More recommend