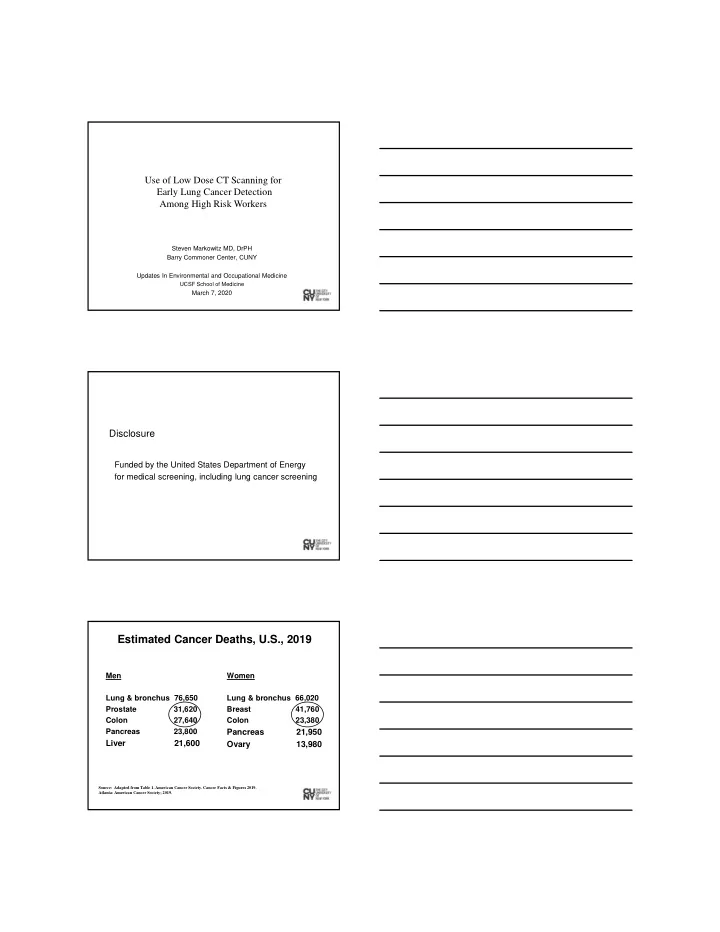
Use of Low Dose CT Scanning for Early Lung Cancer Detection Among High Risk Workers Steven Markowitz MD, DrPH Barry Commoner Center, CUNY Updates In Environmental and Occupational Medicine UCSF School of Medicine March 7, 2020 Disclosure Funded by the United States Department of Energy for medical screening, including lung cancer screening 2 Estimated Cancer Deaths, U.S., 2019 Men Women Lung & bronchus 76,650 Lung & bronchus 66,020 Prostate 31,620 Breast 41,760 Colon 27,640 Colon 23,380 Pancreas 23,800 Pancreas 21,950 Liver 21,600 Ovary 13,980 Source: Adapted from Table 1. American Cancer Society. Cancer Facts & Figures 2019. Atlanta: American Cancer Society; 2019.
Lung cancer mortality remains high, because most cases are diagnosed at advanced stages when successful treatment is limited. Occupational lung cancer 1. Contributes to 10% to 15% of lung cancer ~10,000 to 20,000 deaths annually in U.S. 2. Accounts for 40% to 60% of all occupational cancers 3. Main exposures: asbestos, silica, diesel exhaust, welding fumes Rushton 2010; Labreche 2019; Steenland. AJIM, 2005 Global Burden of Disease Study, 2015 525,000 annual lung cancer deaths due to 9 occupational lung carcinogens GBD 2015 Risk Factors Collaborators, Lancet 2016
Total chemicals used in U.S. and evaluated by IARC 86,000 chemicals in EPA TSCA Inventory ~ 1,000 evaluated by IARC Agents Classified by the IARC Monographs, Volumes 1-125 Group 1 Carcinogenic to humans Group 2A Probably carcinogenic to humans 120 83 Group 3 Not classifiable as to its carcinogenicity to 500 humans 314 Group 2B Possibly carcinogenic to humans IARC Lung Carcinogens Group 1 Group 2A Agent Arsenic and inorganic arsenic Biomass fuel (primarily wood), compounds indoor emissions from household Asbestos (all forms) combustion of Beryllium and beryllium compounds Bitumens, occupational exposure to Bis(chloromethy)ether; chloromethyl oxidized bitumens and their methyl ether (technical grade) emissions during roofing Cadmium and cadmium compounds alpha-Chlorinated toluenes and Chromium(VI) compounds benzoyl chloride (combined Coal, indoor emissions from household exposures) combustion Cobalt metal with tungsten carbide Coal tar pitch Creosotes Engine exhaust, diesel Diazinon Nickel compounds Hydrazine Outdoor air pollution Painting Particulate matter in outdoor air pollution Plutonium Radon-222 and its decay products Silica dust, crystalline Soot Tobacco smoke, secondhand Welding fumes IARC Monographs Volumes 1-125 X-radiation, gamma-radiation
IARC Lung Carcinogens identified since 2010 (*) Group 1 Group 2A Agent Arsenic and inorganic arsenic Biomass fuel (primarily wood), compounds indoor emissions from household Asbestos (all forms) combustion of* Beryllium and beryllium compounds Bitumens, occupational exposure to Bis(chloromethy)ether; chloromethyl oxidized bitumens and their methyl ether (technical grade) emissions during roofing* Cadmium and cadmium compounds alpha-Chlorinated toluenes and Chromium(VI) compounds benzoyl chloride (combined Coal, indoor emissions from household exposures) combustion Cobalt metal with tungsten carbide Coal tar pitch Creosotes Engine exhaust, diesel* Diazinon* Nickel compounds Hydrazine* Outdoor air pollution Painting Particulate matter in outdoor air pollution* Plutonium Radon-222 and its decay products Silica dust, crystalline Soot Tobacco smoke, secondhand Welding fumes* X-radiation, gamma-radiation In occupational medicine, have we had any opportunity to arrest and cure lethal occupational diseases? Screening for Lung Cancer
Why prioritize blue collar workers for lung cancer screening? 1. Exposed to lung carcinogens at work. 2. Smoke at high rates. 3. Workplace as a basis to inform and screen. Prevalence of Cigarette Smokers by Occupation, United States, 2012 ‐ 2014 30 27% 25% 25 21% 20 17% Prevalence (%) 15 12% 10% 10 5 0 Management, Others Sales and Office Service Production, Construction, Business, Science, Transportation, Maintenance, and and Arts and Material Natural Resources Moving Source: Syamlal G. J Occup Environ Med, 2016. SOC high-level aggregation codes are used. The majority of lung cancers in the U.S. occur among former smokers.
Synergy in Risk of Lung Cancer Tobacco and Occupation • Asbestos • Silica • Arsenic • Radon Tobacco and Occupation Screening for Lung Cancer
1970’s-1980’s Failure of CXR and sputum cytology RCT’s to show lung cancer mortality reduction (Mayo Clinic, MSKCC, and John Hopkins) Claudia Henschke MD David Yankelevitz MD Early Lung Cancer Action Project Henschke et al. Lancet 1999 ELCAP (1992 ) Screened 1,000 smokers, > 60 years old, > 10 pack-years Detected 27 lung cancers (2.7%) on baseline scan 23/27 (85%) were Stage I lung cancer Henschke et al. Lancet 1999
Lung cancer: usual stage at diagnosis Stage Distribution for Lung Cancer, U.S., 2009-2015 CA: A Cancer Journal for Clinicians, Volume: 70, Issue: 1, pp: 7-30, 2020, National Lung Screening Trial 2000 → National Cancer Institute National Lung Screening Trial (NLST) • Three annual screening rounds (2002 ‐ 2004) up to 7.4 years follow ‐ up • Largest RCT to date; > 53,000 people 33 major medical centers • $250 million cost • ~26,700 in each arm: LDCT versus CXR
NLST eligibility criteria • 55 ‐ 74 y.o. • ≥ 30 pack years smoking history • quit within past 15 years Why these screening criteria? To identify a large high risk group that, if low dose CT scan is effective, is likely to show an appreciable reduction in death from lung cancer in a few years. NLST results, 2011 Screening yield: T0: 1% had lung cancer T1: 0.68% had lung cancer T2: 0.88% had lung cancer
NLST results Lung cancer stage distribution (three CT screening rounds combined) Stage 1: 63.0% Stage 2: 7.2% Stage 3: 17.0% Stage 4: 12.8% NLST Research Team. NEJM 2011 NLST results Lung cancer mortality reduction = 20% in CT versus CXR arm Overall mortality reduction = 6.7% NELSON Trial (Dutch ‐ Belgian trial) • Four screening rounds at varied intervals (1 year, 2 years, 2.5 years) up to 10 years follow ‐ up • 2 nd largest RCT to date; ~15,800 people • ~6,600 in each arm: LDCT versus No imaging De Koning et al. NEJM. January 29, 2020
NELSON Eligibility criteria • 50 ‐ 74 y.o. • > 15 cigs/day for > 25 years or > 10 cigs/day for > 30 years (15 to 18.75 pack ‐ years) • quit within past 10 years De Koning et al. NEJM. January 29, 2020 NELSON, 2020 Screening yield: T0: 0.9% had lung cancer T1: 0.7% had lung cancer T2: 1.1% had lung cancer T3: 0.8% had lung cancer NELSON results, 2020 Lung cancer stage distribution (in men) (CT ‐ detected cancers; four CT screening rounds combined) Stage 1: 58.6% Stage 2: 9.3% Stage 3: 16.3% Stage 4: 9.4% (unknown: 6.4%) NLST Research Team. NEJM 2011
NELSON Results, 2020 Lung cancer mortality reduction 24% in men and 33% in women in CT versus control arm De Koning et al. NEJM. January 29, 2020 USPSTF Recommendation, 2013 Endorsed annual LDCT screening for lung cancer Eligibility criteria: 55 ‐ 80 y.o. ≥ 30 pack years smoking history quit within past 15 years Occupation? Medicare (CMS), Decision memo, 2015 Eligibility criteria: 55 to 77 years old > 30 pack ‐ years smoking < 15 years since smoking cessation
Medicare (CMS), Decision Memo, 2015 Requires: • Smoking cessation advice • Shared decision ‐ making clinical visit • National registry of CT data Occupation? Eligibility criteria Age- and smoking-based risk vs. Aggregate risk
2014 National Comprehensive Cancer Network (NCCN) 40 NCCN Criteria #1: NCI/Medicare criteria Criteria #2: > 50 years old > 20 pack ‐ years smoking 1 other risk factor for lung cancer : total risk > 1.3%, 6 years Wood. NCCN, 2018 NCCN Criteria #1: NCI/Medicare criteria Criteria #2: > 50 years old > 20 pack ‐ years smoking 1 other risk factor for lung cancer: total risk > 1.3%, 6 years Wood. NCCN, 2018
NCCN Criteria #2 Other risk factors for lung cancer • Occupational exposures (asbestos, silica, diesel exhaust) • Family history • COPD, other respiratory diseases • Radon exposure Lung cancer risk calculators MSKCC: age, gender, pack-years, #quit-years, asbestos AATS: age, gender, BMI, FH, EM education, pk-yrs, quit- years, asbestos ALA, ATS: age, pk-years, #quit-years 44 Occupational studies
Worker Health Protection Program Early Lung Cancer Detection 1993 Defense Authorization Act Section 3162 Required DOE to: “establish and carry out a program for the identification and ongoing medical evaluation of current and former Department of Energy employees who are subject to significant health risks as a result of exposure of such employees to hazardous or radioactive substances during such employment” Department of Energy Worker Health Protection Program INL CA Labs Mound Fernald NTS Portsmouth GDP Paducah GDP ORNL/Y-12 WIPP K25 GDP City University of New York United Steelworkers, Atomic Trades and Labor Council
Features • Former nuclear weapons workers • Non-urban areas • Age, smoking history, occupational history • Centralized CT reading • Community-based diagnosis and treatment Worker Health Protection Program ELCD 2000 - present Screened ~14,000 workers >50,000 CT scans WHPP ELCD Excellent participation! Enrollment 69% (n=5,121, 2014-2018) Show rate 89% (n=33,807 scans, 2007-2018)
Recommend
More recommend