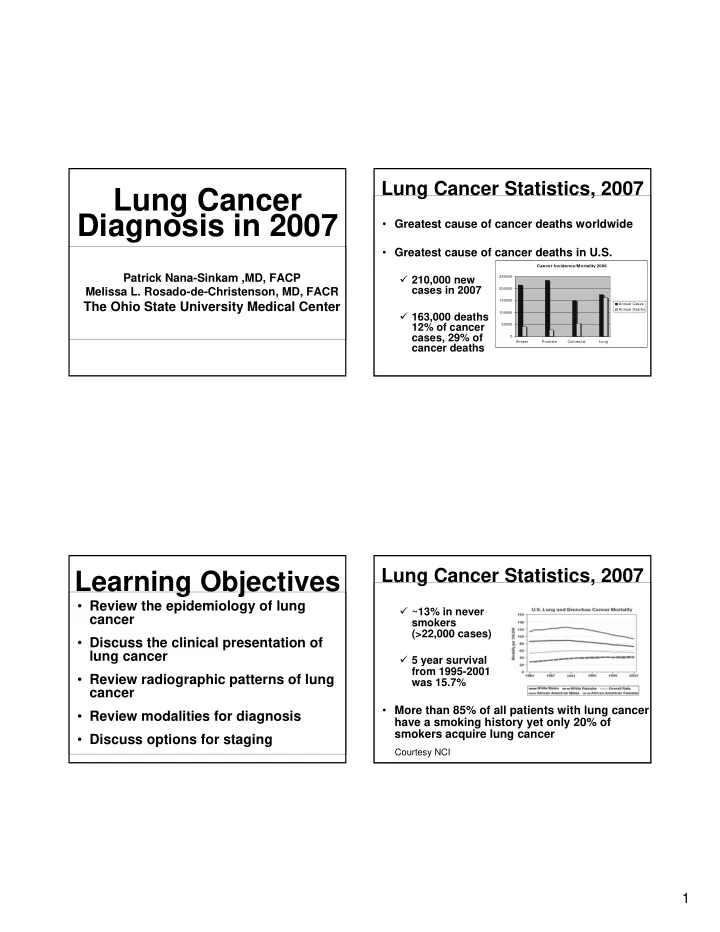
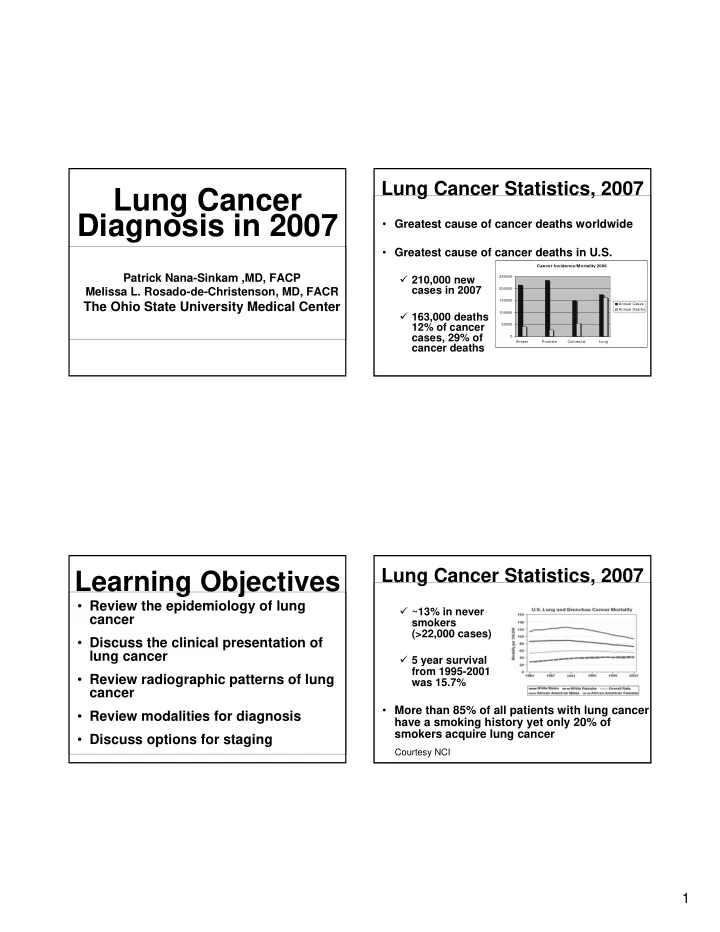
Lung Cancer Statistics, 2007 Lung Cancer Diagnosis in 2007 • Greatest cause of cancer deaths worldwide • Greatest cause of cancer deaths in U.S. Cancer Incidence/Mortality 2006 Patrick Nana-Sinkam ,MD, FACP � 210,000 new 250000 cases in 2007 Melissa L. Rosado-de-Christenson, MD, FACR 200000 150000 The Ohio State University Medical Center Annual Cases Annual Deaths � 163,000 deaths 100000 12% of cancer 50000 cases, 29% of 0 Breast Prostate Colorectal Lung cancer deaths Lung Cancer Statistics, 2007 Learning Objectives • Review the epidemiology of lung � ~13% in never cancer smokers (>22,000 cases) • Discuss the clinical presentation of lung cancer � 5 year survival from 1995-2001 • Review radiographic patterns of lung was 15.7% cancer • More than 85% of all patients with lung cancer • Review modalities for diagnosis have a smoking history yet only 20% of smokers acquire lung cancer • Discuss options for staging Courtesy NCI 1
Gender Differences Risk Factors In Lung Cancer • Tobacco use • Women with lung cancer have been • Chronic lung disease shown to • Genetic predisposition � 1. Have smoked less • Radon • Asbestos � 2. Be younger • Air pollution � 3. Be 2-3 times more likely to have never � Arsenic smoked and � Chromates � 4. Get adenocarcinoma more often than � Chloromethyl ethers males � Nickel Gender Differences In Lung Cancer • Biological Differences: nicotine 20% metabolism, cytochrome p-450 enzyme Adenocarcinoma 35% system, DNA adduct levels, hormonal Squamous cell effects Large cell Small Cell • Hormonal Differences: role of estrogen 20% Other 5% • Genetic Differences: higher p53 mutations 20% among women with non-small cell carcinoma, higher K-ras mutations • Occupational: high incidence in cashiers, waitresses, orderlies, nurse’s aides 2
Pathology Lung Cancer: Lung Cancer Screening Non-Small Cell • Based on the principle that early diagnosis Squamous-cell carcinoma (~20%) allows for more definitve therapy • Studies in the 70’s and 80’s did not support • Most commonly found in men screening • Closely correlated with smoking (dose • Low dose CT (LDCT) is most promising dependent) modality • Two randomized trials are under way: • Tends to spread locally National Lung Screeing Trial (50,000 • More readily detected in sputum patients) and NELSON trial (16,000 patients) • Highly expressed genes encoding proteins • Currently screening is not recommended with detoxification/anti-oxidant properties Treatment “First Pathology Lung Cancer: Non-Small Cell Principles” • Diagnosis Adenocarcinoma (~35%) � Adequate biopsy sample • Most common type of lung cancer • Stage in women and non-smokers � Stage determines treatment • Lesions are usually peripheral • Treatment • Worldwide incidence increasing � In NSCLC, surgery is the cornerstone of treatment � In SCLC, chemotherapy is the cornerstone 3
Pathology Lung Cancer: Pathology Lung Cancer: Non-Small Cell Non-Small Cell Adenocarcinoma (~35%) Large-cell carcinoma (5-10%) • Highly expressed genes encoding small • Very primitive, undifferentiated cells airway-associated and immunologically related proteins • Lesions are usually peripheral • K-ras mutations frequently reported • High tendency to metastasize • Bronchoalveolar carcinoma is a subtype Small-cell lung cancer Bronchoalveolar Cell (SCLC) Carcinoma • Epidemiology: 2-9% of all lung cancers,F>M • 13-20% of all lung cancers • Clinical presentation: solitary lesion: often • Smokers, more prevalent in women than asymptomatic, consolidation or bilateral men disease: cough, chest pain, dyspnea, hemoptysis, weight loss, bronchorrhea (~5%, late stage) • Aggressive (brain evaluation required) • Radiographic: solitary, spiculated, peripheral nodules (43%), consolidation (30%), diffuse (27%) 4
Small-cell lung cancer Initial Workup of (SCLC) Suspected Lung Cancer • Initially chemosensitive (Platinum based Thorough History and Physical therapy better than non platinum based) constitutional symptoms becoming resistant. Should receive localizing findings concurrent chemo/rads signs of metastatic disease • Prophylactic cranial irradiation should be offered (ACCP) Serum chemistries Imaging • Surgery in limited disease? LFTs CT chest through adrenals CBC Brain imaging based on H +P Bone imaging based on H +P SVC Syndrome Clinical presentation ~20% operable at • Dyspnea presentation • Facial swelling or head fullness, cough, arm edema, cyanosis, facial plethora Metastatic spread Primary lesion Intrathoracic spread Bone pain • Lung cancer is the Cough Pleural effusion Neurological Dyspnea most common Hoarseness Weight loss (liver) Hemoptysis Pericardial effusion Fatigue malignant cause of Chest pain SVC syndrome Nodes (supraclavicular the SVC syndrome (2-4% of lung cancers) Focal wheeze fossa) Up to date, 2007 5
SVC Syndrome Superior Sulcus Tumors • 20% of small cell • DX: Percutaneous needle bx (+) in > 90% • SVC obstruction is • Brain imaging a strong predictor essential since most of poor prognosis common site of distal in patients NSCLC recurrence with a median survival of only • MRI may be very five months in helpful in assessing for brachial plexus or one series vertebral body involvement • Unless there is airway compromise, • TX: Preop chemoradiation/resection/chemo establish histology first Up to date, 2007 Paraneoplastic Syndromes Superior Sulcus Tumors System Syndrome Cell type • < 5% Endocrine Hypercalcemia Squamous cell SIADH Small cell • Apex of the lung Cushing’s Small cell/carcinoid Neurological Lambert-Eaton Small cell • Adenocarcinoma is Polyneuropathy Autonomic predominant cell type Neuropathy in some series Skeletal Hypertrophic Squamous cell and Osteoarthropathy Adenocarcinoma • SX: shoulder, arm, Clubbing scapular pain, parasthesia, weakness, 14-50% Collagen vascular Horner syndrome Renal Metabolic Up to date, 2007 Cutaneous Hematological 6
Learning Objectives The Diagnosis of Lung Cancer 1. To recognize typical imaging manifestations of lung cancer including: The Radiologist’s Perspective a. Mass b. Post-obstructive Atelectasis / Melissa L. Rosado-de-Christenson, MD, FACR Consolidation The Ohio State University c. Features of advanced lung cancer The Uniformed Services University 2. To understand the imaging evaluation of patients with pulmonary nodules Imaging Features of Acknowledgements: Lung Cancer AFIP radiology resident classes Pulmonary mass Atelectasis / Consolidation Gerald F. Abbott, MD Pulmonary nodule Mark S. Parker, MD Mediastinal mass (metastatic lymphadenopathy) Peripheral mass with extrapulmonary involvement Diane C. Strollo, MD Metastatic disease 7
Advanced Lung Cancer Advanced Lung Cancer Hematogenous Metastases Mediastinal Mass Advanced Lung Cancer Lung Mass (> 3 cm) Chest Wall Involvement High likelihood of malignancy Well-defined borders Lobular borders Spiculated borders DDX: Infection, benign neoplasia 8
Peripheral Mass Atelectasis / Adenocarcinoma Consolidation Indirect manifestation of malignancy Post obstructive effects of a central neoplasm Reverse S-sign of Golden Indicative of central neoplasm with resultant atelectasis Peripheral Mass Central Mass Adenocarcinoma Squamous Cell Carcinoma 9
Atelectasis Central Mass Squamous Cell Carcinoma Squamous Cell Carcinoma Atelectasis Consolidations in Adults Squamous Cell Carcinoma “Consolidations in adults must be followed to complete radiographic resolution to exclude underlying malignancy. Follow-up chest radiography is recommended six weeks after start of therapy.” 10
Solitary Pulmonary Solitary Pulmonary Nodule Definition Nodule Imaging Do nothing Benign Rounded opacity that is moderately well marginated and is not larger than 3 cm in diameter Malignant Biopsy or Definitely malignant Linear opacities are not nodules Excision Possibly malignant Clustered nodular opacities are not solitary Irregular opacities at the apices are likely scars / fibrosis Follow-up Ovoid or triangular fissural opacities are likely lymph nodes Indeterminate imaging Solitary Pulmonary Nodule Solitary Pulmonary Nodule Intrapulmonary Lymph Node Characterization Nodule density Nodule morphology Nodule attenuation Nodule size / growth 11
Solitary Pulmonary Nodule Solitary Pulmonary Nodule Density - Calcification Spiculation - Emphysema 08/21/07 10/02/07 Solitary Pulmonary Nodule Solitary Pulmonary Nodule Attenuation Morphology Non - solid Part - solid Up to 2/3 malignant Invasive adenocarcinoma 12
Solitary Pulmonary Nodule Fleischner Criteria Attenuation MacMahon et al. Radiology 2005; 237: 395-400. Size Low-risk High-risk < 4 mm No follow up 12 mo follow up 4 - 6 mm 12 mo follow up 6-12, 18-24 mo follow up 6 - 8 mm 6-12, 18-24 mo 3-6, 9-12, 24 mo follow up follow up > 8 mm 3, 9, 24 mo f/u Same dynamic CT, BX Non-solid Part-solid Solitary Pulmonary Nodule Solitary Pulmonary Nodule Size Growth Size Risk < 3 mm 0.2% 4 - 7 mm 0.9% 8 - 20 mm 18% > 20 mm 50% 09/06 12/06 05/07 09/07 5 mm 11 mm 21 mm Midthun et al. Lung Cancer 2003; 41 (Suppl 2): S40 13
Recommend
More recommend