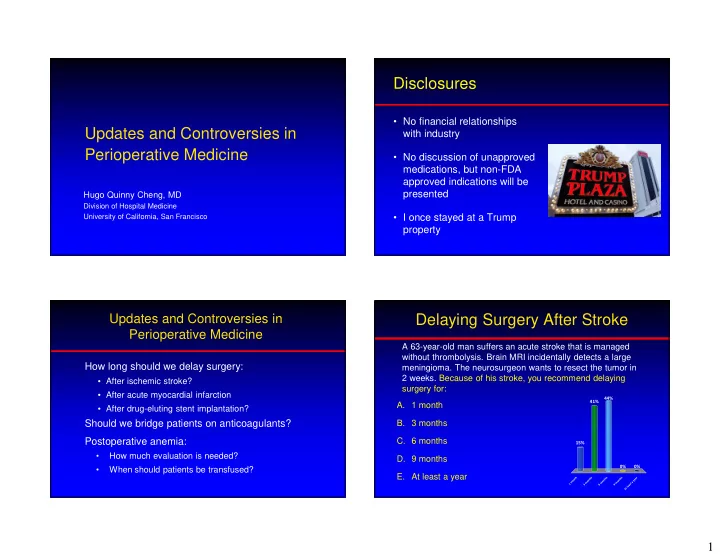
Disclosures • No financial relationships Updates and Controversies in with industry Perioperative Medicine • No discussion of unapproved medications, but non-FDA approved indications will be presented Hugo Quinny Cheng, MD Division of Hospital Medicine • I once stayed at a Trump University of California, San Francisco property Updates and Controversies in Delaying Surgery After Stroke Perioperative Medicine A 63-year-old man suffers an acute stroke that is managed without thrombolysis. Brain MRI incidentally detects a large How long should we delay surgery: meningioma. The neurosurgeon wants to resect the tumor in 2 weeks. Because of his stroke, you recommend delaying • After ischemic stroke? surgery for: • After acute myocardial infarction 44% A. 1 month 41% • After drug-eluting stent implantation? Should we bridge patients on anticoagulants? B. 3 months Postoperative anemia: C. 6 months 15% • How much evaluation is needed? D. 9 months • When should patients be transfused? 0% 0% E. At least a year h s s s r t h h h a n t t t e n n n y o o o o m a m m m 1 s t 3 6 9 a e l t A 1
Delaying Surgery After Stroke Delaying Surgery After Stroke 20% Question: How does time between stroke and surgery MACE Incidence affect the risk of cardiovascular complications? CV Death 15% Ischemic Stroke Danish cohort study of all adults undergoing elective Acute MI 10% noncardiac surgery from 2005-2011: • 7137 patients had prior stroke (1.5% of total cohort) 5% • Outcome: 30-d postop Major Adverse Cardiac Events (MACE): nonfatal MI, ischemic stroke, cardiovascular death • Looked at effect of time since stroke on MACE rate 0% < 3 months 3-6 months 6-12 months > 12 months Time Between Acute Stroke & Surgery Jorgenson ME et al. JAMA 2014; 312:269-277 Delaying Surgery After MI How Long to Wait after CVA? A 63-year-old man suffers an acute myocardial infarction treated without PCI. He was already scheduled for prostate Conclusions: cancer surgery in one month. Because of his recent MI, you recommend delaying surgery for: • Surgery after CVA associated with high CV risk • Risk falls over 9 months, biggest drop after first 3 months A. 1 month 61% Caveats: B. 2 months • Nonrandomized, observational study C. 3 months My take-away: 21% 13% D. 6 months • Delay elective surgery for at least 3 months (up to 9 5% 0% months) if possible E. At least a year h s s s r t h h h a n t t t e n n n y o o o o m a m m m 1 s t 2 3 6 a e l t A 2
Delaying Surgery After Acute MI Delaying Surgery after Acute MI Question: How does time between acute MI and 35% surgery affect the risk of postoperative MI? 30% 30-Day Postop MI 25% 563,842 patients (1999-2004) discharged after hip 20% surgery, colectomy, cholecystectomy, AAA repair, or 15% lower extremity amputation: 10% • 2.9% of cohort had experienced acute MI in prior year 5% • Outcome: 30-day postoperative MI 0% < 30 31-60 61-90 91-180 181-365 Time (days) Between Acute MI & Surgery Livhits M et al. Annals of Surgery 2011; 253:857-63 How Long to Wait after MI? Surgery After Drug Eluting Stent A 75-y.o. man sustains an unstable cervical spine fracture. He had a drug-eluting stent placed 8 months ago Conclusions: for stable angina. The spine surgeon wants to operate, • Surgery within one year of acute MI associated with high but putting him in a halo vest is a less desirable risk of postoperative MI alternative approach. 77% • Risk falls over time; most of the reduction within 2 months What do you recommend? • Trend is similar when only elective surgery considered Caveats: A. Operate now 23% • Nonrandomized, observational study B. Wait 12 months after DES ACC/AHA Guidelines: w S o E D n • Delay elective surgery for at least 2 months r e e t t a f r a e p s O h t n o m 2 1 t a i W 3
Guidelines for Stents & Surgery Effect of Stent Type & Time After Implantation Timing Time of surgery after PCI didn’t matter after first 6 months Guideline Recommendation 20% 6 months Bare Metal Complications Bare Metal Wait minimum 30 days 15% Drug Eluting 10% Drug Eluting Wait minimum 3 months and preferably 6 months 5% 60 120 180 240 300 360 Time between PCI & Surgery Hawn MT et al. JAMA . doi:10.1001/jama.2013.278787 Managing Perioperative Anticoagulation Benefits & Harm of Bridging Perioperative Anticoagulation Two patients on warfarin therapy are scheduled for elective hip arthropasty. You’re asked whether they should receive perioperative bridging anticoagulation (with enoxaparin): � One patient has atrial fibrillation due to hypertension Death or disability from Death or disability from � The other patient has a mechanical AVR � Neither has any other relevant comorbidity thromboembolism perioperative bleeding 44% 34% averted by bridging caused by bridging A. Heparin bridge for AVR only 17% B. Heparin bridge for AF only 5% C. Heparin bridge for both y y h r l l t e n n o h o o t D. Heparin bridge for neither b i R F r e V A o n f A r r o e o o r f g f e d e f g i g e d b r d g i d r i n r i b i b r r b n a n n i p r i a r e a r i H p a p p e e e H H H 4
BRIDGE Trial BRIDGE Trial Patients: Bridged No Bridge • 1884 patients on warfarin for atrial fib or flutter • CHADS-2 score > 1 • Excluded patients with mechanical valve or stroke within Embolic Event 0.3% 0.4% Non-inferior 12 weeks and cardiac & neurologic surgery Intervention: Major Bleeding 3.2% 1.3% NNH = 53 • Randomized to bridging with LMWH or placebo Outcome: Minor Bleeding 21% 12% NNH = 12 • 30-day risk of arterial thromboembolism & bleeding Douketis JD et al. NEJM, 2015; 373:823-33 Douketis JD et al. NEJM, 2015; 373:823-33 BRIDGE Trial for Atrial Fibrillation What About Mechanical Valves? Conclusions: 7% • Bridging did not reduce risk of embolism Thromboembolic 6% Atrial Fibrillation • Bridging increases bleeding risk Risk (annual) 5% Mechanical Valve Caveats: 4% • Few patients with high CHADS-2 score (mean = 2.3) 3% 2% My take-away: 1% • Don’t bridge majority of atrial fibrillation 0% • Carefully consider bridging if stroke risk is very high Without Anticoagulation With Warfarin (CHADS-2 score 5 or 6, rheumatic atrial fibrillation) Ansell J. Chest. 2004;126:204S-233S. Cannegieter, et al. Circulation , 1994 5
Effect of Mechanical Valve Location & Perioperative Anticoagulation: 2012 ACCP Guidelines (9 th Edition) Design on Thromboembolic Risk Valve Location: Atrial Fib. Mechanical Valve Recommendation Aortic RR = 1.0 CHADS 2 = 5-6; Any MVR; older (caged- Bridge with heparin Mitral RR = 1.8 recent CVA; ball or tilting disc) AVR; rheumatic AF recent CVA Valve Design: CHADS 2 = 3-4 Bileaflet AVR plus other ??? Caged Ball RR = 1.0 stroke risk factor(s) Tilting Disk RR = 0.7 CHADS 2 = 0-2 Bileaflet AVR without AF or No heparin bridge Bi-leaflet RR = 0.6 other stroke risk factor Cannegieter, et al. Circulation , 1994 Perioperative Anticoagulation: What About Venous Clots? My Approach after BRIDGE Risk of Recurrent VTE Atrial Fib. Mechanical Valve Recommendation Consider CHADS 2 = 5-6; Any MVR; older (caged- bridging recent CVA; ball or tilting disc) AVR; rheumatic AF recent CVA CHADS 2 = 3-4 Bileaflet AVR plus other stroke risk factor(s) No bridge CHADS 2 = 0-2 Bileaflet AVR without AF or other stroke risk factor Time Since Venous Thromboembolic Event 6
How About Venous Clots? Venous Clots: 2012 ACCP Guideline Retrospective cohort study Risk of Recurrent VTE Recommendation • 1178 patients on warfarin for DVT or PE • Outcome: 30-day recurrent clotting & significant bleeding High Risk: Bridge VTE < 3 months ago; Bridged No Bridge Hazard Severe thrombophilia Ratio Medium Risk: Case-by-case Recurrent VTE 0% 0.2% ns VTE 3-12 months ago; recurrent VTE; decision Bleeding 2.7% 0.2% 17 (4-75) VTE with cancer other thrombophilia Low: No bridge Single VTE > 12 months ago Clark NP et al. JAMA Int Med , 2015; 175:1163 Postoperative Anemia Venous Clots: My Approach You visit a 79-year-old woman on postoperative day #1 after hip fracture repair. You notice her hemoglobin dropped from Risk of Recurrent VTE Recommendation 11.6 g/dL on admission to 8.5 g/dL today. The operative note reports an EBL (estimated blood loss) of 300 mL. Consider bridging High Risk: Which of the following actions is most likely to be useful? or IVC filter VTE < 3 months ago; 40% 37% Severe thrombophilia A. Order labs to rule out coagulopathy Medium Risk: B. Order labs to rule out hemolysis 17% VTE 3-12 months ago; recurrent VTE; C. Recheck CBC; the results are wrong No bridge 6% VTE with cancer other thrombophilia D. No work-up; the EBL is wrong Low: . g . . . . n . l . e . o u . o r m a r w Single VTE > 12 months ago g a e s o h t i s c u l t L u t u s B o e E o r e e e e l h h u l u t r r t ; ; p o o C u t t B s C k - s b r b a k o a c l l e w r e r h e o d d c N r r e O O R 7
Recommend
More recommend