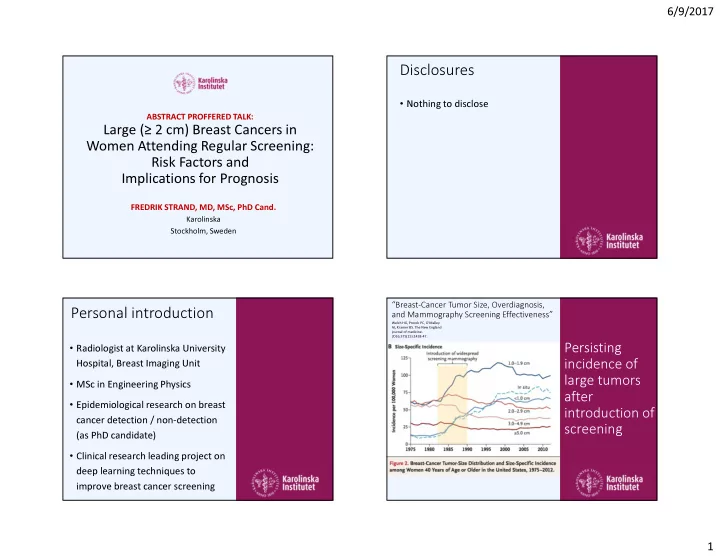
6/9/2017 Disclosures • Nothing to disclose ABSTRACT PROFFERED TALK: Large (≥ 2 cm) Breast Cancers in Women Attending Regular Screening: Risk Factors and Implications for Prognosis FREDRIK STRAND, MD, MSc, PhD Cand. Karolinska Stockholm, Sweden “Breast-Cancer Tumor Size, Overdiagnosis, Personal introduction and Mammography Screening Effectiveness” Welch HG, Prorok PC, O'Malley AJ, Kramer BS. The New England journal of medicine. 2016;375(15):1438-47. • Radiologist at Karolinska University Persisting Hospital, Breast Imaging Unit incidence of large tumors • MSc in Engineering Physics after • Epidemiological research on breast introduction of cancer detection / non-detection screening (as PhD candidate) • Clinical research leading project on deep learning techniques to improve breast cancer screening 1
6/9/2017 Without Larger tumor Screening � � Worse Larger Tumors prognosis Source: Strand, unpublished Large AND Interval Screen-Detected Interval Cancer � � Interval Cancers Worst Worse Non-Attenders prognosis prognosis Source: Strand, unpublished 2
6/9/2017 Methods Authors The Study Analysis Predisposing Fredrik Strand Large (≥ 2 cm) Breast Predisposing risk factors factors known • Comparison: women with ≥ 2 cm vs. < Johanna Holm Cancers in Women 2 cm tumor at diagnosis before diagnosis Mikael Eriksson • Overall and Stratified by detection Attending Regular mode Sven Törnberg Screening: Disease progression Purpose Edward Azavedo • Comparison: Age, BMI and PD Risk Factors and • Stratified by detection mode Improve Per Hall Implications for Prognosis Study population screening Kamila Czene • 2,358 cases of invasive breast cancer, 2001 to 2008 in Stockholm-Gotland Results – predisposing risk factors for large (vs. small) tumor All Screen-detected Interval Cancers n=2,358 n=1,647 n=711 Large cancers 24% 20% 34% Interval cancers 30% 0% 100% Source: Strand, manuscript 3
6/9/2017 Stratified by detection mode Interval Cancer Two different detection PALPATION (mainly) techniques – what hinders MAMMOGRAPHY MAMMOGRAPHY detection Screen-detected Cancer might not be “Post-dinner analysis” – potential confounders the same Education-level � OR change from 2.46 to 2.47 Breast area (size proxy) � OR change from 2.46 to 1.99 Source: Strand, manuscript Probability of tumor remaining Molecular subtype by detection undetected until > 2 cm mode and BMI For Interval High BMI is Cancers – related to tumor size at aggressive detection tumor increases characteristics – sharply with especially for BMI interval cancers Modell- estimated probabilities Source: Strand, Source: Strand, manuscript manuscript 4
6/9/2017 Disease progression = Long-term follow-up local recurrence, distant Does the metastasis or breast cancer death • Disease Progression was defined as association Among women either of local recurrence, distant between BMI with interval metastasis or breast cancer death and adverse cancer - high BMI is tumor • We followed patients from date of diagnosis (2001 to 2008) until the associated with characteristics end of 2013 markedly worse translate into prognosis worse • Possible survival bias since only prognosis? women who were alive at study entry in 2009 and 2010 could be included (however – no bias identified when adjusting for year of study entry or time from diagnosis to study entry) Conclusions Clinical Significance BMI as a predisposing risk factor • BMI increases probability of being Less efficient for women with high BMI What to offer diagnosed with a larger tumor – PALPATION (mainly) especially among interval cancers women with high BMI? Molecular subtype MAMMOGRAPHY MAMMOGRAPHY • Women with high BMI more often have aggressive molecular subtypes Women with high risk of mammographic masking � Supplemental ultrasound or MRI (especially Luminal B and Her2, not so much for basal) Women with high BMI Disease progression More frequent screening � • Women with high BMI more often Also, take breast cancer risk into account experience disease progression (HR 2.0) 5
Recommend
More recommend