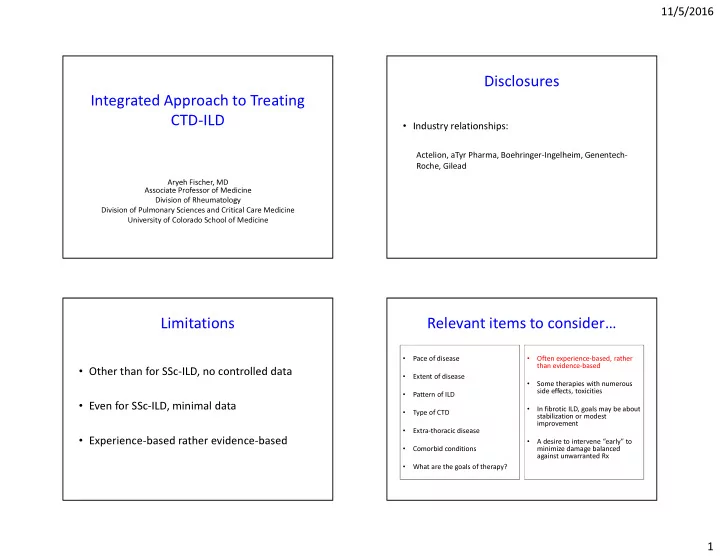
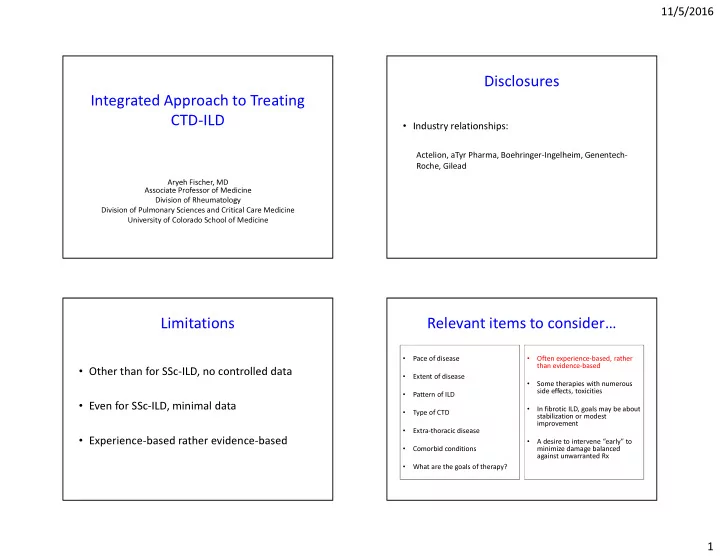
11/5/2016 Disclosures Integrated Approach to Treating CTD-ILD • Industry relationships: Actelion, aTyr Pharma, Boehringer-Ingelheim, Genentech- Roche, Gilead Aryeh Fischer, MD Associate Professor of Medicine Division of Rheumatology Division of Pulmonary Sciences and Critical Care Medicine University of Colorado School of Medicine Limitations Relevant items to consider… • • Pace of disease Often experience-based, rather than evidence-based • Other than for SSc-ILD, no controlled data • Extent of disease • Some therapies with numerous side effects, toxicities • Pattern of ILD • Even for SSc-ILD, minimal data • In fibrotic ILD, goals may be about • Type of CTD stabilization or modest improvement • Extra-thoracic disease • Experience-based rather evidence-based • A desire to intervene “early” to • Comorbid conditions minimize damage balanced against unwarranted Rx • What are the goals of therapy? 1
11/5/2016 Determining impairment Clinical realities for SSc-ILD • Subjective • The majority of SSc patients have ILD – Dyspnea • Clinically progressive disease in ~ 1/3 – Extra-thoracic disease burden Treat: “clinically-significant”, progressive disease • Treatment is not benign (especially CYC and stem cell transplant) • Objective • Effective therapies only associated with stability or modest improvement (SLS I, II, FAST, MMF retrospective data) – PFTs (FVC, DLco) – (Fear of losing ground) – 6MWT • Decisions whether to initiate immunosuppression are individualized – Disease extent by HRCT Predictors of progression? Pulmonary function testing Although not adequate to diagnose ILD… SSc: RA: Men?, CCP?, smokers? – Scl-70 antibody positivity • Ideal modality for assessing progression in those with ILD – Isolated nucleolar ANA Other CTDs: ??? – “Early” disease • Reproducible – Disease extent by HRCT • Relatively inexpensive – Hx of progression • Trend FVC, DLco over time PM/DM: – tRNA synthetase • SSc patients: pulmonary vasculopathy antibodies (e.g. Jo-1, PL-7, – Disproportionate reduction in DLco PL-12, etc.) – MDA-5 – Elevated FVC/DLco ratio (e.g., FVC 80%, DLco 40%) 2
11/5/2016 Six minute walk test General approach to Rx • Measures distance walked, HR, oxygen desaturation Corticosteroids Steroid sparing agent • Reproducible, inexpensive • Effort / coach dependent • Often high dose initially • Azathioprine • MSK disease impacts performance / results • Mycophenolate mofetil • Won’t distinguish ILD from PAH, other causes of • Not a good long term • Cyclophosphamide hypoxia • Tacrolimus option • Cyclosporine • Not ideal for clinical trials, but does aid in assessment in longitudinal care of an individual patient • Rituximab – select cases • Others? Current approach to treatment Non-drug therapy • pulmonary rehab CTD-ILD Idiopathic UIP (ANY pattern) Idiopathic non-UIP • use O2 correctly (IPF) • PH assessments • GERD / aspiration • N-acetylcysteine (NAC)? • Pneumocystis prophylaxis Immunosuppression Clinical trials Immunosuppression • vaccines Lung transplantation • mental health Pirfenidone Nintedanib 3
11/5/2016 Scleroderma Lung Study Scleroderma Lung Study at 2 years CYC Placebo 49% improved 26% improved CYC placebo 51% worsened 74% worsened Tashkin et al 2006 NEJM 354;2655-66 Tashkin et al AJRCCM 2007;176:1026-1034 Fibrosing alveolitis in SSc trial (FAST) Mycophenolate mofetil (MMF) • Very popular for the treatment of CTD-ILD low-dose prednisone, IV CYC x 6 months followed by AZA vs . placebo • Numerous retrospective series in CTD-ILD – mostly scleroderma-ILD BASELINE 1-YR FOLLOW-UP – all with few subjects Rx (n=22) Placebo (n=23) Rx (n=19) Placebo (n=18) P FVC 80 81 83 78 0.08 • MMF in CTD-ILD appears to be: DLCO 53 55 50 52 0.64 – well-tolerated TLC 82 77 80 74 0.61 – associated with preservation of lung function Swigris Chest 2006, Liossis Rheumatology 2006, Gerbino Chest 2008, Zamora Resp Med 2008, Hoyles et al. Arthritis Rheum 2006 Saketkoo Am J Med Sci 2009, Koutroumpas Clin Rheum 2010, Simeon-Aznar Clin Rheum 2011 4
11/5/2016 MMF in CTD-ILD: retrospective study, 125 Plot of mixed-effects model estimates for FVC% in CTD subjects with UIP or non-UIP subjects, diverse CTDs CTD-UIP (n=32; SLBx =15) mixed-effects model estimates for FVC% FVC% CTD-non-UIP (n=93; SLBx=36) weeks before and after MMF initiation weeks before and after MMF initiation Fischer et al. J Rheumatol 2013 Fischer et al. J Rheumatol 2013 MMF start MMF was associated with steroid tapering effects MMF in CTD-ILD • Well tolerated median prednisone dose: at MMF initiation: 20 mg qd • Low rate (10%) of discontinuation after 9-12 months on MMF: 5 mg qd (p<0.0001) • Effective corticosteroid tapering 30 Mean prednisone dose (mg) 28 • Associated with stabilization or improvement in lung 26 RED=RA (n= 18) 24 BLACK=SSc (n=44) 22 function BLUE=PM/DM (n=32) 20 18 GREEN=LD-CTD (n=19) • A longer term option (than CYC) 16 14 12 10 8 • Warrants prospective study 6 4 2 0 -250 -200 -150 -100 -50 0 50 100 150 200 250 weeks before and after MMF initiation Fischer et al. J Rheumatol 2013 Fischer et al. J Rheumatol 2013 5
11/5/2016 SLS II: MMF had fewer adverse events, fewer patients in the MMF arm SLS II prematurely withdrew from the study (20 vs. 32), and time to stopping treatment was shorter in the CYC group (p=0.019) FVC had modest improvement with both MMF and CYC; no significant between- treatment difference Leukopenia! Tashkin et al. Lancet Resp Med 2016 Tashkin et al. Lancet Resp Med 2016 Other options? • Cyclosporine, Tacrolimus • Azathioprine – “ familiar ” – may be particularly – well tolerated effective in patients with myositis – ILD – FAST trial (SSc) – case series suggest • Rituximab 10 subjects enrolled (6 NSIP, 4 UIP), 48 week open label – Refractory myositis-ILD role for variety of • decline in 1, stability in 5 , improvement in 1 – “Rescue therapy” CTD-ILD • 3 withdrew, 1 infusion rxn, 2 deaths (CHF, PNA) Matteson et al, Open J Rheum 2012 6
11/5/2016 Rituximab in chronic CTD-ILD (9 RA, 15 other CTD) RTX for severe refractory ILD (CTD-ILD n=33, HP n=6, misc n= 11) • Median decline in FVC of 14.3% and DLCO of 18.8% in the 6–12 months pre-RTX • Median improvement in FVC of 6.7% (P < 0.01) and stability of DLCO (0% change; P < 0.01) in the 6–12 months post-RTX • 2 developed serious infections (pneumonia) requiring hospitalization • 10 died from progression of underlying ILD, a median of 5.1 (1.2– Spaghetti plot showing trajectories for FVC% over time for each subject (n=24) and 24.5) months after treatment mixed-effects model estimates FVC% over time for the entire cohort Keir et al Respirology 2013 Chartrand et al. Sarcoidosis Vasculitis and DLD 2016 Rituximab in chronic CTD-ILD Should histopathology impact treatment decisions? RA-OP RA-LIP Are these all Non-RA (n=9) RA (n=15) treated the RA-C-NSIP same? aaaaa RA-F-NSIP Figure 3. Spaghetti plot showing trajectories for percentage of FVC% over time for subjects without or with RA RA-UIP Chartrand et al. Sarcoidosis Vasculitis and DLD 2016 7
11/5/2016 Should underlying CTD impact Individual CTD-ILDs treatment decisions? SSc-NSIP • Fischer is totally making it up… MCTD-NSIP Are these all treated the SjS-NSIP same? SLE-NSIP RA-NSIP SSc-ILD Myositis-ILD (Synthetase-ILD) • • MMF >>>>> CYC • Early vs. late disease Window of opportunity • “evolution” from NSIP/OP to fibrotic IP • Not very prednisone- • (they all have fibrotic • Often will use INTENSE corticosteroids responsive (concerns – Pulse dose (1 gram methylpred x 3 days) interstitial pneumonia) – Weekly mini-pulses for renal crisis?) – MMF first line – Early trigger for rituximab • Disease extent • Aspiration, GERD • IVIg for the myositis component • AZA, tacrolimus, cyclosporine • PFT disconnect / PFT • Development of • Long-term Rx needed challenges PH/PAH – FVC/DL ratio 8
11/5/2016 RA-ILD: what’s driving therapy? RA-ILD RA = RED ILD = BLUE • ILD pattern? disease activity disease activity – And these patients get bronchiolitis • I do not extend from PANTHER (but I recognize some do…) time time • AZA is more effective for synovitis than MMF disease activity disease activity • I combine AZA or MMF with biologics • Rituximab is a cool thing to recommend time time Synovitis often impacts Rx DMARDs proven to be effective in RA Biologic Traditional Joint disease ILD • Anti-TNFs • Methotrexate – Infliximab (Remicade) • Sulfasalazine • Complex arena with lots • Not as complex… – Etanercept (Enbrel) • Leflunomide – Adalimumab (Humira) – Corticosteroids of biologic DMARDs • Azathioprine – Golimumab (Simponi) – TNF antagonists – AZA, MMF, CYC… – Certolizumab (Cimzia) • Cyclosporine – IL-6 antagonist • Anakinra (Kineret) • (Gold) – T-cell agents • Abatacept (Orencia) • Rituximab (Rituxan) – B-cell agents • Toclizumab (Actemra) – JAK/STAT inhibitors • Tofacitinib (Xeljanz) 9
11/5/2016 DMARDs proven effective in RA-ILD Controlled trials for RA-ILD Compared to other CTDs, Survival for RA-UIP = IPF UIP is disproportionately represented in RA Other IPF n=536 UIP RA-UIP=24 NSIP Moua and Zamora Martinez et al Respiratory Research 2014 Kim CHEST 2009 10
Recommend
More recommend