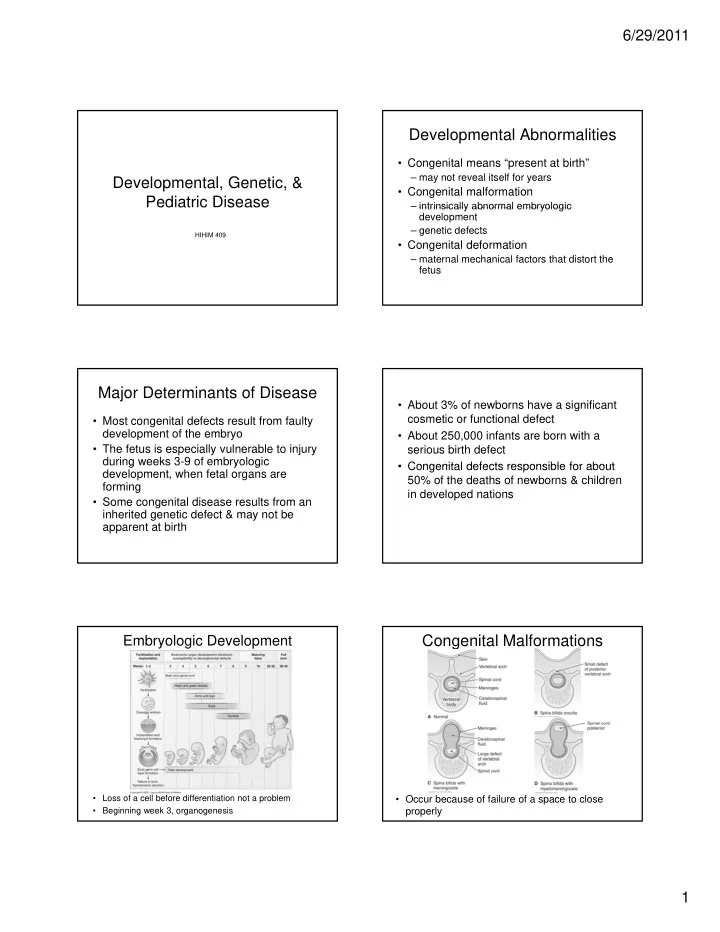
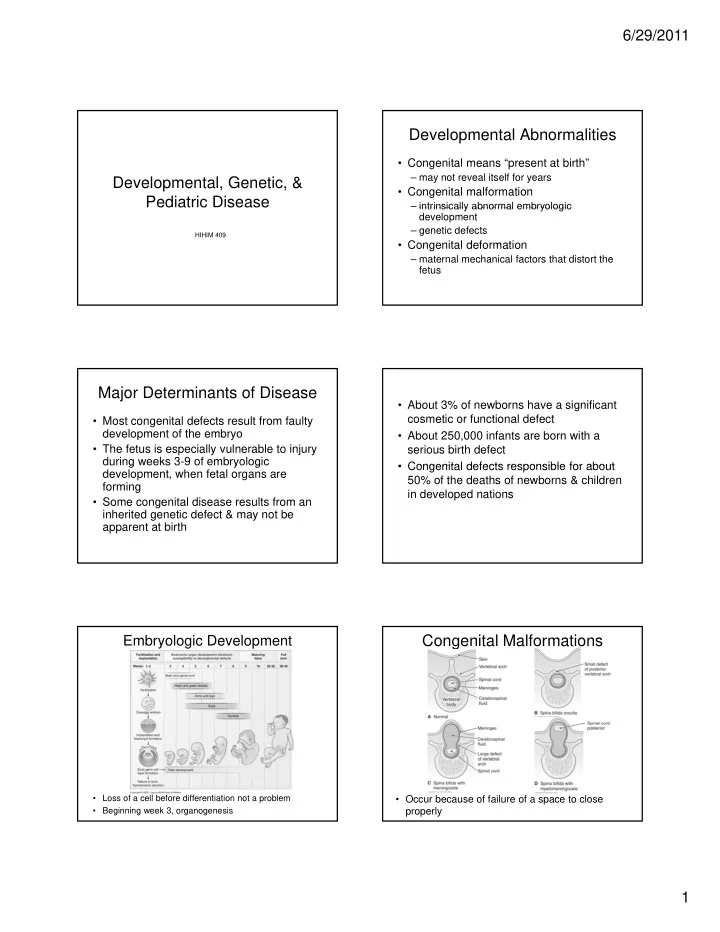
6/29/2011 Developmental Abnormalities • Congenital means “present at birth” – may not reveal itself for years Developmental, Genetic, & • Congenital malformation Pediatric Disease – intrinsically abnormal embryologic intrinsically abnormal embryologic development – genetic defects HIHIM 409 • Congenital deformation – maternal mechanical factors that distort the fetus Major Determinants of Disease • About 3% of newborns have a significant cosmetic or functional defect • Most congenital defects result from faulty development of the embryo • About 250,000 infants are born with a • The fetus is especially vulnerable to injury serious birth defect during weeks 3-9 of embryologic g y g • Congenital defects responsible for about • Congenital defects responsible for about development, when fetal organs are 50% of the deaths of newborns & children forming in developed nations • Some congenital disease results from an inherited genetic defect & may not be apparent at birth Embryologic Development Congenital Malformations • Loss of a cell before differentiation not a problem • Occur because of failure of a space to close properly • Beginning week 3, organogenesis 1
6/29/2011 • Failure of tissue to polydactyly divide syndactyly • Failure of a tissue or • Failure of an organ to differentiate embryologic structure or grow to disappear normally hypospadias Congenital Malformations • Flawed embryologic development VSD Patent ductus arteriosus • Cause unknown • Result from mutations & environmental factors ASD • Teratogens are capable of inducing fetal • Teratogens are capable of inducing fetal malformations – chemical – infectious agent Cleft lip Spina bifida – drugs – ionizing radation anencephaly 2
6/29/2011 Fetal Alcohol Syndrome TORCH • Common infectious • 1:1000 agents • Mom consumes • Toxoplasmosis alcohol • Rubella – how much determines • Cytomegalovirus Cytomegalovirus the severity • Herpesvirus • Fetal growth • In about 1-5% of live restriction, CNS births abnormalities, • Worse if during weeks distinctive facial 3-9 features Congenital Deformations Genetic Disorders • Caused by maternal • Major determinants of disease mechanical factors that – Almost every disease is influenced to some distort fetus degree by genetic variations that confer • Usually arise during vulnerabilities to environmental influences weeks 35-38 weeks 35 38 clubfoot • not always predictable • Maternal factors include – malformed uterus due to – Strictly genetic disease is caused by hip dislocation leiomyomas mutations of the DNA in a predictable manner – crowding from multiple fetuses – decreased amniotic fluid Karyotype • 2 types of cells – germ – somatic • can’t transmit genetic defects • Chromosomes – autosomes – autosomes – sex chromosomes • Genotype – genetic makeup • Phenotype – physical expression of traits 3
6/29/2011 Disease • Genetic – mutations of germ cells – hereditary disease • Environment E i t – affects somatic cells • Combination – both environment influences & strong familial tendencies • Terminology Mutations – Allele • one of a gene pair – Homozygous • Permanent change • alleles are identical – Heterozygous in DNA • alleles are not identical • Mutagens – Dominant • expressed – chemicals – Recessive Recessive • not expressed – radiation – Carrier • Can occur in utero • has recessive gene but no disease – Expressivity • qualitative characteristic • trait expressed in various ways – Penetrance • quantitative characteristic • degree or severity of the abnormality 4
6/29/2011 Sex-Linked Recessive • Present on X chromosome • > 5,000 monogenic disorders have been identified with more being discovered • Genes on Y chromosome related to sperm production • Most humans have about 6-8 defective genes most being recessive & therefore genes, most being recessive & therefore • X & Y share no alleles so disorders affect X & Y h ll l di d ff t not expressed males more often Autosomal Dominant Diseases • Physically expressed if only one copy of gene is present • An affected parent has a 50% chance of passing 50% chance of passing the gene to a child • Have the gene, have the defect • No carriers • Some are due to new mutations Autosomal Recessive Diseases • Physically expressed only if both chromosomes carry a copy of the gene 5
6/29/2011 Enzyme Defects • Accumulation of a substrate or deficiency of an end product • Gaucher disease – accumulation of glucocerebrosides in macrophages • Glycogen storage disease Gl di – defect in the enzyme that converts glycogen to glucose so no glucose • Alpha-1-antitrypsin deficiency – protein that protects tissue from excessive digestion by enzymes from neutrophils Defects in Membrane Receptors or Disease of Growth Control Proteins Transport Proteins • Neurofibromatosis – von Recklinghausen Defects in Structural Proteins 6
6/29/2011 Cytogenetic Diseases • Abnormalities involving large parts or whole chromosomes usually occurring during the production of ova & sperm • One or more extra chromosomes • One or more extra chromosomes • Missing chromosomes • Monosomy – Loss of an autosome – Results in spontaneous abortion as this is not compatible with life compatible with life Trisomy • Extra copy of a chromosome • Most result in spontaneous p abortion – Exceptions are chromosomes 13, 18, 21 7
6/29/2011 Klinefelter syndrome • XXY Genetic Diagnosis Turner Syndrome • If mother is 35yo or greater • If already have a child with a known genetic disorder • If have a family history of genetic problems • XO Pediatric Disease Terminology • Perinatal period • Major determinants of disease from 28 th week of pregnancy to 7 th day after birth – • Neonatal period – pediatric diseases differ materially from adult 1 st month after birth – • Full-term pregnancy diseases – 38-40 weeks • Normal birth weight – genetic defects are a common cause of genetic defects are a common cause of – 3500gms pediatric disease • Post-term infant – born after 42 weeks – maternal factors are the cause of many fetal & • Premature infant born before the end of the 37 th week – neonatal disorders • Low birth weight – < 2500gms • Gestational age – length of time in the womb 8
6/29/2011 • Length of gestation, birth weight, & organ Apgar Score maturity all related • 5 minute score of 0-1 have 50% mortality rate • 7 or better almost 0 mortality rate Intrauterine Growth Restriction Prematurity • Before the end of the 37 th week • About 1/3 of low birth weight infants • SGA • Low birth weight • Maternal factors are most common causes • 5-10% of pregnancies – HTN of pregnancy – malnutrition • Causes – drug or alcohol abuse – preterm rupture of the amnion preterm rupture of the amnion – cigarette smoking cigarette smoking • Placental factors – intrauterine infection – insufficient placental blood flow – multiple fetuses – placenta previa – structural abnormalities of the uterus, cervix, placenta – placenta abruptio • Fetal factors – placental hemorrhage – genetic disease – abnormal placental implantation – congenital anomalies – relaxed cervix – infections Liver Lungs • Do not reach full maturity until • Not fully capable of 6-8yo processing bilirubin • Weeks 28-32 begin to secrete until about 2 weeks of surfactant • If not enough surfactant, have age RDS – hard to keep alveoli open • Treat with – breathing becomes difficult – phototherapy with grunting & retractions – hypoxic & cyanotic – exchange transfusion – damage to alveoli & vessels – fluid accumulation kernicterus – protein in the exudate not absorbed & forms a membrane coating 9
Recommend
More recommend