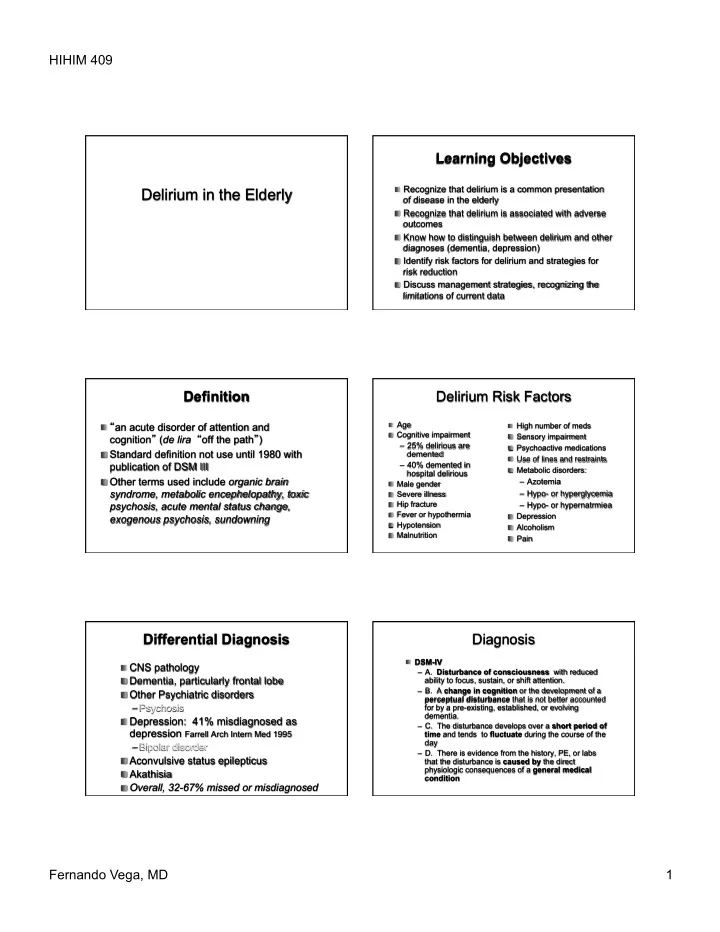
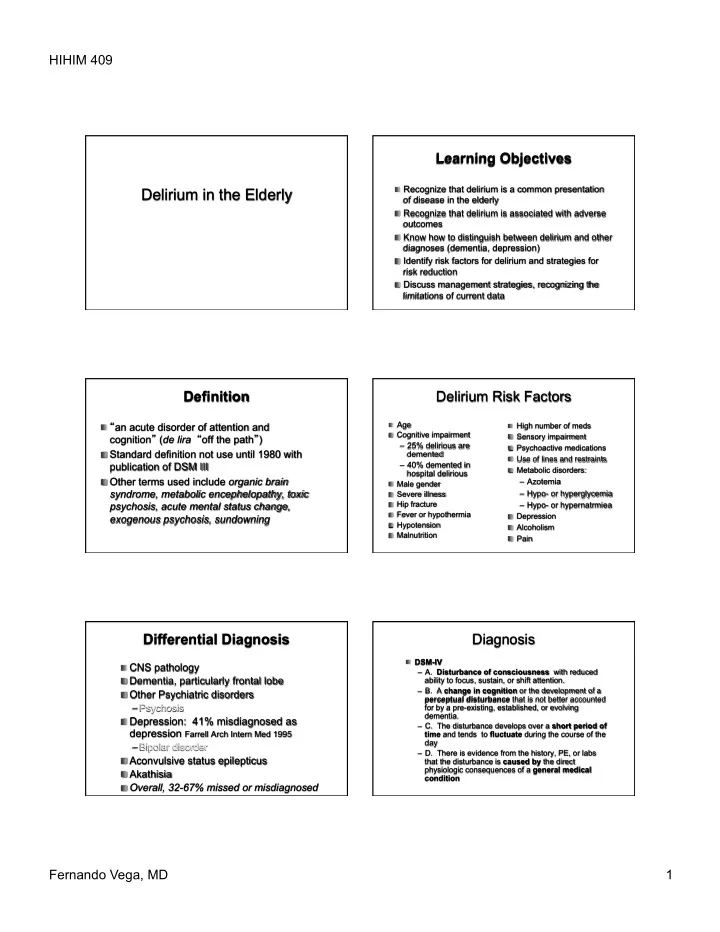
HIHIM 409 Learning Objectives � Recognize that delirium is a common presentation Delirium in the Elderly of disease in the elderly � Recognize that delirium is associated with adverse outcomes � Know how to distinguish between delirium and other diagnoses (dementia, depression) � Identify risk factors for delirium and strategies for risk reduction � Discuss management strategies, recognizing the limitations of current data Definition Delirium Risk Factors Age High number of meds � “ an acute disorder of attention and � � Cognitive impairment � Sensory impairment cognition ” ( de lira “ off the path ” ) � – 25% delirious are Psychoactive medications � � Standard definition not use until 1980 with demented Use of lines and restraints � publication of DSM III – 40% demented in Metabolic disorders: � hospital delirious � Other terms used include organic brain – Azotemia Male gender � syndrome, metabolic encephelopathy, toxic – Hypo- or hyperglycemia Severe illness � Hip fracture psychosis, acute mental status change, – Hypo- or hypernatrmiea � Fever or hypothermia � Depression exogenous psychosis, sundowning � Hypotension � Alcoholism � Malnutrition � Pain � Differential Diagnosis Diagnosis DSM-IV � � CNS pathology – A. Disturbance of consciousness with reduced � Dementia, particularly frontal lobe ability to focus, sustain, or shift attention. – B. A change in cognition or the development of a � Other Psychiatric disorders perceptual disturbance that is not better accounted – Psychosis for by a pre-existing, established, or evolving dementia. � Depression: 41% misdiagnosed as – C. The disturbance develops over a short period of depression Farrell Arch Intern Med 1995 time and tends to fluctuate during the course of the day – Bipolar disorder – D. There is evidence from the history, PE, or labs � Aconvulsive status epilepticus that the disturbance is caused by the direct physiologic consequences of a general medical � Akathisia condition � Overall, 32-67% missed or misdiagnosed Fernando Vega, MD 1
HIHIM 409 Diagnostic Tools CAM (Confusion Assessment Method) � Sensitivity Specificity 1. Acute change & fluctuation in mental status and behavior � CAM* .46-.92 .90.92 AND � Delirium Rating Scale* .82-.94 .82-.94 2. Inattention � Clock draw .87 .93 AND EITHER 3. Disorganized thinking � MMSE (23/24 cutoff) .52-.87 .76-.82 OR � Digit span test .34 .90 4. Altered consciousness (not alert) *validated for delirium & capable of distinguishing delirium � from dementia Inouye SK et al. Ann Intern Med 1990;113:941-948. Diagnosis Delirium versus Dementia � Delirium Dementia � MMSE & Clock draw Insidious onset Rapid onset Primary defect in short term -Not designed for delirium Primary defect in attention memory Fluctuates during the course -Useful at separating “ normal ” from Attention often normal of a day “ abnormal ” Does not fluctuate during Visual hallucinations -Not specific for distinguishing delirium day common Visual hallucinations less Often cannot attend to from dementia common MMSE or clock draw -May be useful as change from baseline Can attend to MMSE or clock draw, but cannot perform well Searching for the cause Medications and Delirium � Sedative-hypnotics, especially benzos � History and PE (consider possible urinary retention & PVR, impaction) � Narcotics, especially meperidine � Discontinue or substitute high risk meds � Anticholinergics � Labs: CBC, lytes, BUN, Cr, glucose, calcium, � Miscellaneous LFTs, UA, EKG – Lidocaine -Propranolol � And if those don ’ t tell you, consider: – Amiodorone -Digoxin � Neuroimaging – H2 Blockers -Lithium � CSF – Steroids -Metoclopromide � Tox screen, thyroid, B12, drug levels, ammonia, cultures, ABG – NSAIAs -Levodopa � EEG - in difficult cases to r/o occult seizures or � Consider any drug a possible cause psych disorders - 17% false neg, 22% false pos Fernando Vega, MD 2
HIHIM 409 Intervention Protocol Possible Benefit From: � Cognition Orientation, activities � Preoperative psychiatric assessment followed by nursing reorienation (33% vs � Sleep Bedtime drink, 14%) massage, music, noise reduction � Postoperative reorienation (87% vs 6%) � Immobility Ambulation, exercises � Preoperative education about delirium (78% vs. 59%) � Vision Visual aids and adaptive � Pre and post operative psychiatric equipment intervention (13% vs 0) � Hearing Portable amplifiers, – British J. Psych 1996 512-515 – Can Med Ass J 1994 965-70 cerumen disimpaction – Nurs Res 1974 341-348 Inouye NEJM 1999 � Dehydration BUN, volume repletion – Res Nurs Health 1985 329-337 Drug therapy Interventions that May Help � Eliminate extra meds, reverse metabolic � All drug therapy has side effects abnormalities, hydration, nutrition � Use only if delirium interfering with therapy, or � Geriatric consultation? risking patient ’ s or others ’ safety and welfare � Education of patients and family � Almost no data on outcomes in drug treated � Re-orientation by staff, family, sitters, clocks, versus non drug treated patients calendars � No good RCTs � Remove nonessential lines and tubes � Approach based on case reports and expert � Quiet, noninterrupted sleep at night opinion � Stimulation (but not too much) during day � Discharge home? Drug Therapy of Delirium Neuroleptics � Considered agents of choice for most � One small RCT of neuroleptics vs. benzos in cases of delirium AIDS associated delirium/dementia found higher SE ’ s with benzos � RCTs in agitation and dementia suggest benefit (NNT = 5) � Improved outcomes with neuroleptics (N=67) � Side effects can include extrapyramidal � Small sample, generalizability uncertain SE ’ s, hypotension, sedation, akathisia – Breitbart et al Am J Psych 1996 231-237 � Sedation effect before antipsychotic effect � Haloperidol, droperidol � Atypicals: Respiridone, olanzapine Fernando Vega, MD 3
HIHIM 409 Atypical neuroleptics Use of Haloperidol � Lowest possible dose, e.g., .5-1.0 BID � Risperidone: for those with side effects from tapering down as delirium clears haloperidol or contraindications � 0.5mg, repeat every 30 minutes until agitation is controlled – Starting dose: .5mg HS or BID � Olanzapine: agent of choice for patients with � Some advocate doubling of dose every 30 minutes until agitation is controlled PD with hallucinations/delirium (probably not wise in elderly!) – Starting dose 2.5mg PO HS or BID � Droperidol can be used IV - more rapid onset – Caution: sedation, hypotension, less anti-psychotic than haloperidol Benzodiazepines Other agents � Should usually be avoided � ?Trazadone 25-100mg � Agents of choice for EtOH, benzo � Physostigmine (don ’ t try this) withdrawal – reverses delirium due to anticholinergic activity � More rapid onset than neuroleptics – SE ’ s: bradycardia, asystole, � Peak effects brief, sedation more common, bronchospasm, seizures can prolong delirium � ?Donepezil � May be useful in terminal delirium associated with high dose narcotics and � ?Mood stabilizers myoclonus � Narcotics and pain medications (empiric � Lorazepam .5-1 mg IV or PO (t1/2 15-20 use in patients with dementia often helpful) hours) Prevention is the Best Medicine � Summary � Delirium is common in older inpatients, associated with poor outcomes, and � All evidence suggests that it is easier to commonly missed or misdiagnosed PREVENT delirium than to TREAT � Prevention is the best approach delirium � Management involves treating underlying � Prevention of delirium is least likely to be causes, minimizing medications, supportive possible in the intensive care unit care, and avoidance of restraints when � Treatment of delirium in the intensive care possible unit is particularly challenging and most � ICU delirium poses particular challenges likely to require medications, sitters, and/ � Further research and RCTs are needed or physical restraints Fernando Vega, MD 4
Recommend
More recommend