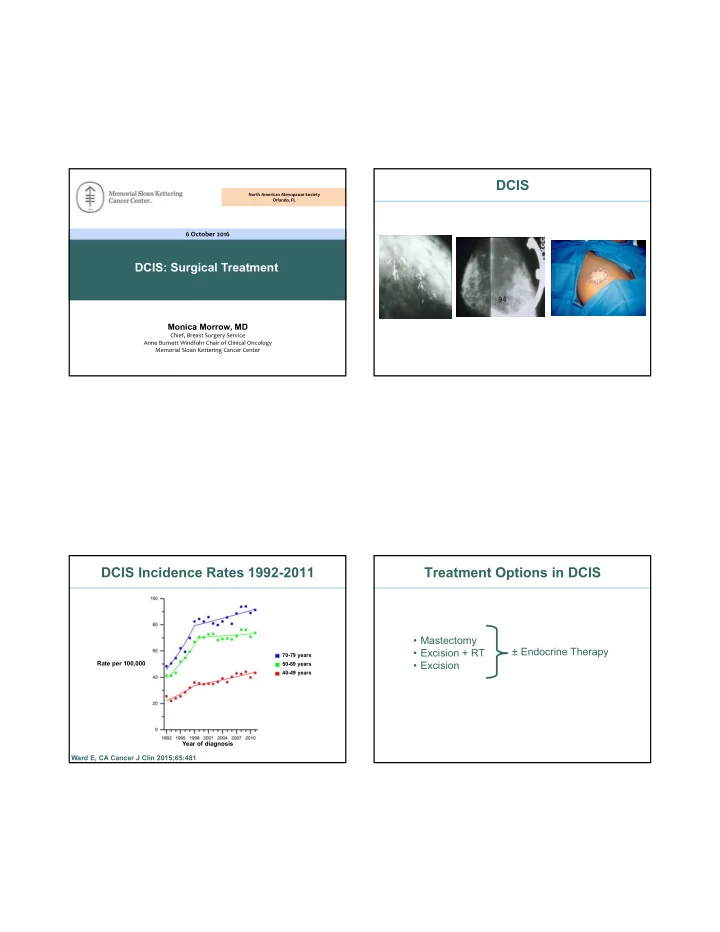
DCIS North American Menopause Society Orlando, FL 6 October 2016 DCIS: Surgical Treatment Monica Morrow, MD Chief, Breast Surgery Service Anne Burnett Windfohr Chair of Clinical Oncology Memorial Sloan Kettering Cancer Center DCIS Incidence Rates 1992-2011 Treatment Options in DCIS • Mastectomy ± Endocrine Therapy • Excision + RT 70-79 years • Excision Rate per 100,000 50-69 years 40-49 years Year of diagnosis Ward E, CA Cancer J Clin 2015;65:481
Outcome of Surgical Treatment in DCIS Outcome of Surgical Treatment in DCIS Worni et al, J Natl Cancer Inst 2015 SEER Study DCIS 1991-2010 Narod et al, JAMA Oncol 2015 n = 121,080 SEER Study DCIS 1998-2011 n = 108,196 Mean f/u 7.5 yrs (0-24) Breast Cancer Specific Mortality 3.3% (95% CI 3.0-3.6%) Narod S, JAMA Oncol 2015;1:888 Worni M, J Natl Cancer Inst 2015;107:djv263 SEER9 Age Adjusted Incidence Rate of Outcome of Surgical Treatment in DCIS Breast Cancer by Stage (1973–2005) Sagara et al, J Clin Oncol 2016 SEER Study DCIS 1998-2007 Incidence rate (per 100,000) n = 32,144 BCS ± RT Mean f/u 8.0 yrs 10 yr Breast Cancer Specific Mortality 1.8% RT n = 20,329 2.1% no RT n = 11,815 Sagara Y, J Clin Oncol 2016;34:1190
DCIS Factors Influencing Patient Decisions 100% greatly Do excellent outcomes with treatment translate to 90% moderately excellent outcomes with less or no treatment? 80% not/slightly 70% 60% • Mortality is not a useful endpoint—low with all 50% treatments 40% • Local recurrence varies with treatment and is 30% important to patients 20% 10% 0% recurrence radiation recovery body/sexuality Katz S, J Clin Oncol 2005;23:5526 Presence of Invasive Cancer After Why Do We Perform Surgery in DCIS? Core Needle Biopsy of DCIS All Cases n = 7350 Underestimate: 25.9% (95% CI 22.5-29.5) • Exclude the presence of invasive cancer at Predictors diagnosis 14g vs 11g Bx High nuclear grade Palpable Size > 20mm Mammographic mass • Reduce the risk of future development of invasive cancer Low Risk Lesions Low/Int grade Underestimate n = 1385 21.1% (15.4, 28.3) Size on imaging ≤ 20mm n = 2783 20.1% (12.3, 31) Brennan M, Radiology 2011;260:119
Metaanalysis of Long Term Outcomes Metaanalysis of Long Term Outcomes of Local Therapy for DCIS of Local Therapy for DCIS 5 prospective, 21 retrospective studies Follow up ≥ 10 yrs n = 9404 Treatment 10 yr LR BCS 25.1% Treatment 10 yr LR 95% CI BCS + Tam 24.7% Mastectomy 2.6% 0.8-4.5 BCS + RT 14.1% BCS + RT 13.6% 9.8-17.4 BCS + RT + Tam 9.7% BCS 25.5% 18.1-32.9 Stuart K, BMC Cancer 2015;15:890 Stuart K, BMC Cancer 2015;15:890 Excision Alone in Favorable DCIS: DCIS ECOG-ACRIN E5194 Cohort 1 Cohort 2 Is the outcome of excision alone in selected, low risk DCIS patients good enough that we should consider Low/int grade High grade eliminating excision? ≤ 2.5 cm ≤ 1 cm n = 561 n = 104 Median f/u 12.3 years * Protocol specified 3 mm or greater margin Solin L, J Clin Oncol 2015;33:3938
LR After Excision Alone for DCIS Margins and LR: ECOG-ACRIN E5194 12 Year Results of ECOG-ACRIN E5194 Cohort 1: Low/int grade Low/Int grade T ≤ 2.5 cm High grade n = 561 Margin Width, mm 12 yr IBTR 3 ‒ 5 15.5% 5 ‒ 9 14.0% p = .87 > 10 13.4% Solin L, J Clin Oncol 2015;33:3938 Solin L, J Clin Oncol 2015;33:3938 What Is the Risk of Invasive Recurrence Impact of Invasive Recurrence After Excision Alone in Low Risk DCIS? on Mortality ECOG 5194 NSABP B17/B24 EORTC 10853 Breast Cancer Mortality Invasive Invasive DCIS Years since IBTR Wapnir I, JNCI 2011;103:1 Donker M, J Clin Oncol 2013;31:4054 Solin L, J Natl Cancer Inst 2013;105:701
RTOG 9804: RT vs Observation in Good Risk DCIS n = 629 Modern molecular biology should be able to identify low/int grade a truly low risk subset of DCIS patients < 2.5 cm size margins ≥ 3 mm Local Failure (%) True, but that hasn’t happened yet Time Since Random Allocation (years) McCormick B, J Clin Oncol 2015;33:709 Comparison of Ontario Cohort to E5194 Cohort: DCIS Score KM 10yr Estimates of Risk of Local Recurrence ECOG E5194 Ontario DCIS Cohort Local Recurrence Risk (%) Local Recurrence Risk (%) Solin L, J Natl Cancer Inst 2013;105:701 Rakovitch E, SABCS 2014 Solin L, J Natl Cancer Inst 2013;105:701
Surgery vs Active Monitoring Treatment With Excision Alone for Low Risk DCIS (LORIS) R Treatment with excision alone, regardless of margin Surgery Eligibility A width, is associated with substantially higher rates of N IBTR than treatment with excision and WBRT, even in D Age > 46 years pre-defined low risk patients Screen detected calcifications O 11g VAB M Non-high grade DCIS I Observation Core Bx Level 1 evidence Z Excision + margins Annual Mammogram E Endpoint: Development of invasive cancer at 5 years Enrollment: 932 patients over 6 years PI: Adele Francis Results What Is the Risk of Invasive Cancer in Rate of Upgrade to Invasive Carcinoma Patients Meeting LORIS Eligibility Criteria? • Surgical excision for DCIS diagnosed by core-needle Total Population biopsy 2009-2012 n = 296 • Meeting all clinical and pathologic LORIS criteria • 296 patients Upgrade to invasive No Upgrade at (approx 16% of DCIS) carcinoma surgical excision n = 58 (20%) n = 238 (80%) Pilewskie M, Ann Surg Oncol 2016 (Epub) Pilewskie M, Ann Surg Oncol 2016 (Epub)
Results Results Tumor Characteristics of Cases with an Upgrade Treatment Recommendations of Upgraded Cases Final Invasive Stage n = 58 Invasive upgrades (n = 57)* Proportion % Stage IA (pN0) Stage IB Stage IIA Radiation therapy 27/30 90% 54 (93%) 1 (2%) 3 (5%) Endocrine therapy 48/54 89% 26/58 = 45% have tumor pathology T1mic T1N1mi T1N1 Chemotherapy** 10/57 18% that warrants genomic profiling or 13 (22%) 1 (2%) 2 (3%) Adjuvant treatment recommended 53/57 93% consideration for chemotherapy T1a T2N0 26 (45%) 1 (2%) *treatment information missing for one patient **indications for chemotherapy: High/intermediate recurrence score, node positive or T1b HER2 overexpressing disease, triple negative, high-risk tumor features 14 (24%) T1c 1 (2%) Pilewskie M, Ann Surg Oncol 2016 (Epub) Pilewskie M, Ann Surg Oncol 2016 (Epub) Mastectomy Use Based on Conclusions Who Made the Surgery Decision 35 • Survival outcomes are excellent in DCIS regardless of treatment, but risk of LR varies 30 Surgeon significantly 25 Shared Patient 20 % • Good outcomes with treatment do not necessarily 15 mean good outcomes without treatment 10 5 • Observation without excision is not warranted 0 White outside of a clinical trial Adjusted for age, marital status, # surgeons visited, comorbidity, tumor size, grade, SEER site Katz S, J Clin Oncol 2005;23:5526
Conclusions • Patients are major drivers of radical treatment in DCIS • Surgeons can reduce overtreatment by avoiding SN biopsies in BCT patients and re-excisions for margins > 2 mm
Recommend
More recommend