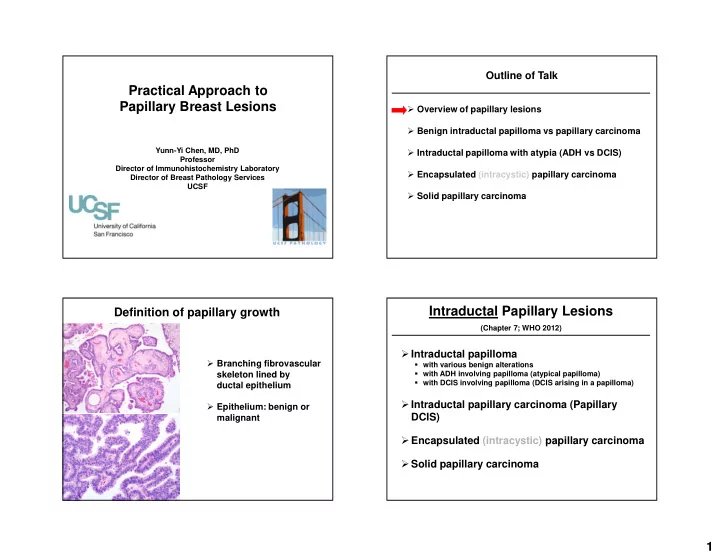
Outline of Talk Practical Approach to Papillary Breast Lesions � Overview of papillary lesions � Benign intraductal papilloma vs papillary carcinoma Yunn-Yi Chen, MD, PhD � Intraductal papilloma with atypia (ADH vs DCIS) Professor Director of Immunohistochemistry Laboratory � Encapsulated (intracystic) papillary carcinoma Director of Breast Pathology Services UCSF � Solid papillary carcinoma Intraductal Papillary Lesions Definition of papillary growth (Chapter 7; WHO 2012) � Intraductal papilloma � Branching fibrovascular � with various benign alterations skeleton lined by � with ADH involving papilloma (atypical papilloma) � with DCIS involving papilloma (DCIS arising in a papilloma) ductal epithelium � Intraductal papillary carcinoma (Papillary � Epithelium: benign or DCIS) malignant � Encapsulated (intracystic) papillary carcinoma � Solid papillary carcinoma 1
Outline of Talk Papillary Intraductal Patterns � Overview of papillary lesions Papillary Carcinoma � Benign intraductal papilloma vs papillary carcinoma (Papillary DCIS & Encapsulated papillary CA) � Intraductal papilloma with atypia (ADH vs DCIS) versus � Encapsulated (intracystic) papillary carcinoma � Solid papillary carcinoma Intraductal papilloma Papillary DCIS with adjacent cribriform and micropapillary DCIS 2
3
Intraductal papilloma 4
Papilloma: Myoepithelial Markers Actin p63 SMM 5
Myoepithelial markers, CK5/6 and ER-- IHC markers useful in distinguishing papilloma from papillary carcinoma Benign papilloma retains a continuous layer of Papilloma vs Papillary carcinoma ME cells along the fibrovascular cores P63 stain 6
Papillary carcinoma lacks Papilloma with UDH: CK5/6 + Papillary carcinoma: CK5/6 - ME cells along the fibrovascular cores P63 stain Papillary Carcinoma-- Benign Papilloma-- � CK5/6 negative � CK5/6 positive � ER diffuse and strong � ER patchy and variable CK5/6 CK5/6 ER ER 7
SMM stain Pitfalls in Interpretation of MEC Markers � SMM/calp: stain pericytes/myofibroblasts, mimic ME cells � p63: may stain cancer cells, mimic ME cells � CK5/6: does not stain pericytes/myofibroblasts or cancer cells, but not a consistent MEC marker SMM p63 CK5/6 p63 stain CK5/6 stain 8
Papillary DCIS often with attenuated MEC expression around the ducts Pitfalls in Interpretation of MEC Markers � SMM/calp: stain pericytes/myofibroblasts, mimic ME cells � p63: may stain cancer cells, mimic ME cells � CK5/6: does not stain pericytes/myofibroblasts or cancer cells, but not a consistent MEC marker SMM p63 CK5/6 Histologic features helpful in distinguishing Outline of Talk benign papilloma from papillary carcinoma in situ Benign papilloma Papillary DCIS � Overview of papillary lesions Connective tissue Prominent, variable fibrosis Thin/delicate stroma � Benign intraductal papilloma vs papillary carcinoma Cell types Epithelial and myoepithelial Epithelial cells cells � Intraductal papilloma with atypia (ADH vs DCIS) Cytologic features Heterogeneous population, Monotonous population, normochromatic hyperchromatic � Encapsulated (intracystic) papillary carcinoma Cell organization Haphazard (as in UDH) Regular architecture: cribriform, rigid bar, solid, � Solid papillary carcinoma micropapillary (as in DCIS) Apocrine metaplasia Present Absent Adjacent ducts Usual ductal hyperplasia DCIS (adapted from Kraus and Neubecker, Cancer 1962;15:444-455) 9
Papilloma with “Atypia” 10
11
Epithelial Proliferation in a Papilloma Papilloma with Atypia � Benign (UDH) vs atypical LG � Same criteria as in non-papillary lesions ADH � UDH: heterogeneous cells, irregular architecture DCIS � Atypical: monomorphic cells, rigid architecture � Adjunct IHC markers � UDH: strong/mosaic CK5/6, patchy ER Where to draw the line? � Atypical: negative CK5/6, diffuse ER “Papilloma with Atypia” Papilloma with Atypia Where to draw the line: Size: Page et al. How much is enough for DCIS? � ADH vs. DCIS cutoff >3mm � Page et al: Size Atypical area > 3mm ( Cancer 1996;78:258) � Risk of subsequent breast CA: � Increased vs. papillomas without atypia (RR ~7.5x) � Tavassoli: Proportion � Unlike ADH in parenchyma: Atypical area > 1/3 (Pathol of the Breast 2 nd Ed,1999) � ipsilateral and same site as original papilloma � Elston, Ellis & Pinder: Qualitative � Risk between ADH in parenchyma and LG DCIS “Overt features of malignancy, no matter what the proportion” (The Breast, 1998) ( Cancer 1996;78:258) 12
“Papilloma with Atypia” Papilloma with Atypia Where to draw the line: How much is enough for DCIS? Proportion: Tavassoli � Elston, Ellis & Pinder: Qualitative “Overt features of malignancy, no matter what the proportion” (The Breast, 1998) � Ellis: Qualitative “ADH…less than 2 -3 mm. Larger foci are accepted if associated with ……a papilloma” (Modern Pathol, 2010) 6 mm 6 mm Pathology of the Breast 2nd Ed,1999 Papilloma with Atypia Papilloma with Atypia ADH vs. DCIS: WHO 2012 ADH vs. DCIS: WHO 2012 � Size: Page et al. � Size: Page et al. Atypical area > 3mm Atypical area > 3mm � WHO disclaimer � Proportion: Tavassoli “It is acknowledged that this is a pragmatic Atypical area > 1/3 guideline and that scientific evidence for this size criterion to diagnose LG DCIS is lacking” � Qualitative: Elston, Ellis & Pinder “Overt features of malignancy, no matter what the proportion” 13
Outline of Talk Papilloma with Atypia Caution � Overview of papillary lesions � Benign intraductal papilloma vs papillary carcinoma � Intraductal papilloma with atypia (ADH vs DCIS) � Only for ADH vs LG DCIS � Encapsulated (intracystic) papillary carcinoma � Not for intermediate or high grade � Solid papillary carcinoma DCIS (any amount is diagnostic) Encapsulated/intracystic papillary carcinoma • Single cystic space/duct • Often central • Well circumscribed • Fibrous capsule 14
Encapsulated/intracystic papillary carcinoma • Single cystic space/duct • Often central • Well circumscribed • Fibrous capsule • Older women (average 65 yrs) • Indolent behavior • Traditionally = variant of DCIS • But… Encapsulated/Intracystic Papillary Carcinoma-- Encapsulated/intracystic papillary Carcinoma-- Negative MEC IHC at periphery Negative MEC IHC at periphery SMM AJCP 2005;123:36 AJSP 2006;30:1002 15
Encapsulated PC showing skeletal muscle invasion-- Is encapsulated/intracystic papillary CA invasive? (h/o intracystic papillary ca, s/p mastectomy, chest wall nodule) Invaded Past Compressed Myoepithelium Myoepithelium ? Invasive In-situ Controversial ! Encapsulated papillary ca in breast Encapsulated papillary ca metastatic to axillary LN Encapsulated papillary ca metastatic to axillary lymph node 16
Mammary papillary carcinoma metastatic to lung (h/o papillary DCIS 10 years ago, s/p mastectomy) Although lymph node or even systemic metastasis can occur in patients with EPC, this is a very rare event! Encapsulated Papillary CA Encapsulated/intracystic papillary carcinoma: an invasive tumor with circumscribed growth and excellent prognosis Behavior Regardless of whether these are in situ or invasive cancers, clinical outcome is excellent with AJSP 2011;35:1 adequate local therapy alone (akin to DCIS) AJSP 2011;35:1093 Carter 1983; Lefkowitz 1994; Leal 1998; Harris 1999; Solorzano. 2002; Hill 2005; Grabowski 2008; Gore 2009; Esposito 2009; Wynveen 2011; Rakha 2011 17
Encapsulated Papillary CA 11 Studies, 231 Patients --California Cancer Registry Mastectomy, Excision alone or with RT --1988-2005 Outcome No. of Events 917 cases: 427 “CIS” 490 “Invasive” Local 2 Relative cumulative survival (specific) Recurrence Intracystic Pap Invasive Breast Positive 1 Axillary LN 5 yr 97.3% 83.2% Distant 10 yr 95.6%* 74.6% 1 Metastases *CIS 96.8%, Invasive 94.4% (p = n.s.) Died of 0 Disease Adapted from Rakha, et al. Am J Surg Pathol 2011;35:1093 (Table 2) Encapsulated Papillary CA (WHO 2012, AJCC 7 th Ed) � Continue to manage as for DCIS � 208 encapsulated, 30 solid papillary � 339 cases from review of literature � Avoid over-diagnosis as frankly invasive � Most lack myoepithelial layer � special type papillary carcinoma of invasive carcinoma: � Infrequent lymph node mets (~3%), infrequent � Stage as pTis local or distant recurrence � Indolent behavior, “extremely favorable prognosis ” � If associated with conventional invasive • Local therapy adequate, no chemotherapy CA, staged by size of definite invasive CA 18
Evaluation of “invasion” in EPC Evaluation of “invasion” in EPC � Challenging � Atypical glands or tumor nests beyond the capsule � Typcally IDC, nos Not sufficient Encapsulated papillary ca with adjacent IDC Evaluation of “invasion” in EPC � Recognized pattern of invasive ca � Invades beyond the fibrous capsule of Adjacent to capsule Granulation tissue & hemosiderin EPC into adjacent stroma Not sufficient EPC IDC IDC EPC 19
Recommend
More recommend