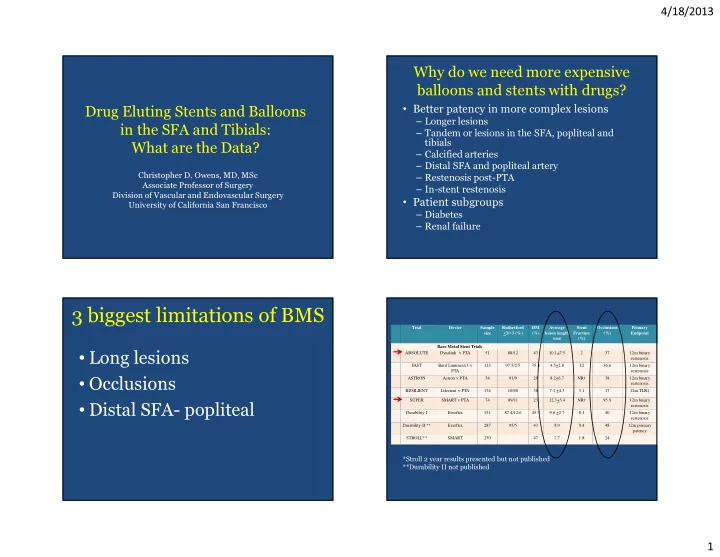
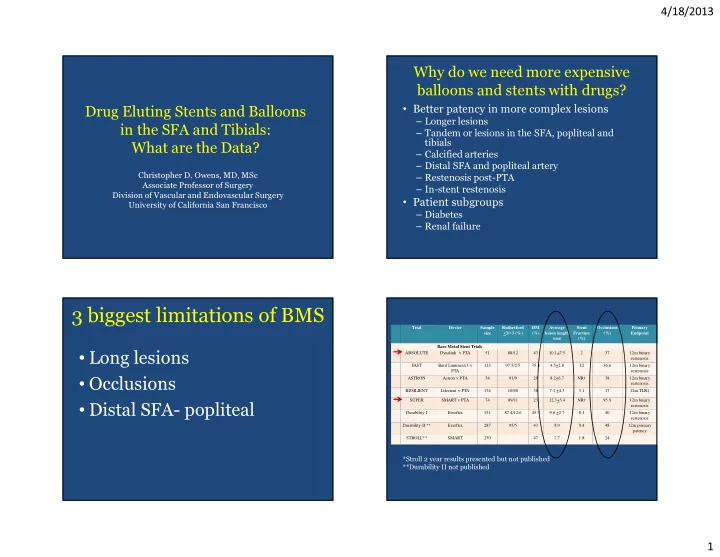
4/18/2013 Why do we need more expensive balloons and stents with drugs? • Better patency in more complex lesions Drug Eluting Stents and Balloons – Longer lesions – Tandem or lesions in the SFA, popliteal and in the SFA and Tibials: tibials What are the Data? – Calcified arteries – Distal SFA and popliteal artery – Restenosis post-PTA Christopher D. Owens, MD, MSc Associate Professor of Surgery – In-stent restenosis Division of Vascular and Endovascular Surgery • Patient subgroups University of California San Francisco – Diabetes – Renal failure 3 biggest limitations of BMS Trial Device Sample Rutherford DM Average Stent Occlusions Primary size <3/>3 (%) (%) lesion length Fracture (%) Endpoint (cm) (%) Bare Metal Stent Trials • Long lesions ABSOLUTE Dynalink v PTA 51 88/12 43 10.1+7.5 2 37 12m binary restenosis FAST Bard Luminexx3 v 123 97.5/2.5 35.8 4.5+2.8 12 36.6 12m binary PTA restenosis • Occlusions ASTRON Astron v PTA 34 91/9 29 8.2+6.7 NR† 38 12m binary restenosis RESILIENT Lifestent v PTA 134 100/0 38 7.1 +4.3 3.1 17 12m TLR‡ SUPER SMART v PTA 74 89/11 23 12.3+5.4 NR† 95.9 12m binary • Distal SFA- popliteal restenosis Durability I Everflex 151 87.4/12.6 45.7 9.6 +2.7 8.1 40 12m binary restenosis Durability II ** Everflex 287 95/5 43 8.9 0.4 48 12m primary patency STROLL** SMART 250 47 7.7 1.8 24 *Stroll 2 year results presented but not published **Durability II not published 1
4/18/2013 Freedom from Binary Restenosis at 1 year (%) 90 p=.0001 NA 80 NA p=.377 70 p=.028 p=.01 p=.84 60 50 10 cm, 37% 40 12 cm, 30 96% 20 10 0 Resilient Durability I Durability Super ABSOLUTE FAST ASTRON II Current Surgery Reports 2013 Differential rates of endothelialization What is a drug coated stent? SES PEX ZES EES BMS Coronary Artery Disease 2010;21:46-56 J Controlled Release 2012 2
4/18/2013 Manufacturer Device Drug Polymer Indicatio Trials n J & J Enrollment Cypher Sirolimus 3 layer coating: Cardiac RAVEL, N=479 Parylene C, PEVA, SAPPHIRE, SIRIUS PBMA Primary randomization Boston Scientific Taxus Paclitaxel Translute SIBS Cardiac ELUTES, TAXUS 12 month primary patency (nonresorbable II, ASPECT rate: elastomeric) PTA Zilver PTX Boston Scientific Ion Paclitaxel Triblock copolymer Cardiac PERSEUS • Zilver PTX vs PTAall, (83.1% N=238 N=241 (polystyrene and vs. 32.8%, p<.01; Zilver PTX vs. polyisobutylene) Boston Scientific Promus Everolimus PBMA, PVDF-HFP Cardiac SPIRIT PTAoptimal, (83.1% vs. 65.3%, Guidant and Xience V Everolimus Fluoropolymer Cardiac SPIRIT p<.01. Abbott Suboptimal Optimal Guidant and PTA (>30% residual Xience Everolimus Fluoropolymer Cardiac SPIRIT PTA Abbott stenosis) Prime N=118 Medtronic N=120 Endeavor Zotarolimus Phosphorylcholine Cardiac ENDEAVOR Cook Zilver PTX Paclitaxel None Femoro- Zilver PTX Secondary randomization popliteal 12 month primary patency rate: Bare Zilver Zilver PTX • Provisional ZilverPTX vs N=59 N=61 provisional Zilver BMS, (89.9% vs. 73%, p=.01) Circ Cardiovasc Interv 2011;4:495-504 Lesion characteristics Patient characteristics of ZilverPTX of ZilverPTX • Length = 5.5 cm • Occlusion = 27% • Distal SFA/popliteal = 7% in Rx arm 3
4/18/2013 SFA IDE Trial Results: K-M Patency 100.0% Primary Patency K-M Reported 12 Month 90.0% DES 83% 82% 81% 77% 80.0% Drug-Coated 70.0% Standard Nitinol Stents 60.0% 50.0% Zilver PTX Zilver PTX Smart Stroll Resilient Durability II PTA Stent LifeStent EverFlex 236 250 Patient sample size 134 287 Diabetics (%) 49 47 38 43 Avg. lesion length 5.4 7.7 7.1 8.9 (cm) 0.9 1.8 Fracture rate (%) 3.1 0.4 Occlusion (%) 27 24 17 48 PSVR 14 2.0 2.5 2.5 2.0 14 Circ Cardiovasc Interv 2011;4:495-504 The ZilverPTX Single Arm Study: 12- 3 Year Effectiveness month results from the TASC C/D Primary Patency (PSVR < 2.0): Zilver vs. PTA lesion subgroup 50 ABSOLUTE Trial Restenosis rate 40 • Lesion length 22 cm 30 20 • Occlusions 84% 10 0 • Distal SFA/Popliteal 3.7% 6 month 12 month 24 month • Popliteal 0% Data presented by DAKE at LINC 2013 J Cardiovasc Surg 2013;54:115-22 4
4/18/2013 Single arm open label everolimus-eluting stent in Relative differences in patency in long SFA lesions the SFA – STRIDES Study 90 Percent patency 12 mo Ethylene vinyl alcohol copolymer & prolonged elution time over 90 days 80 70 60 50 77% Dynalink-E self-expanding everolimus-eluting stent 225 µg everolimus/cm 2 40 67% 30 53% 20 Primary patency = 68% at 12 months 10 0 ZilverPTX ABSOLUTE SUPER J Cardiovasc Surg 2013;54:115-22 & Cardiovasc Intervent Radiol 2013;36(2):353-61 & N Engl J J Vasc Surg 2011;54:394-401 Med 2006;354: 1879-88 Drug Eluting Stents Strut Thickness Product Polymer Properties Polymer Thickness Polymer DESTINY TRIAL • CLI population Total Drug 85.2% 85.2% • Target lesion length = 17 mm 132 um TAXUS™ • Thrombus P=.0001 • RVD = 3 mm 16 um SIBS • Inflammation • Significance ca++ = 76% 54.4% 148 um PTX • Rate/Degree of 54.4% • CTO 16% Endothelialization 140 um CYPHER™ • Platform was Multi-link Vision 12.6 um PEVA/PBMA stent 152.6 um Sirolimus • Xience V 91 um ENDEAVOR™ • Multi-link Vision 5.3 um PC Polymer • Polymer coating 96.3 um Zotarolimus (poly[vinylidene fluoride- 81 um XIENCE™ co-hexafluoropropylene] 7.6 um Fluropolymer PVDF-HFP 88.6 um Everolimus • Everolimus 20 J Vasc Surg 2012;55:390-9 5
4/18/2013 ACHILLES trial • CYPHER SELECT sirolimus eluting stent • Mean lesion length 27 mm • 80% CTO • Mixed CLI/IC population JACC vol 60, No22, 2012 JACC vol 60, No22, 2012 ACHILLES trial 90 primary patency 80 70 • Angiographic primary endpoint of 1 year 60 lower restenosis rates SES 50 • Study fairly limited by short lesions, and 40 incomplete follow up. POBA 30 20 10 0 DES Control JACC vol 60, No22, 2012 Vasa 2012;41:90-95 & Cardiovasc Intervent Radiol 2013 6
4/18/2013 DES in BTK How is DCB different from DES • Appear to be safe in the 165 patients treated Parameters that DES DCB in RCTs distinguish DCB from DES • Like the coronary artery in which DES do not Drug concentration on the Low Very high 2-3 µg/mm 2 ( ≈ 20-30 µg/mm) device 5-10µg/mm improve patient survival, MI, or major Drug transfer at the time of slow Rapid, all at once deployment adverse cardiac events, DES in the tibials have Reservoir of drug Polymer (except No (excipient important) ZilverPTX) not been shown to improve patient or limb Drug retention in tissues Short term Need a drug which binds to cell salvage, wound healing, or index limb membranes and is easily transferable to adjacent cells amputations. diffusion good Excellent • May be useful for spot stenting or tidying up a lipophilic yes Even better Active ingredient Not necessary Should be active immediately long segment treated with balloon angioplasty > 20 DCB in development or in early phase trials in Europe 7
4/18/2013 1.8 PACCOCATH 4 DEB Technologies and 5 DEB Trials with 6-month LLL 1.6 primary Endpoint 1.4 PASSEO 1.2 MOXY 18-Lux 1 0.8 IN.PACT 0.6 7.5 cm, 6.0 cm, 6.1 cm, 0.4 6.1 cm 27% 15% 40% 6.8 cm, 30.8 % 0.2 0 THUNDER FEMPAC LEVANT 1 BIOLUX P-I PACIFIER -0.2 Conclusions: Existing Data • Metal implants have the disadvantage of inducing excessive neointimal hyplerplasia due movement, nicro-abrasion and inflammation with motions as simple as walking 87.8% • Can a combination of toxic drug and metal improve the results – for short term, yes especially in longer lesions. Long term will be confronted with increasing failure and increasing stent fracture as all DES become BMS. Late restenosis catch up a concern. • DCB – simple technology however acute results show high rate of failure in long or complex lesions. Elastic recoil and constrictive remodeling remain a problem. < 500 patients with 6 month data reported to date! • DCB’s will also show a high rate of failure in the long-term as drug distribution is not even within the arterial wall. Drug stays for a short time and therefore late restenosis will occur. However, one can • Length 7.6 cm repeat the procedure. • Improvements of DCB are still required to achieve better drug 12.4% stent rate • Occlusion 34% distribution and longer duration to prevent early restenosis and distal emboli. Combination of DCB and spot stenting or plaque • Popliteal 12% tacking may be the answer • DUS PSVR 2.4 J Am Coll Cardiol Intv 2012;5:331-8 8
Recommend
More recommend