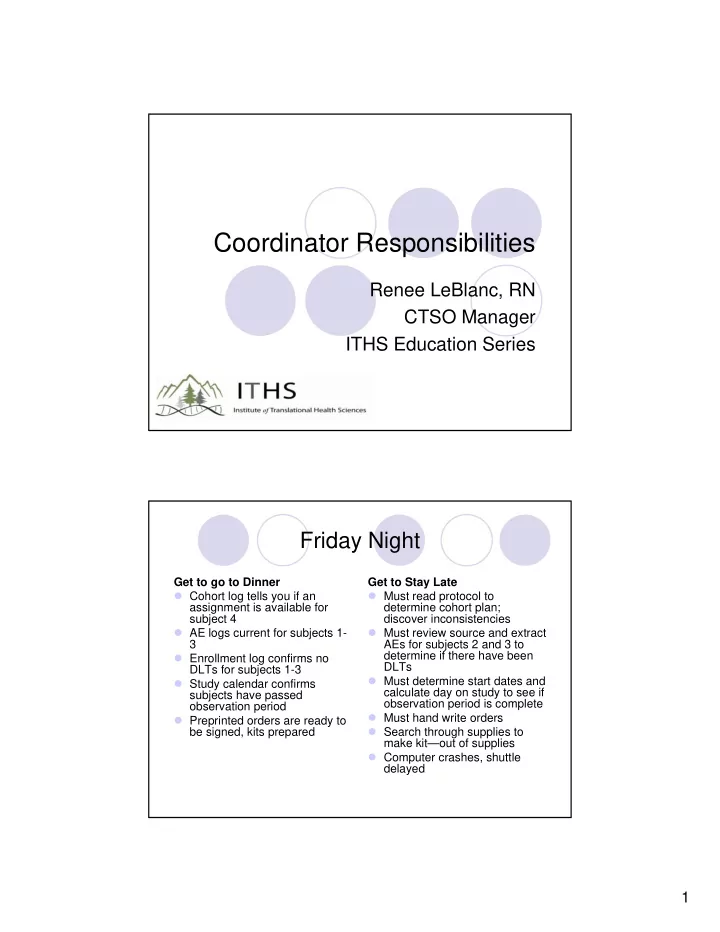
Coordinator Responsibilities Renee LeBlanc, RN CTSO Manager ITHS Education Series Friday Night Get to go to Dinner Get to Stay Late Cohort log tells you if an Must read protocol to assignment is available for determine cohort plan; subject 4 discover inconsistencies AE logs current for subjects 1- Must review source and extract 3 AEs for subjects 2 and 3 to Enrollment log confirms no determine if there have been DLTs DLTs for subjects 1-3 Must determine start dates and Study calendar confirms calculate day on study to see if subjects have passed observation period is complete observation period Must hand write orders Preprinted orders are ready to Search through supplies to be signed, kits prepared make kit—out of supplies Computer crashes, shuttle delayed 1
Objectives Improve your Understanding of the Study Coordinator Role and Responsibility for Promoting patient safety Supporting protocol compliance Producing quality data Purpose of Attending A strong foundation of understanding the application of the principles of GCP is assurance of subject protection Act purposefully with sound judgment Respond to challenging situations with best options Confidence defending your actions to monitors and auditors 2
Subject Safety Focus on Priorities To minimize risk Consent Eligibility Safety labs AE CRFs Protocol adherence unless to avoid immediate harm Quality data 3
What if? Adult subject determined eligible for study while under conscious sedation. Mother thinks it’s a great study and signs the consent. Autonomy? New risk language is known to the PI but IRB will not review prior to subject appointment Subject needs blood draw for eligibility; PI wants standard care labs resulted before clinic visit to determine if pt can start chemo on or off protocol. The Regulations 45 CFR 46 (aka “The Common Rule”) gives requirements for consenting and documentation of consenting for research 21 CFR 50 Protection of Human Subjects 50.24 lists the basic elements of informed consent. 50.20 General Requirements of Informed Consent 21 CFR 312.60 General Responsibilities of Investigators, “An investigator shall,…, obtain informed consent…” ICH GCP Guidelines 4.8 Informed Consent of Trial Subjects 4.8.7 …provide the subject with ample time… Institution policy and procedure 4
How Coordinators Support Subject Safety Participate in the informed consent process; ensure adequate time and access to personnel qualified to answer questions in order that the subject can make an informed decision. Schedule follow up appointments if necessary Ensure subject’s questions are answered Ensure documentation of the process Reconsent if new information or procedures May need pre-research lab consent to determine eligibility and stay in compliance (HAMA) Informed Consent Know the Dos What went Wrong Sign the most current (Paper) consent in drawer version expired Process conducted by Physician not available to licensed personnel sign consent document Document process Process started by left off with indecision; dates Consent prior to study don’t match procedures Blood draw before clinic Re-consent when new appointment risk and procedures Subject has left system 5
Coordinator Responsibilities What went wrong Corrective Action (Paper) consent in drawer Team utilizes central file expired with current documents Physician not available to Develop a process to sign consent document include PI in follow up consent Progress notes indicate Document subject gave subject undecided informed consent Signature dates don’t Note file explaining date match discrepancies Blood draw before clinic Research lab blood draw appointment consent Subject has left system Letter to subjects Read what you sign “I have reviewed the risks, benefits and alternatives of the study with the subject and answered all their questions satisfactorily.” This is a statement for a licensed personnel to sign such as a physician, physician’s assistant or advanced practice nurse—with study specific training documents on file 6
What if? Subject’s neutrophil count lower than protocol requirements for treatment. Treat and support with GCSF? Subsequent infection Renal function above parameters, hydrate and give Cyclosporine. Renal failure Under additional scrutiny when participating in research How Coordinators Support Subject Safety Confirm eligibility criteria are met prior to enrollment —document review and sign off by PI. Ensure any deviations from the eligibility are approved by the PI/sponsor and documented. Noncompliance may need to be reported; depending on institution. Ensure protocol evaluations are done; visit checklists, review labs. 7
Regulations Determination of risk and benefit is ongoing CFR 45 Part 46 IRB approval of research section 46.111 Risks to subjects are minimized…the research plan makes adequate provision for monitoring the data collected to ensure the safety of subjects… GCP 2.2 A trial should only be initiated and continued if the anticipated benefits justify the risks How Do We Know if the Risk Benefit Ratio has changed? By review of AE trends: change in the frequency or severity of the expected AE Outcome data. Study showed no difference between groups and hypothesis was a 20% difference in the new treatment Poor enrollment: is the study question going to be answered 8
Adverse Event Tracking Get a good baseline AEs can be Expected or Unexpected Review expected AEs to determine if trends indicate a change in the initial risk benefit ration DLTs will result in changes to the subject’s treatment plan and contribute to study stopping rules therefore real time AE collection is necessary PI review and sign off documented What is the protocol DSMP? Examples: Adverse experiences will be graded and recorded throughout the study according to NCI CTCAE, version 4.0. Toxicities will be characterized in terms including duration, intensity, and time to onset. Only grade 2 and higher adverse events or adverse events will be recorded. AEs will be collected until… 9
CTC V3 Grade 3 Neutropenia CRFs/Data Collection Priorities Baseline Eligibility checklist Adverse Events Log tracking stopping rules Study Drug/Intervention Response End of Study: is the subject evaluable Note: Not on the list: CRFs for labs, con meds. PI initiated studies: consider printing from ORCA and filing in research chart vs. transferring data to CRF 10
Reminder for studies with DSMB Coordinator Responsible for: Scheduling per protocol: failure to conduct DSMB meetings = noncompliance Maintain a log with meeting dates File minutes and submit to IRB/FDA Response and follow up Modification/Unanticipated event DSMB charter defines quorum, includes contact information and purpose of meeting Real Life: Don’t Try This at “Home” PI signs off on eligibility after the subject has been on study for a month Subject comes in for a study blood draw, PI not around to sign consent…coordinator signs for investigator Baseline liver function labs surprisingly show subject not eligible, unfortunately labs not verified prior to start of study procedures Glucose level is close enough to the protocol cut off of go ahead and treat Sterility test results are not available and the study drug is about to expire-proceed 11
Quiz A subject presents at the clinic who does not meet the protocol eligibility criteria. The coordinator A) Informs the PI, “(but) the protocol says…we will need to inform the IRB” B) When asked by the PI if the protocol will exclude the subject says, “I don’t know.” C) Says, “Whatever you think is best.” Compliance 12
Protocol Development Read the protocol for consistency between sections Identify operational issues –prepare lab requisitions Compare protocol, consent and contract to ensure consistency—important for billing too Meet with the PI to determine what procedures are standard of care and which are research Confirm eligibility criteria, stopping rules and cohort assignment plan with PI If you don’t Confusion about which instructions to follow: fuel for debate with monitors Noncompliance/Protocol Deviations to report Protocol Modifications to correct discrepancies and inconsistencies Compromise study data for missed labs Research billing errors 13
45 CRF 46 IRB is required to have written procedures that require the prompt reporting to the IRB of proposed changes in approved research activity, and for ensuring that such changes…may not be initiated without IRB review and approval EXCEPT to eliminate apparent immediate hazards to the subject OHRP Continuing noncompliance is reportable to outside government agencies Institutional lawyers care if you don’t follow the protocol 45 CRF 46: IRBs are required to have written procedures to ensure prompt reporting to the IRB, to the department or agency head of any unanticipated event that involves risk to subjects or others or any serious or continuing noncompliance with this policy or the requirements or determinations of the IRB 14
Recommend
More recommend