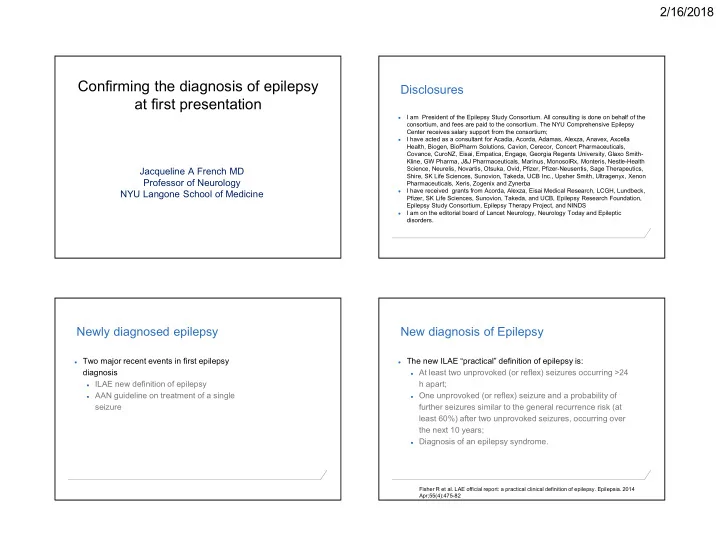
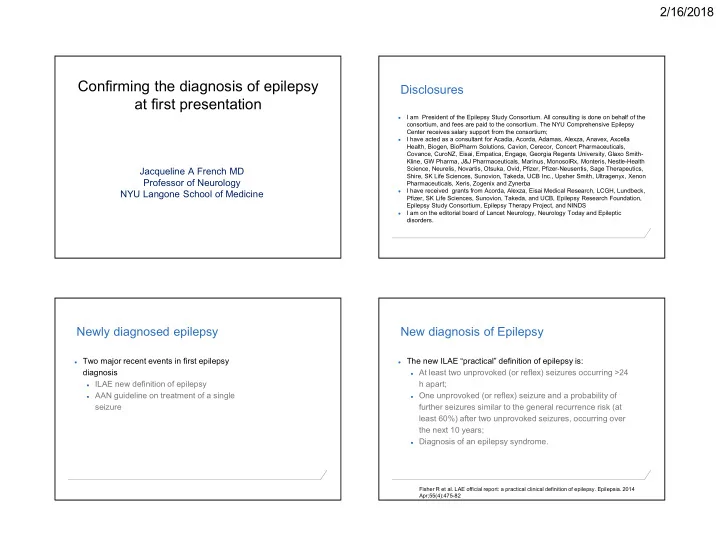
2/16/2018 Confirming the diagnosis of epilepsy Disclosures at first presentation I am President of the Epilepsy Study Consortium. All consulting is done on behalf of the ● consortium, and fees are paid to the consortium. The NYU Comprehensive Epilepsy Center receives salary support from the consortium; I have acted as a consultant for Acadia, Acorda, Adamas, Alexza, Anavex, Axcella ● Health, Biogen, BioPharm Solutions, Cavion, Cerecor, Concert Pharmaceuticals, Covance, CuroNZ, Eisai, Empatica, Engage, Georgia Regents University, Glaxo Smith- Kline, GW Pharma, J&J Pharmaceuticals, Marinus, MonosolRx, Monteris, Nestle-Health Science, Neurelis, Novartis, Otsuka, Ovid, Pfizer, Pfizer-Neusentis, Sage Therapeutics, Jacqueline A French MD Shire, SK Life Sciences, Sunovion, Takeda, UCB Inc., Upsher Smith, Ultragenyx, Xenon Professor of Neurology Pharmaceuticals, Xeris, Zogenix and Zynerba I have received grants from Acorda, Alexza, Eisai Medical Research, LCGH, Lundbeck, NYU Langone School of Medicine ● Pfizer, SK Life Sciences, Sunovion, Takeda, and UCB, Epilepsy Research Foundation, Epilepsy Study Consortium, Epilepsy Therapy Project, and NINDS I am on the editorial board of Lancet Neurology, Neurology Today and Epileptic ● disorders. Newly diagnosed epilepsy New diagnosis of Epilepsy ● Two major recent events in first epilepsy ● The new ILAE “practical” definition of epilepsy is: diagnosis ● At least two unprovoked (or reflex) seizures occurring >24 ● ILAE new definition of epilepsy h apart; ● AAN guideline on treatment of a single ● One unprovoked (or reflex) seizure and a probability of seizure further seizures similar to the general recurrence risk (at least 60%) after two unprovoked seizures, occurring over the next 10 years; ● Diagnosis of an epilepsy syndrome. Fisher R et al. LAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014 Apr;55(4):475-82 1
2/16/2018 New diagnosis of Epilepsy ● The new ILAE “practical” definition of epilepsy is: ● At least two unprovoked (or reflex) seizures occurring >24 h apart; ● One unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after two unprovoked seizures, occurring over the next 10 years; ● Diagnosis of an epilepsy syndrome. Fisher R et al. LAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014 Apr;55(4):475-82 AAN Guideline AAN Guideline ● Conclusion: Immediate antiepileptic drug (AED) therapy, as compared with ● ● Adults with an unprovoked first seizure should be informed delay of treatment pending a second seizure, is likely to reduce that sz recurrence risk is greatest early within the first 2 years recurrence risk within the first 2 years (Level B) (21%–45%) (Level A), and clinical variables associated with ● Clinicians’ recommendations whether to initiate immediate increased risk may include: AED treatment after a first seizure should be based on a prior brain insult (Level A), individualized assessments that weigh the risk of ● ● an epileptiform EEG (Level A), recurrence against the AEs of AED therapy. ● An abnormal CT/MRI(Level B) a nocturnal seizure (Level B). ● 2
2/16/2018 AAN and ILAE conclusion The fundamentals of diagnosis ● At the point of a treatment decision, there may be fewer (or even ● Treatment after a single seizure may be one) event(s), making diagnosis more difficult. Clinician should appropriate try to nail the diagnosis as early as possible ● Was it a seizure? ● If it was a seizure (or seizures), is it epilepsy? ● There is a major cost to patient and healthcare system of delay of diagnosis If it is not a seizure, what is it? How often is a seizure not a seizure? www.epilepsydiagnosis.org/epilepsy-imitators.html#overview ● It has been estimated that 5-10% of outpatients in epilepsy clinics PARASOMNIA and 20–40% of the patients admitted for video-EEG monitoring PSYCHOGENIC GI have NES (non-epileptic seizures), in both developed and STEREOTYPIES SLEEP D/O TIA developing countries PSYCH PAROXYSMAL BREATH-HOLDING DYSTONIA NEURO- LOGIC DYSKINESIA MIGRAINE ENDO- CRINE PHEOCHROMO CARDIO- TICS CYTOMA VASCULAR META- SYNCOPE BOLIC ARRHYTHMIA Asadi-Pooya AA, Sperling MR. Epidemiology of psychogenic nonepileptic HYPOGLYCEMIA seizures. Epilepsy Behav. 2015;46:60-5 3
2/16/2018 What is it? What is it? What is it? Delay to NES diagnosis at different ages Reuber et al, NEUROLOGY 2002;58:493–495 4
2/16/2018 What if there is no video-EEG? Was it a seizure? ● In actuality, most of the time, particularly early in the course of ● 12 y.o presents at the ED with headache, abdominal pain, after diagnosis, events are not frequent enough to capture on event last evening video-EEG ● Previous evening, pt was riding in car, felt nauseated, shaky. Mom ● In this case, asking the family to capture on phone video is reports patients speech was slurred and was having trouble getting often useful, but even then, the diagnosis may be difficult words out.; his "eyes looked shifty" and his hands were shaking. ● When even a phone video is not available, a diagnosis must He then "passed out" for a few minutes and was very sleepy. They rest on a precise history. got home and he was able to walk out of the car, speech still seemed slurred, was c/o abdominal pain. ● EEG, MRI, exam normal Was it a seizure? Was it a seizure? ● While out to dinner, child felt dizzy. She fell backward. She was stiff, was ● Pt rehearsing for her school performance and singing. She then went shaking, eyes rolled back with her pupils being dilated. Foaming at the silent and stopped singing. One minute later she was coming around and mouth was present. Child was rolled onto her left side and EMS was was able to answer questions appropriately. She states she remembers called. Post-ictal for 15 min, confused, disoriented. singing and then remembers coming to when she was sitting on the floor. No loss of tone, bowel or bladder incontinence. ● Then shortly after while at the ER, child proceeded to the following. Per Dr. XYZ note (ED physician): "She had right sided facial grimacing her head ● Four other episodes- She will suddenly stop her activity and stare turned to the right. Her eyes deviated to the right and her head went back straight ahead. She does not have any abnormal movements with this. and then her right arm started. Then (right arm) extending and having She is able to follow instructions to sit down. Episodes will last from 30 generalized tonic-clonic movements and then the left arm did so and was seconds to max 1 minute and then resolve. Afterwards, she is confused definitely a progression from a partial onset seizure. and will take 5-10 minutes to return to baseline. 5
2/16/2018 Epilepsy Behav. 2014 Dec;41:197-202 Epilepsy Behav. 2014 Dec;41:197-202 Epilepsy Behav. 2014 Dec;41:197-202 Epilepsy Behav. 2014 Dec;41:197-202 Even observed seizure semiology may not be Was it a seizure? diagnostic ● EEG: Left hemispheric slowing and epileptiform activity consistent ● 8 Epileptologists, 12 neurologists with focal left hemisphere cerebral dysfunction. and 20 internists watched 150 videos of epileptic seizures, ● MRI bilateral occipital gray matter heterotopia more pronounced psychogenic non-epileptic on the left than on the right. seizures, and non-epileptic physiologic events ● Epileptologists performed the best, and accuracy improved as more events were observed Jin et al, Epilepsy Behav 2014 41:197-202 Don’t ask-Won’t tell Structured interview form may help ● As evidenced in the examples, presence of certain seizure ● DISCOVER (Diagnostic Interview Conducted Outside Video EEG characteristics (eg forced head turning,vocalizations, salivation, Recording)-Structured interview that can be used to ensure oral automatisms, etc), can increase the diagnostic certainty of a important characteristics are queried. seizure ● Has been used for all patients enrolled in HEP ● However, families/observers may not describe these features ● Both subject and observer (if available) are interviewed unless they are asked for them. ● Allows for more precise diagnosis to confirm epilepsy as well ● Even physician observers may not describe these if they are not as seizure type prompted to Friedman et al, Neurology February 12, 2013; 80 (7 Supplement) 6
Recommend
More recommend