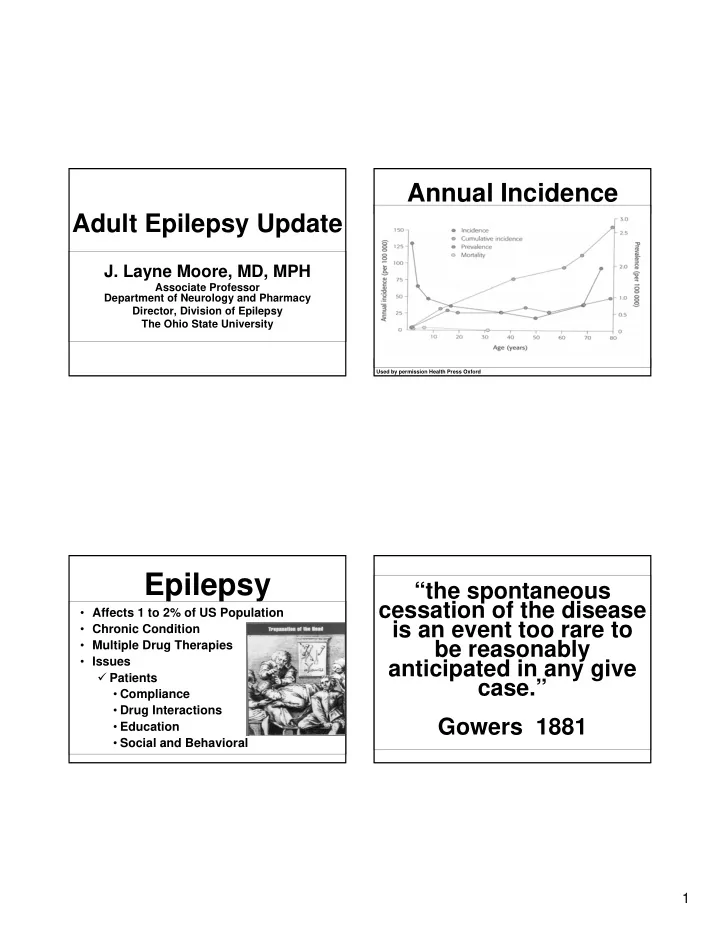
Annual Incidence Adult Epilepsy Update J. Layne Moore, MD, MPH Associate Professor Department of Neurology and Pharmacy Director, Division of Epilepsy The Ohio State University Used by permission Health Press Oxford Epilepsy “the spontaneous cessation of the disease • Affects 1 to 2% of US Population is an event too rare to • Chronic Condition be reasonably • Multiple Drug Therapies • Issues anticipated in any give � Patients case.” • Compliance • Drug Interactions Gowers 1881 • Education • Social and Behavioral 1
Newly Diagnosed Refractory Epilepsy (n=470) 1 st drug Seizure-free 47% (n=222) Uncontrolled 53% • What is refractory epilepsy? (n=248) � Uncontrolled with multiple medications Seizure-free 13% 2 nd drug (n=61) � Intolerable side-effects to achieve control Uncontrolled 40% (n=187) 3 rd drug • How to fight back? Seizure-free 4% (n=18) Uncontrolled 36% (n=169) Kwan & Brodie NEJM 2000 Which patients respond? • Early response in key • Response to the 1 st drug � 11% response to 2 nd drug if 1 st was ineffective � 41% for SE � 55% idiosyncratic reaction Kwan and Brodie 2
Seeking a Cause • For most persons with epilepsy or seizures no cause is found • People without a clear cause have the best prognosis. Risk Ratios for Selected Causes Alzheimers 10 Encephalitis 16 2 Aseptic Meningitis HTN LVH 7.3 Risk Ratio Stroke 20 Mild HI 1.5 Moderate HI 4 Severe HI 29 Baseline 1 0 5 10 15 20 25 30 35 3
Seizure or Spell Diagnostic Pitfalls Evaluation • Careful history hopefully with collateral • Is the diagnosis correct? history • Does the patient have epilepsy? � Past Medical History • Risk factors • Neurological examination • EEG • Neuroimaging Our Differential Seizure Evaluation Diagnoses • Syncope • EEG � Often prominent autonomic symptoms � Awake and asleep increase sensitivity • Seizure � Looking for evidence of epilepsy • An “aura” is a seizure � symptoms may be positive, negative, or mixed * Less than 2% of normal people have • pSychogenic spell epileptiform discharges � Almost anything goes • Evidence of focal-onset vs. • other Stuff generalized-onset seizure � cataplexy • This will dictate our choice of AEDs � migraine � TIA 4
Seizure Evaluation • Neuroimaging � MRI with thin coronal cuts through hippocampus � CT scan is only indicated if: • Patient has contraindications to MRI • It is emergent to look for a bleed or mass effect MTS Sleep Stages • Awake • Stage I Most Interictals • Stage II Seizures • Stage III • Stage IV • REM 5
Older Drugs Strategies for Management of Epilepsy • Dilantin (Phenytoin) PHT • Phenobarbital • Medication • Tegretol, Carbatrol (Carbamazepine) CBZ � Partial • Depakote, Depakene (Valproic Acid) VPA � Generalized � Bones loss • Resective Surgery • Aging population, post-menopausal • Vagal Nerve Stimulator women � Hormonal birth control failure (except VPA) • Ketogenic Diet/ Atkins Diet • And may decrease the levels of other AEDs • Stimulators � High protein binding displacing drugs like coumadin and synthroid 2 nd Generation Drugs Antiepileptic Drug (AED) Therapy • Neurontin (Gabapentin) TGB Long-Term Management • Felbatol (Felbamate) TPM Strategies for Epilepsy FOS ZNS • Lamictal (Lamotrigine) LTG LVT GBP CBZ VPA OCBZ • Topamaz (Topiramate) PB PHT FBM PGB • Gabitril (Tiagabine) 1900 1920 1940 1960 1980 2000 � No enzyme induction 1st Generation 2nd Generation � Low protein binding � Less interference with other drugs 6
3 rd Generation Drugs The End • Trileptal (Oxcarbazepine) • Zonegran (Zonisamide) • Keppra (Leviteracitam) • Lyrica (Pregabalin) � Little interaction with other drugs � Renal excretion Newly Diagnosed (n=470) 1 st drug Seizure-free 47% Pediatric Epilepsy (n=222) Uncontrolled 53% (n=248) 2 nd drug Seizure-free 13% Jorge Vidaurre M.D. (n=61) Director Epilepsy Center Uncontrolled 40% (n=187) 3 rd drug Nationwide Children’s Hospital- OSU Seizure-free 4% (n=18) Uncontrolled 36% (n=169) Kwan & Brodie NEJM 2000 7
Epilepsy: Epilepsy Incidence/100,000 200 • Convulsive disorders are among the most frequently occurring 181,000 new 150 neurological condition in children Cases Per year 100 50 0 0 20 40 60 80 100 Age Hauser, Epilepsia 33:1992 Causes of Childhood- Incidence Acquired Epilepsy Tumors Trauma • Incidence of seizures is higher in Poison childhood, especially the first year of life (100/100,000) and in older patients Birth injury 45%-55% 45%-55% Genetic or Prematurity idiopathic Infection Metabolic Disturbances Fever 8
Non-epileptic paroxysmal Definitions events in childhood • Seizure: Clinical manifestation of an • Syncope abnormal, excessive activity of a set of • Breath-holding spells cortical neurons • Movement disorders (tics) • Epilepsy: Chronic brain disorder of • Sleep disorders (parasomnias, night various etiologies characterized by terrors, sleep walking) recurrent, unprovoked seizures • Day dreaming, inattentiveness & distractibility • Epilepsy syndromes: Grouping of similar patients according to seizure type EEG, age • Self stimulatory behavior of onset, familial episodes, prognosis, and • Gastroesophageal reflux other clinical signs • Psychogenic Breath Holding Was the Event a Event Video Seizure? 9
Benign Rolandic Epilepsy Seizure Classification (BRE) • Partial seizures: originating in a focal area of the brain. • One of the most frequent syndromes, occurring in up to 24% of all epileptic � Simple: Do not impair consciousness seizures in children between ages 5 and 14 � Complex: Impairment of consciousness • Age of presentation: 3- 13 year • Generalized seizures • Remission rate almost 100% at age 16. � Absences, clonic, tonic, tonic-clonic, • Seizures are usually infrequent. atonic and myoclonic Benign Rolandic Epilepsy (BRE) Benign Partial • Seizures usually occur during sleep Epilepsies of • Partial sensorimotor: hemi facial twitching, drooling , arrest of speech, Childhood numbness of tongue, lips. • GTC in 20-30% of cases 10
BRE Video Idiopathic Generalized Epilepsies 11
Childhood Absence Epilepsy (Pyknolepsy, Petit Mal Epilepsy) • “Very frequent (several to many per day) absence seizures” • Brief in duration (usually 5-30 seconds) • Sudden behavioral arrest, with staring and quick return to normal baseline activities • “Otherwise normal child” Childhood Absence Epilepsy (Pyknolepsy, Petit Mal Epilepsy) • Often precipitated by hyperventilation Absence Video • An EEG demonstrating “bilateral, synchronous spike-waves, usually 3 HZ, on a normal background activity” 12
Commonly used Juvenile Myoclonic Epilepsy(JME) Medications • Ethosuxamide • Seizures are precipitated by sleep deprivation, alcohol, stress. • Valproic acid • Photosensitivity • Lamotrigine • Intelligence remain normal Juvenile Myoclonic Epilepsy(JME) • Age of onset: 8-24 years. Peak between Myoclonus video 12-18 years • The characteristic seizure type is Child during sleep “myoclonus”, usually affecting shoulders • GTC seizures appear usually more than 3 years after myoclonus. • Absences occur in up to 30% of patients. 13
Symptomatic Generalized Epilepsies Photic Induced • Infantile spasms Seizure • Lennox Gastaut syndrome Medications used for Infantile Spasms JME • Age of onset: 4-6 months • Broad spectrum medications: • Types: flexor (Jackknife, salaam attacks) , • Valproic Acid extensor or mixed. • Lamotrigine • Usually occur in cluster, during awakening • Topiramate or falling sleep • Levetiracetam • Usual EEG shows hypsarrhythmia interictaly. Most frequent ictal • Medications that can worsen seizures: manifestation: ”electrodecremental • Phenytoin, carbamazepine response” 14
Hypsarrhythmia Sleep West Syndrome • Infantile spasms • Hypsarrhythmia • Mental retardation Ictal Event: IS Hypsarrhythmia-Wakefulness 15
Recommend
More recommend