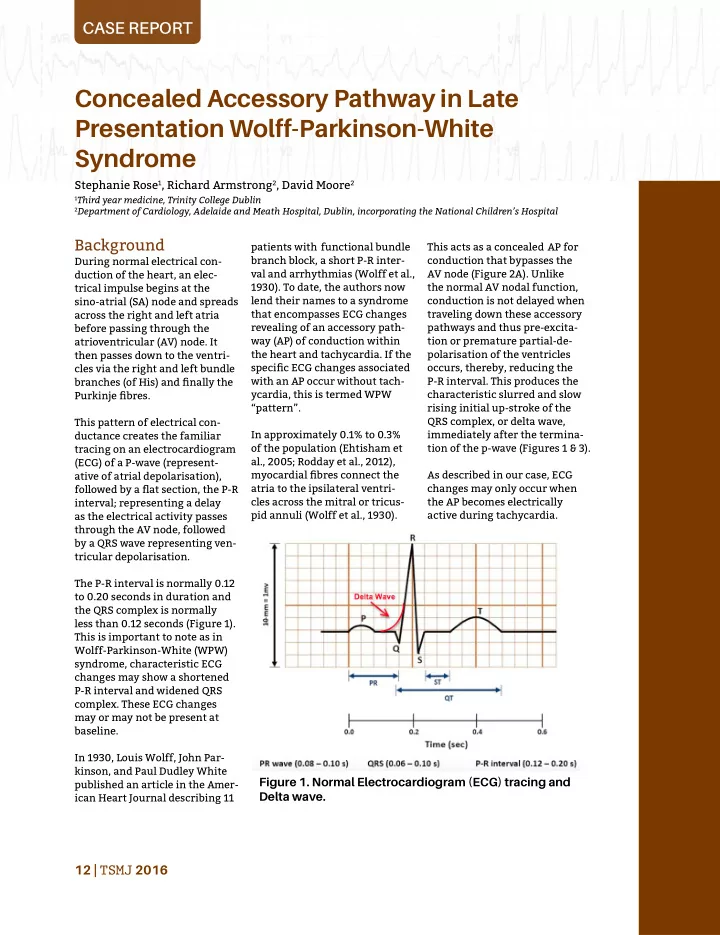
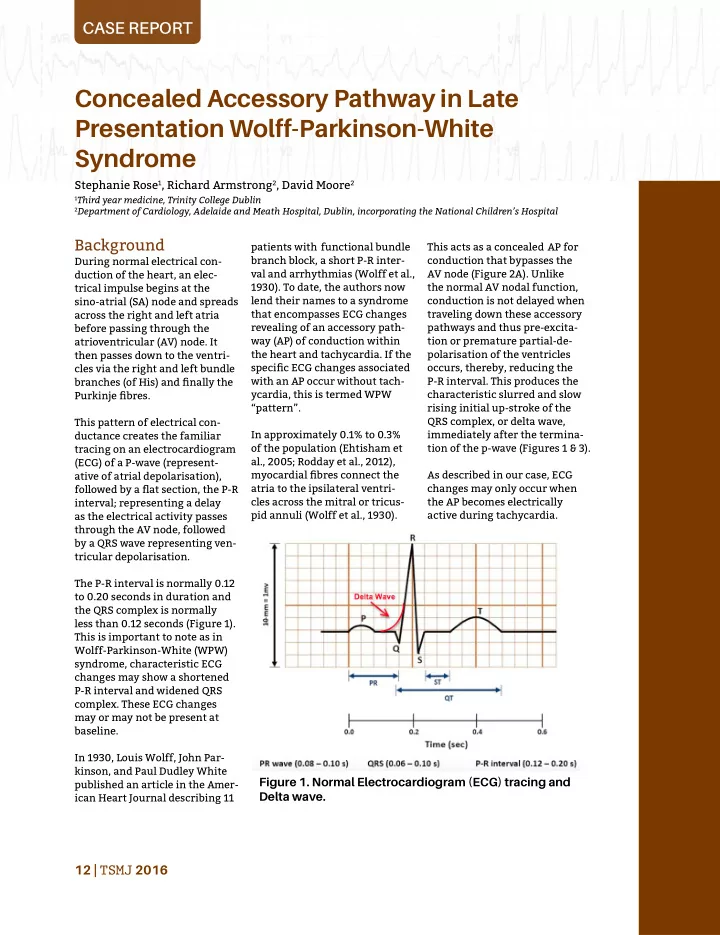
CASE REPORT Concealed Accessory Pathway in Late Presentation Wolff-Parkinson-White Syndrome Stephanie Rose 1 , Richard Armstrong 2 , David Moore 2 1 Third year medicine, Trinity College Dublin 2 Department of Cardiology, Adelaide and Meath Hospital, Dublin, incorporating the National Children’s Hospital Background patients with functional bundle This acts as a concealed AP for branch block, a short P-R inter- conduction that bypasses the During normal electrical con- val and arrhythmias (Wolff et al., AV node (Figure 2A). Unlike duction of the heart, an elec- 1930). To date, the authors now the normal AV nodal function, trical impulse begins at the sino-atrial (SA) node and spreads lend their names to a syndrome conduction is not delayed when that encompasses ECG changes traveling down these accessory across the right and left atria revealing of an accessory path- pathways and thus pre-excita- before passing through the way (AP) of conduction within tion or premature partial-de- atrioventricular (AV) node. It the heart and tachycardia. If the polarisation of the ventricles then passes down to the ventri- specific ECG changes associated occurs, thereby, reducing the cles via the right and left bundle with an AP occur without tach- P-R interval. This produces the branches (of His) and finally the ycardia, this is termed WPW characteristic slurred and slow Pu rkinje fibres. “pattern”. rising initial up-stroke of the QRS complex, or delta wave, This pattern of electrical con- In approximately 0.1% to 0.3% immediately after the termina- ductance creates the familiar of the population (Ehtisham et tion of the p-wave (Figures 1 & 3). tracing on an electrocardiogram al., 2005; Rodday et al., 2012), (ECG) of a P-wave (represent- ative of atrial depolarisation), myocardial fibres connect the As described in our case, ECG atria to the ipsilateral ventri- changes may only occur when followed by a flat section, the P-R cles across the mitral or tricus- the AP becomes electrically interval; representing a delay pid annuli (Wolff et al., 1930). active during tachycardia. as the electrical activity passes through the AV node, followed by a QRS wave representing ven- tricular depolarisation. The P-R interval is normally 0.12 to 0.20 seconds in duration and the QRS complex is normally less than 0.12 seconds (Figure 1). This is important to note as in Wolff-Parkinson-White (WPW) syndrome, characteristic ECG changes may show a shortened P-R interval and widened QRS complex. These ECG changes may or may not be present at baseline. In 1930, Louis Wolff, John Par- kinson, and Paul Dudley White Figure 1. Normal Electrocardiogram (ECG) tracing and published an article in the Amer- Delta wave. ican Heart Journal describing 11 12 | TSMJ 2016
Accessory AVN pathway SA Node Accessory pathway ¡ Figure 2. (A) A physiological mechanism of conduction in WPW with accessory pathway conduction (atrioventricular) resulting in the delta wave. (B) Orthodromic conduction in WPW syndrome occurring down AVN and retrogradely up accessory pathway. (C) Anti- dromic conduction where accessory pathway conducts anterogradely (atrioventricular) and the impulse returns to the atria via the AVN. (D) mechanism of AF in WPW syndrome. Therefore there are no ECG antidromic reciprocating tach- ing indoors on a ladder. The changes at baseline and this ycardia (Figure 2C). This occurs pain was continuous, dull and can be described as a concealed in only 5-10% of cases (Blom- described as a central tightness AP (Kulig et al., 2010). If ECG ström-Lundqvist et al., 2003). across the chest radiating to changes are present at baseline Lastly, the AP may lead to atrial the left neck and shoulder. Her this is described as a manifest fibrillation (Figure 2D). These subjective pain score was 8/10. pathway. These APs (Figure 2) arrhythmia experienced in WPW The pain worsened on inspira- may permit atrioventricular patients are potentially fatal and tion and there were no allevi- re-entrant tachycardia (AVRT), a summary of risk factors, signs ating factors. Other presenting whereby electrical conduction and symptoms, ECG findings, symptoms were pre-syncope, travels as a circuit from the and investigations can be found atrium to the ventricles and weakness, and numbness on the in Table 1. back to the atrium resulting in left side of the tongue. repeated AV nodal stimulation, Case Presentation inducing tachycardia. This The patient had slowly walked Here we describe a case of a accounts for 95% of re-entrant for nearly an hour to her Gen- concealed accessory pathway in tachycardias in WPW patients eral Practitioner who called an a 64 year old lady who presented (Blomström-Lundqvist et al., ambulance and administered to cardiology in 2015 with acute 2003). sublingual glyceryl trinitrate chest pain, palpitations and shortness of breath on a back- without symptomatic relief. Most commonly, the electrical ground of heavy smoking (10 Of note, the patient’s previous impulse travels to the ventricles pack years), high cholesterol, via the AV node and back to medical history revealed two type 2 diabetes mellitus and the atria via the AP in a retro- previous admissions to A&E for aortic regurgitation. grade manner. This is classified chest pain in 2006/2007 which as orthodromic reciprocating had been excluded as cardiac in On admission, the patient was tachycardia, and no delta wave origin by the cardiology team apyrexial with a blood pressure is seen on ECG investigation following negative blood tests, of 118/67, a pulse rate of 100/ (Figure 2B). a normal 24 hour Holter ECG, min and respiration rate of 15. and two non-revealing stress If the electrical impulse antero- The initial symptom of chest tests achieving 96% of her target pain occurred at 11am in the gradely travels to the ventricles heart rate. via the AP and returns via the morning following mild to AV node, this is classified as moderate exertion whilst paint- TSMJ 2016 | 13
CASE REPORT Table 1. Summary of most common structural risk factors, signs and symptoms, ECG findings (not always present) and possible investigations in WPW syndrome 12 lead ECG findings Signs and Additional Risk Factor indicative of WPW symptoms Investigations syndrome Ebstein’s Anomaly; Palpitations Shortened P-R interval Echocardiogram The most commonly of <0.12 s occurring congenital Dizziness Treadmill test defect associated with A prolonged QRS WPW syndrome. It Dyspnoea complex >0.11 s Pharmacological involves malformation testing with of the tricuspid valve Atrial Flutter Delta Waves procainamide or and may lead to (bidirectional AP) ajmaline may define cyanosis, dyspnoea, Atrial Fibrillation duration of anterograde fatigue, arrhythmias, No delta waves effective refractive and congestive heart Syncope or (retrograde AP) period of the accessory failure. presyncope pathway. Tachycardia Electrophysiological Study Sudden cardiac death ECG Findings tachyarrhythmias is given in performed to rule out coronary Table 2 and in this clinical sit- artery disease. As represented in The appearance of the 12 lead ECG on admission revealed a uation, the Brugada Criteria Figures 6 and 7, very mild arte- (Figure 5) provides a flow chart rial disease within the right and wide QRS complex and regu- to the clinician that may be used left coronary arteries was found, lar monomorphic ventricular to ascertain whether or not the tachycardia (VT) (Figure 3). mainly at the bifurcations and tachyarrhythmia is ventricular not in keeping with the signs The patient was diagnosed by or supraventricular in origin. the clinician on-call as having and symptoms experienced by the patient. Both the coronary monomorphic unstable VT and Investigations emergency direct current (DC) angiogram and transthoracic cardioversion was delivered as a Throughout the patient’s admis- echocardiogram did not reveal synchronised shock. The patient sion, blood tests were non-re- any structural abnormalities. was then converted to sinus vealing for any indication of Following coronary angiogra- rhythm (Figure 4). A differen- ischaemia or other pathology. phy, delta wave ECG changes tial diagnosis for wide complex A coronary angiogram was were detected, allowing for Table 2. Differential Diagnosis of Wide Complex Tachyarrhythmias Supraventricular Tachycardia With Bundle branch block can occur with any Bundle Branch Block supraventricular arrhythmia May occur during atrial flutter, atrial fibrillation, Supraventricular Tachycardia With atrioventricular nodal reciprocating tachycardia Atrioventricular Conduction Over an (AVNRT), atrioventricular reciprocating tachycardia Accessory Pathway (AVRT), and atrial tachycardia Ventricular Tachycardia May be diagnosed using Brugada Criteria 14 | TSMJ 2016
Regular monomorphic tachycardia Appearance of possible fusion of wide and narrow complex tachycardia Figure 3. ECG on admission: Wide complex regular tachyarrhythmia showing delta waves (arrows) and right bundle branch block pattern.
Recommend
More recommend