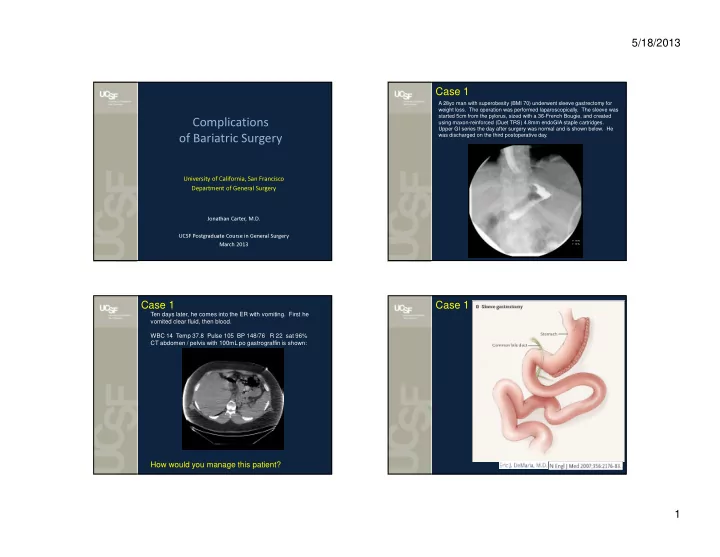
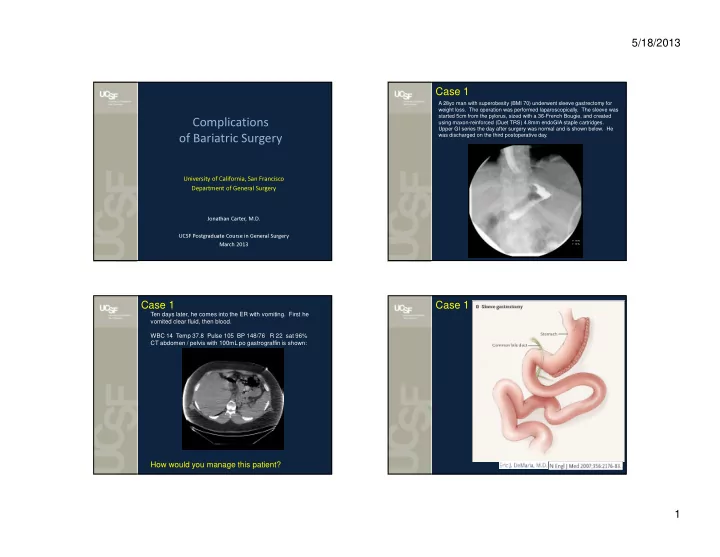
5/18/2013 Case 1 A 28yo man with superobesity (BMI 70) underwent sleeve gastrectomy for weight loss. The operation was performed laparoscopically. The sleeve was started 5cm from the pylorus, sized with a 36-French Bougie, and created using maxon-reinforced (Duet TRS) 4.8mm endoGIA staple cartridges. Complications Upper GI series the day after surgery was normal and is shown below. He was discharged on the third postoperative day. of Bariatric Surgery University of California, San Francisco Department of General Surgery Jonathan Carter, M.D. UCSF Postgraduate Course in General Surgery March 2013 Case 1 Case 1 Ten days later, he comes into the ER with vomiting. First he vomited clear fluid, then blood. WBC 14 Temp 37.8 Pulse 105 BP 148/76 R 22 sat 96% CT abdomen / pelvis with 100mL po gastrograffin is shown: How would you manage this patient? 1
5/18/2013 Case 1 Case 1 The patient underwent laparoscopic re-exploration A hole adjacent to the staple line, possible created from the Duet, was identified near the GEJ. A latex T-tube was placed in the hole and externalized. Adjacent JP drains were placed. A feeding jejunostomy tube was placed. The fistula healed completely within 3 months. Case 2 Case 2 A 36 year old woman with BMI 54 underwent sleeve gastrectomy 5 months prior. She presented to the ER with failure to thrive and vomiting. She says she can only hold down 3 bites of food. Any more, she vomits. She was initially managed by a gastroenterologist. EGD x 2 showed “normal” sleeved stomach without twist or obstruction. There was mild esophageal dilation. The endoscope passed easily into the duodenum. Hyoscyamine and Reglan were trialed with no benefit. Diagnosis: sleeve stricture CT scan showed a sleeved stomach. Her albumin is 2.6 She has been on TPN Treatment: What would be your next diagnostic test? conversion to RYGB (standard) …or seromyotomy: 2
5/18/2013 Case 3 Case 3 63 yo man with LapBand placed 2 years ago. The balloon was known to contain 8cc. Three months ago, he developed reflux and a hoarse voice and was started on pepcid. He developed intolerance to solid food but was tolerating liquids until 3 days prior when he began having emesis. He has lost 15 lbs over the past 20 days. EGD: "bulging" at the band site and esophagitis. Diagnosis? Case 3 Case 4 A confirmatory upper GI series was obtained: A 45 year old woman underwent LapBand placement 3 years ago for a BMI 43. She lost 53 pounds and has been well. Her last adjustment (band fill) was 15 months ago. She presents with a port-site infection. Diagnosis? Diagnosis: slipped LapBand (anterolateral) Treatment: reoperative to either remove or reposition the band 3
5/18/2013 Case 4 Case 6: Stumper! Upper endoscopy was performed: 38 year old woman presents with dysphagia and malnutrition after gastric bypass 7 years prior. She weighs 92 pounds. A 5mm stricture of the gastrojejunostomy was diagnosed by upper endoscopy. It was serially dilated to 15mm, but there was no improvement in the dysphagia. An upper GI series was obtained: Diagnosis: LapBand erosion Diagnosis? Treatment: surgically remove band Case 5 Summary of Most Common Complications Bypass Sleeve Band stricture of gastrojejunostomy (2-3%) stricture at incisura (0-4%) acute pouch obstruction (0-10%) treatment: dilation during endoscopy treatment: dilation, hyoscyamine, treatment: nasogastric tube myotomy or conversion to bypass marginal ulceration (3-5%) GERD (up to 40%) band erosion (0-7%) treatment: antacids treatment: acid blockers treatment: surgery to remove band gallstone disease (2% with prevention) gallstone disease (2% with gallstone disease (2% with prevention) VIDEO prevention) prevention: ursodiol for 6 months prevention: ursodiol for 6 months prevention: ursodiol for 6 months treatment: remove gallbladder treatment: remove gallbladder treatment: remove gallbladder internal hernias with obstruction (0-5%) micronutrient deficiency (??) port infection (0.3-9%) treatment: surgery treatment: supplementation treatment: surgery to remove port leak (0.3-4%) leak (0.2-4%) band slippage (2-14%) treatment: drainage, feeding tube treatment: drainage, feeding tube treatment: surgery to remove/reposition band micronutrient deficiency (0-15%) port or tubing malfunction (0.4-7%) treatment: supplementation treatment: surgery to fix malfunction reflux or esophageal dilation (0-10%) treatment: antacids or band removal psychological intolerance (0-5%) treatment: removal of band 4
Recommend
More recommend