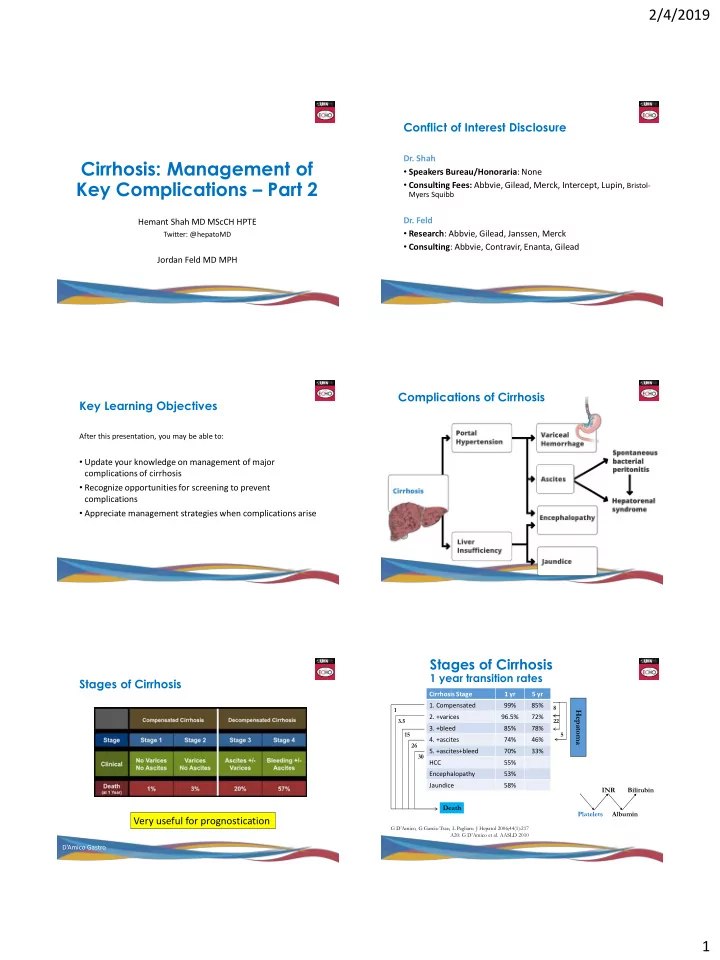
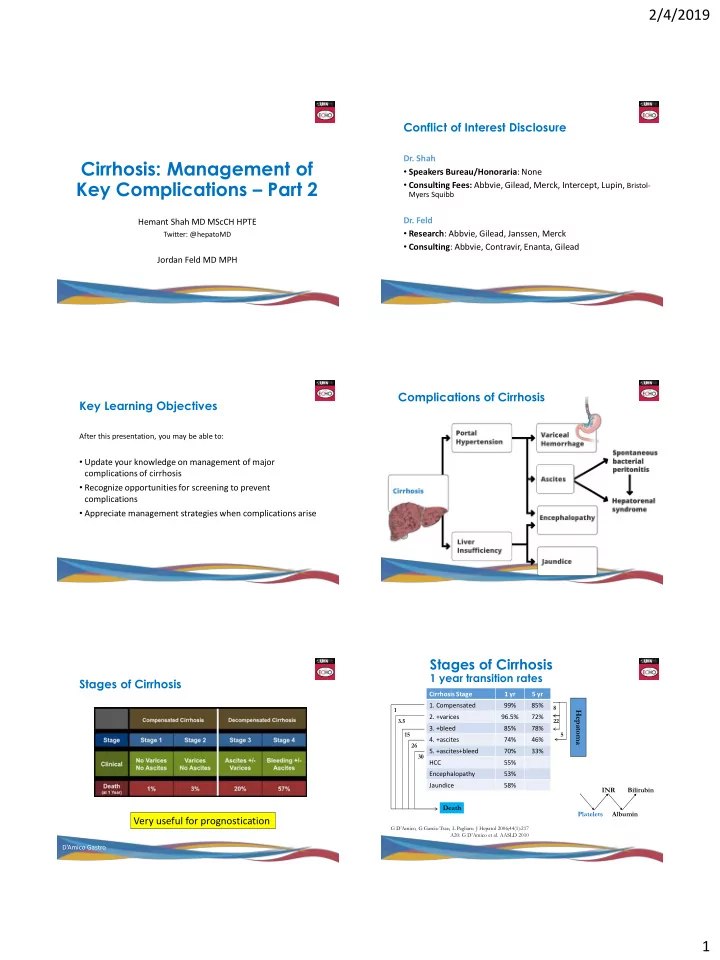
2/4/2019 Conflict of Interest Disclosure Dr. Shah Cirrhosis: Management of • Speakers Bureau/Honoraria : None Key Complications – Part 2 • Consulting Fees: Abbvie, Gilead, Merck, Intercept, Lupin, Bristol- Myers Squibb Dr. Feld Hemant Shah MD MScCH HPTE • Research : Abbvie, Gilead, Janssen, Merck Twitter: @hepatoMD • Consulting : Abbvie, Contravir, Enanta, Gilead Jordan Feld MD MPH Complications of Cirrhosis Key Learning Objectives After this presentation, you may be able to: • Update your knowledge on management of major complications of cirrhosis • Recognize opportunities for screening to prevent complications • Appreciate management strategies when complications arise Stages of Cirrhosis 1 year transition rates Stages of Cirrhosis Cirrhosis Stage 1 yr 5 yr 1. Compensated 99% 85% 8 1 Hepatoma 2. +varices 96.5% 72% 3.5 22 3. +bleed 85% 78% 15 5 4. +ascites 74% 46% 26 5. +ascites+bleed 70% 33% 30 HCC 55% Encephalopathy 53% Jaundice 58% INR Bilirubin Death Platelets Albumin Very useful for prognostication G D’Amico, G Garcia -Tsao, L Pagliaro. J Hepatol 2006;44(1):217 A20: G D’Amico et al. AASLD 2010 D’Amico Gastro 1
2/4/2019 Issues in Cirrhosis Management Ascites • Ascites • SBP Prophylaxis • Varices • Encephalopathy • Hepatocellular Cancer • Others Management of Ascites Sodium Balance 1) Salt restriction - (66 mmol/d – 1.5-2 g/d) Intake Output 2) Salt restriction – dietitian available – EatRight Ontario 3) Salt restriction! 4) Avoid Doctors -- NSAIDs, surgery, saline 100-150 mmol/d <20 mmol/d 5) Diuretics 6) Fluid restriction – only once hyponatremic Typical No Added Typical Urinary Na + Excretion of ascitic Salt Diet 7) Paracentesis Pt on no diuretics 8) TIPS 9) Transplant - All patients should be evaluated Result? Daily positive Na + Balance of 80-130 mmol/d = 600-1000ml fluid/d Diuretics Urine electrolytes • International Ascites Club - Recommend combo therapy: • Useful if refractory ascites despite ‘adhering’ to low salt diet or on lots of diuretics • Goal is to measure sodium output, and then compare to sodium Spironolactone 100 mg/d + Furosemide 40 mg/d input - With stepwise increase to max 400 + 160mg/d • Two ways to measure: - Check lytes/creat with every change • Spot Urine: - If issues with gynecomastia – change spironolactone • Sodium-potassium ratio >1 is 90% predictive of Na excretion greater than to amiloride (10 mg = 100 mg) 78mmol/d • 24hr Urine: • If done correctly, accurate sodium-excretion Aim = 0.3-0.5 kg/d (1lb/d) without edema 0.8-1 kg/d (2lb/d) w/ edema 2
2/4/2019 Refractory Ascites Interpreting Urine Sodium • Occurs 5-10% of patients with ascites If ascites difficult to manage (high-dose diuretics) and: • Definition: No response to Spironolactone 400 mg + Low urine sodium Sodium-retainer, stop diuretics, may need paracentesis Furosemide 160 mg/d or diuretic intolerance Moderate-High urine sodium Sodium-excreter, consuming • Check compliance too much sodium, work on diet - if excreting > 78 mmol/d and gaining wt CHEATING! - Rule out other causes -- tumor, PV thrombosis etc Bad Prognosis Options in Refractory Patients 1. Repeated large volume paracentesis + albumin 2. TIPS 3. Peritonvenous shunt - Abandoned due to high complications Gines NEJM 1991 Worse than almost any cancer! Gines NEJM 2004 Large volume taps Spontaneous Bacterial Peritonitis - SBP • Key is remember to check! • Effective but high rate of recurrence • 50% have no symptoms – no fever, no pain • Patients often prefer paracentesis to diet + diuretics • Complications of protein/complement loss, infection • Rule: If someone with ascites presents to medical attention for etc prove diuretic resistant!! ANY reason…they need a tap to r/o SBP • This is VERY poorly done at ALL hospitals • Replace albumin if >5L removed • Can be literally life-saving • If require > 8L q 2 weeks -- non-compliant • Cell count (neutrophils>250 or WBC>500) + culture in blood culture bottles • Low risk of SBP if no symptoms, therefore cell count, • After an episode of SBP – long-term prophylaxis but cultures not necessa • Norfloxacin 400 mg daily or • Ciprofloxacin 750 mg once per week 3
2/4/2019 Albumin and SBP Varices • Excellent evidence that giving high-dose albumin in setting of SBP decreases mortality (19% @ 3 months) • Dose: • 1.5mg/kg on day 1 • 1 mg/kg on day 3 • A lot of albumin! • For 70kg person, that ’ s 7 bottles of 25% albumin Sort et al. NEJM. 1999; 341:403-409 . Beta blockers vs Banding for Primary Variceal screening Prophylaxis • Guidelines recommend every 2-3 years once cirrhosis diagnosed • Multiple trials - both better than placebo • Not required if primary disease taken away e.g. HCV after SVR – no • Mostly methodologically flawed (often significantly) need for endoscopy if no varices prior to SVR • Once present – may consider increasing to annual surveillance • Generally show a small benefit of banding over beta blockers for patients with big varices (grade 3 or 4) • If being selective: • Guidelines still suggest beta blockers – cost + safety • Fibroscan< 20 Kpa AND Platelets > 150 very low risk of varices that • If beta blockers not tolerated or very big varices require treatment and can forego endoscopy band first • Once on a beta blocker no need to keep scoping! • Aim for HR<60 bpm When they do Bleed - Managing Varices • Banding superior to beta blockers – repeat sessions q 4 weeks until eradicated • TIPS is an effective rescue therapy for bleeding • Methods: Garcia-Pagan et al. 2010 • Group 1: EBL + Medical Mgt w TIPS as rescue • Group 2: Diagnostic Endo + TIPS w/in 72hrs • e-PTFE-covered stents (dilated to 8 mm) • If portal-pressure gradient >12 mmHg stent dilated to 10 mm • Primary Endpoint: Failure to control bleeding or re-bleeding within 1 year 4
2/4/2019 A clear benefit for early TIPS Encephalopathy Variceal bleed randomized to early TIPS (<72 h) vs standard care after octreotide + banding 86% 97% 42 DAYS ARR=30%; NNT=3.3 CI 2.1-8.3) 67% 12 MONTHS 61% ARR=25%; NNT=4.0 (CI 2.1-50.0) • Very strong effect on rebleeding and survival • Under-utilized in Toronto! Garica-Pagan NEJM 2010 Encephalopathy Primary Outcome – Breakthrough First HE • ‘Brain fog’ from liver disease • Liver clears nitrogenous waste • With shunting – waste products to the brain • Mild to severe symptoms • Asterixis – rarely focal neuro deficits, Parkinsonism • Treatment: • Avoid precipitants – meds, infection, bleeding Hazard Ratio 0.42, p<0,001 • Lactulose • Laxative – changes rectal pH to change bacterial flora to decrease ammonia producing bugs • Others may work – recent study with PEG – I’m skeptical • Rifaxamin • Non-absorbable antibiotic – similar effect, no diarrhea • Now covered by ODB (LU code) • Driving…you don’t want them on the road… Bass et al. NEJM. 2010; 326: 1071-1081. Other Issues for Cirrhotics Summary • Hepatocellular cancer screening • Main complications: • US q 6months • Ascites • AFP recommendation back to equivocal • Salt restriction, diuretics, screen for SBP! • Caveats: High if active hepatitis, often low in small HCCs – limits • Varices sensitivity and specificity but still may be useful • Can avoid screening if FS<20 & Plt>150 • Particularly: Post- SVR for HCV, if you don’t trust your ultrasound! • Encephalopathy • Vaccinations – ALL (remember annual flu) • Reverse ppt, lactulose, rifaximin, driving • Infections • Cancer • low threshold to treat…sepsis is VERY common cause of • Surveillance with US +/- AFP death…renal function very tenuous • Findings may be subtle (normal WBC but high for cirrhosis) • Screen for problems and try not to precipitate them! • Statins and Anticoagulation - Emerging 5
Recommend
More recommend