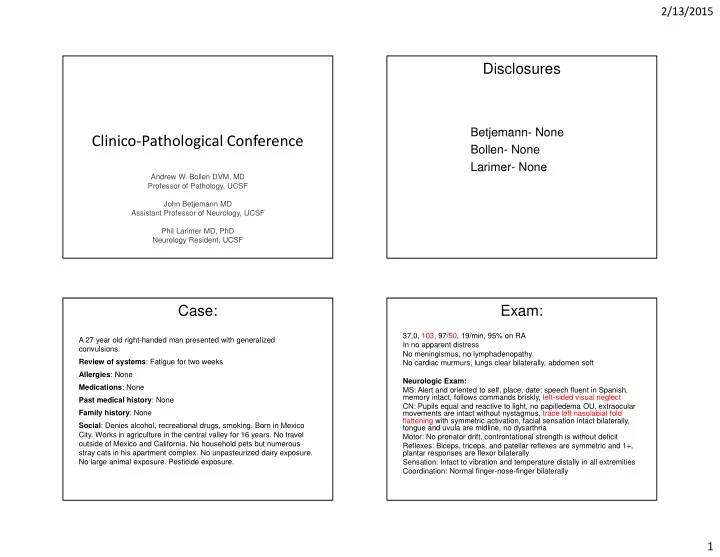
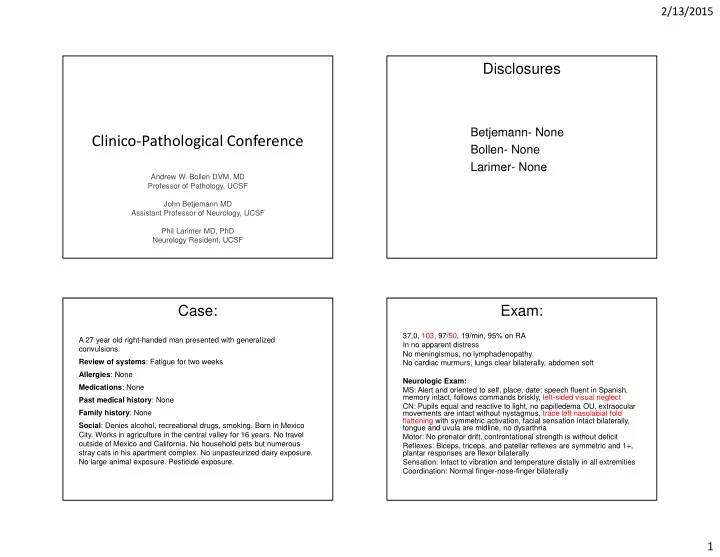
2/13/2015 Disclosures Betjemann- None Clinico-Pathological Conference Bollen- None Larimer- None Andrew W. Bollen DVM, MD Professor of Pathology, UCSF John Betjemann MD Assistant Professor of Neurology, UCSF Phil Larimer MD, PhD Neurology Resident, UCSF Case: Exam: 37.0, 103, 97/50, 19/min, 95% on RA A 27 year old right-handed man presented with generalized In no apparent distress convulsions. No meningismus, no lymphadenopathy Review of systems : Fatigue for two weeks No cardiac murmurs, lungs clear bilaterally, abdomen soft Allergies : None Neurologic Exam: Medications : None MS: Alert and oriented to self, place, date; speech fluent in Spanish, Past medical history : None memory intact, follows commands briskly, left-sided visual neglect CN: Pupils equal and reactive to light, no papilledema OU, extraocular Family history : None movements are intact without nystagmus, trace left nasolabial fold flattening with symmetric activation, facial sensation intact bilaterally, Social : Denies alcohol, recreational drugs, smoking. Born in Mexico tongue and uvula are midline, no dysarthria City. Works in agriculture in the central valley for 16 years. No travel Motor: No pronator drift, confrontational strength is without deficit outside of Mexico and California. No household pets but numerous Reflexes: Biceps, triceps, and patellar reflexes are symmetric and 1+, stray cats in his apartment complex. No unpasteurized dairy exposure. plantar responses are flexor bilaterally No large animal exposure. Pesticide exposure. Sensation: Intact to vibration and temperature distally in all extremities Coordination: Normal finger-nose-finger bilaterally 1
2/13/2015 Initial Labs 12.7 14.8 247 36.9 CRP 5.2 CT head 5 cm FLAIR 5 cm T1 with gadolinium 5 cm 2
2/13/2015 ADC 5 cm GRE 5 cm Therapies: Labs (normal unless otherwise noted): Dexamethasone CRP 5.2 RPR Albendazole CEA Serum cryptococcal antigen AFP Serum cocci immunodiffusion and Vancomycin, Ceftriaxone CA 19-9 complement fixation Metronidazole CA 125 HIV antibody and viral load Beta HCG CD4 228 Cefipime EBV PCR TTE: Normal Cefazolin Cysticercosis IgG Computed tomography scans of Toxoplasmosis IgG, IgM, PCR Imipenem/cilastin the chest, abdomen, and pelvis CSF (HD#4): 5 WBC (98% TMP-SMX as well as an ultrasound of the lymphocytes), 0 RBC, glc 83, testicles did not reveal a primary Vancomycin protein 30, LDH 14, CrAg, cocci neoplasm. complement fixation, india ink, Voriconazole CTA head/neck: normal AFB smear, cysticercosis IgG Ambisome Blood/CSF bacterial/AFB/fungal cultures: no growth 1 7 14 21 26 Hospital Day (transfer) 3
2/13/2015 Clinical Course Scan at day 26 Brain Seizure LP Biopsy Fever Mild encephalopathy and ongoing headaches Vancomycin, Ceftriaxone Cefazolin Cefipime Metronidazole TMP-SMX Albendazole Voriconazole/Vancomycin Dexamethasone Opiates for headache FLAIR T1 with GAD 1 7 14 21 26 Hospital Day (transfer) FLAIR T1 with GAD FLAIR T1 with GAD 4
2/13/2015 FLAIR T1 with GAD FLAIR T1 with GAD FLAIR T1 with GAD FLAIR T1 with GAD 5
2/13/2015 FLAIR T1 with GAD FLAIR T1 with GAD FLAIR T1 with GAD FLAIR T1 with GAD 6
2/13/2015 FLAIR T1 with GAD FLAIR T1 with GAD UCSF Course • He remained in coma with EEG demonstrating only diffuse slowing. • Due to evidence of herniation on arrival, he was intubated and an EVD was placed. • He had elevated intracranial pressure refractory to CSF diversion and medical management so had a decompressive hemicraniectomy on UCSF HD#3. • He did not regain brainstem reflexes, was Death transitioned to comfort measures, and succumbed to his illness 35 days after initial Decompression presentation EVD Brain Biopsy Seizure Fever Intubated (inconclusive) Mild encephalopathy Coma FLAIR T1 with GAD 1 7 14 21 28 35 Hospital Day 7
2/13/2015 Approach and Overview � Key points � History � Exam � Evaluation � Treatment RECENT ADVANCES IN � Broad Differential Diagnosis (DDx) NEUROLOGY � Further work up CLINICO-PATHOLOGIC � Diagnostic and treatment pearls CONFERENCE � Make a diagnosis John Betjemann, MD History and Exam- Key Points Evaluation and Treatment- Key Points � Young healthy man from Mexico working in � Labs agriculture � LP: not consistent with meningitis but was performed after 4 days of steroids and Abx � Subacute onset of fatigue, encephalopathy, � CD4= 228 headache and new seizure � Imaging: � Exposure to stray cats � Initially multiple ring enhancing lesions with edema. � Exam: left visual neglect, facial asymmetry New lesions on repeat scan despite treatment � Treatment � Steroids � Polymicrobial, fungal, neurocysticercosis (NCC) 8
2/13/2015 Differential Diagnosis Low CD4 � Malignancy � Infection � Lymphoma � Pyogenic abscess � Multifocal CNS � Septic emboli neoplasm/metastases � Toxoplasmosis � Gliomatosis Cerebri � Fungi � Sarcoid � TB � Infarct/vasculitis � NCC Walker UA. Curr Opin Rheumatol 2006 Malignancy- Multifocal glioma/CNS Malignancy- CNS Lymphoma metastases � Pros � Pros � Encephalopathy, focal � Headache, seizures deficits, and seizures � Imaging: ring enhancing masses, gray-white, with edema � Immunodeficiency � Cons � Cons � Encephalopathy � Age � Age � Usually more steroid � Lack of discernible primary responsive � Dramatic progression after 3 weeks � Imaging Haldorsen IS. AJNR 2011 9
2/13/2015 Malignancy- Gliomatosis Cerebri Infection- Pyogenic Abscess � Pros � Cons � Age � History and exam � Ring enhancing lesions � Usually more extensive radiographic involvement � Cons (none of these exclude the possibility!) � Lack of fever � Negative blood cultures � CSF classically with pleocytosis and elevated protein � Septic emboli � Negative TTE and blood Cx, lack of other embolic strokes and absence of hemosiderin on GRE Freund M. et al. Eur Radiol. 2001 Infection- Toxoplasmosis Infection- Fungi � Cryptococcus � Pros � Usually immunocompromised � Immunodeficiency � Typically meningoencephalitis rather than discrete mass- � Imaging: multiple ring enhancing like lesions (cryptococcomas) lesions with edema � CSF: � Cons � elevated OP, pleocytosis (lymphocytic), low gluc, high prot. � India ink, culture and CrAg (sens 93-100 and spec 93-98)(Tanner � Not quite immunodeficient enough DC et al. 1994) � Negative serologies � Aspergillosis � Majority are IgG positive � Usually disseminated infection but can be local spread � PCR: 83% sens, 95% spec in CSF of AIDS-infected patients � Coccidomycosis (similar in serum) (Alfonso Y, et al. 2009 and Mesquita RT et � Typically a meningitis, but can have abscess formation al. 2010) � CSF with lymphocytic pleocytosis 10
2/13/2015 Infection- TB Infection- Neurocysticercosis � Pros � Pros � Imaging fits well with tuberculomas � Commonly presents with seizures and focal findings � Low CD4 may serve as risk for TB or may be result of active � From an endemic area TB � Cons � CSF often nonspecific in tuberculomas � Not treated empirically for TB � Imaging not classic-not truly cystic, no calcification, � Negative AFB smear and culture are not terribly helpful and no scolex � Cons � Serum Ab testing negative (up to 98% sensitive) (Del � Classically causes a meningitis +/- tuberculomas Brutto OH 2012) � Not from a truly endemic area � New lesions despite albendazole � CT chest without malignancy, but evidence of remote TB? Neurosarcoid Vasculitis � Can impact any portion of the CNS without � Many of the above conditions can be associated systemic manifestations with a vasculitis � Imaging: can see enhancing parenchymal lesions � Might somewhat explain the interval progression but also often meningeal enhancement and cranial on MRIs neuropathies � Initial treatment involves steroids 11
2/13/2015 Further Diagnostic Considerations Diagnostic and Treatment Pearls � CSF � Dental exam: source of bacteremia and septic � Timing: emboli � when possible LP prior to steroids and Abx � Ophthalmologic exam: sarcoid, lymphoma � For cytology, CSF should be analyzed within few hours � PET scan: potential biopsy target � For TB and lymphoma key is volume, volume, volume! � Labs: Beta-D-glucan, galactomannan � Lymphoma: cytology sensitivity 2-32% (Scott BJ, 2013). Lower yield with small CF volume, processing delays and steroids � TB: AFB smear~60%, PCR 56% sensitivity (Thwaites GE 2013) � Steroids � Alter imaging, decrease diagnostic yield (lymphoma) Diagnostic and Treatment Pearls Diagnosis � Our CSF diagnostic testing is limited! � What are we good at Lymphoma � Viruses Pyogenic abscess � CrAg Tuberculosis � In many cases a negative test doesn’t exclude the Neurocysticercosis Fungal abscess disease (lymphoma, TB) Neurosarcoid gliomatosis Toxoplasmosis Metastatic/multifo +/- vasculitis cal glioma Steiner I, et al. Eur J Neuol. 2012 12
Recommend
More recommend