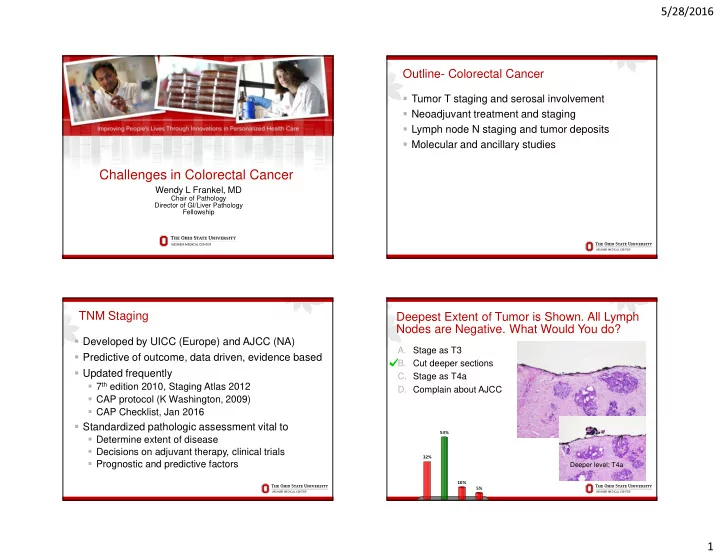
5/28/2016 Outline- Colorectal Cancer � Tumor T staging and serosal involvement � Neoadjuvant treatment and staging � Lymph node N staging and tumor deposits � Molecular and ancillary studies Challenges in Colorectal Cancer Wendy L Frankel, MD Chair of Pathology Director of GI/Liver Pathology Fellowship TNM Staging Deepest Extent of Tumor is Shown. All Lymph Nodes are Negative. What Would You do? � Developed by UICC (Europe) and AJCC (NA) A. Stage as T3 � Predictive of outcome, data driven, evidence based B. Cut deeper sections � Updated frequently C. Stage as T4a � 7 th edition 2010, Staging Atlas 2012 D. Complain about AJCC � CAP protocol (K Washington, 2009) � CAP Checklist, Jan 2016 � Standardized pathologic assessment vital to 53% � Determine extent of disease � Decisions on adjuvant therapy, clinical trials 32% � Prognostic and predictive factors Deeper level; T4a 10% 5% 1
5/28/2016 T4- Serosal Involvement CAP Cancer Staging Protocol- T4 � Absence of standard guidelines for assessing � Associated with decreased survival peritoneal involvement may contribute to � May need additional treatment underdiagnosis � Adjuvant chemotherapy recommended by ASCO for � The following findings are considered to Stage III and IV not II unless high risk features (i.e. T4) represent serosal involvement by tumor � Significant variability in reporting serosal involvement � Tumor at serosal surface with inflammatory � Studies with meticulous sampling 59% reaction, mesothelial hyperplasia, and/or � Other studies <10% erosion/ulceration � Underdiagnosed likely due to inadequate sampling � Free tumor cells on serosal surface with and not recognizing serosal penetration (up to 20%) underlying ulceration of visceral peritoneum � Both associated with decreased survival Gunderson LL, J Clin Oncol, 2010; Ludeman L, Histopathol, 2005; Shepherd NA, Gastroenterol, 1997 T4a- Serosal Surface Deeper Sections T3- close Deeper Sections, T4a 2
5/28/2016 Serosal Clefts- T4a Cytokeratin 7 is not helpful in most cases Tumor less than 1 mm; Serosal Reaction Cleft- Mesothelial Hyperplasia T3 vs. T4a � Serosal penetration under-recognized � Serosal scrape cytology 128 cases colon cancer � Peritoneal cytology + in 19% T3 (46% in T3 within 1 mm of serosal reaction) and 55% T4 Cancer � Tumor < 1 mm with reaction; T4a? � Fibroinflammatory, granulation tissue � Peritumoral abscess that communicates to surface Mesothelium � Hemorrhage, fibrin � Reactive mesothelial cells Panarelli, Am J Surg Pathol, 2013 3
5/28/2016 Elastic Stain- Why Consider it? Serosal Surface T3 or T4a? � T3 vs. T4a can be challenging � Clinically important Stage II � Possible surrogate for serosal invasion � Elastic in lung cancer for invasion visceral pleura, AJCC 7 th ed TNM � Subserosal elastic lamina colon � Located just deep to peritoneum � May be retracted toward front of carcinoma because of fibrosis � Not present in all cases If gross perforation, T4 Elastic Stain Elastic Stain- Helpful or Not? � Studies variable results; different stains and # slides � Challenges � Not all cases contain EL, particularly right colon � EL incomplete in many; need to ‘draw a line’ � Not practical if necessary to stain several slides � Reporting results (if you find EL+ deep T3) � Upstage or add comment? � I currently do not use it Deep T3 Elastic Lamina Invasion Shinto, Dis Col Rect, 2004; Kojima, Am J Surg Pathol, 2010; Kojima, Front Oncol, 2012; Liang, Am J Surg Pathol, 2013; Grin, Hum Pathol, 2013; Kojima, Am J Surg Pathol, 2013 4
5/28/2016 Deepest Extent of Tumor and Elastic Stain are Rectal Resections Shown. What Would You do? A. Stage as T3 � Radial margin most critical factor local B. Stage as T4a recurrence in rectal C. Cut deeper sections cancer (< 1mm) D. Complain about both AJCC � No 4a in non- and Elastic stains serosalized rectum 50% 47% Deeper level; T4a 2% 1% A. B. C. D. Tumor Regression Grade Neoadjuvant Chemoradiation � For advanced rectal cancer; T3-T4 and/or LN+ Description Tumor Regression Score � Improved resectability/reduced local recurrence No viable cancer cells 0 (complete response) � Associated with significant tumor response, Single cells or small groups of cells 1 (near complete response) downstaging, better prognosis � Several grading systems, modified Ryan Residual cancer with evident tumor 2 (partial response) suggested regression, but more than single cells or small groups of cells � Evaluate in tumor � Not LN or other metastatic site Extensive residual cancer with no 3 (poor or no response) evident regression � Acellular mucin likely represent treated cancer � Do not use to classify T or N 5
5/28/2016 Tumor Regression Grade Mucin Pools Tumor cells 0 (Complete Response) 2 (Partial Response) Acellular 1 (Near Complete Response) 3 (Poor Response) Mucin Pools Deeper than Malignant Cells All Other 14 Lymph Nodes are not Involved, What is the N Stage? Still ypT2 A. N0 B. N1 C. N1a D. N1 with comment Mucin in perirectal fat Still ypT2, Radial Margin- R0 57% ypT2 16% 14% 13% Mucin at radial margin Don’t upstage T or call + radial margin A. B. C. D. 6
5/28/2016 Muddy the Waters Tumor Deposits What Counts as a Lymph Node? � Nodules without residual nodal tissue (recognized 1935) � AJCC 5 th edition (1997) � Size matters, 3mm � AJCC 6 th edition (2002) � Shape matters (contour) � Round smooth � Irregular � AJCC 7 th edition (2010) � Count all separately � LN, LVI or discontinuous tumor � N1c Tumor Deposits Classify this Metastasis: What Counts as a Lymph Node? A. Involved lymph node B. Tumor deposit C. Lymphovascular invasion D. Indirect spread of tumor 63% 29% There are identifiable LN < Poor reproducibility Still subjective, residual LN 3mm; data not confirmed 6% 3% A. B. C. D. 7
5/28/2016 Lymph Node (pN) Issues in Staging- Tumor Deposit and N1c Tumor Deposit � TD can be diagnosed when � Discrete foci tumor in � No residual LN is found pericolic/perirectal fat or in adjacent mesentery away from � Do not add TD to positive LN number leading edge of tumor and no � Do not use N1c if any positive LN evidence residual LN but within lymph drainage area of primary � Do not use N1c if N1(mic)- 0.2 to 2 mm carcinoma � N1c is not worse, by definition, than N1a or b � TD- Discontinuous spread, LV with extravascular extension, or � N1c appears to be at least as bad as N1 totally replaced LN � Does not change the T stage even if tumor is T1/T2, � Identifiable LVI/LN is not TD and TD is in pericolonic tissue Jin, Am J Surg Pathol, 2015 Interobserver Study LN vs. TD: 25 Tumor Deposit (7/7) Metastasis Reviewed by 7 Pathologists Lymph Node (7/7) Rock, Arch Path Lab Med, 2013 8
5/28/2016 Challenging- TD or LN? Classify this Metastasis: Tumor Deposit (4/7) Lymph Node (4/7) A. Involved lymph node B. Tumor deposit C. Lymphovascular invasion D. Indirect spread of tumor 70% No definite residual LN or vessel Moderate agreement Useful features: round, peripheral lymphocytes/follicles, thick capsule, 14% 11% possible subcapsular sinus 5% A. B. C. D. Classify this Metastasis; If there is Already 1 Lymph Nodes Positive LN, What N Stage? � Minimum number? The more the better � Fat clearing helps, not standard practice A. Involved lymph node, N1a B. Tumor deposit, N1a � AJCC TNM 7, at least 10-14; CAP, <12, regross C. Involved lymph node, N1c � No definite minimum rectum after neoadjuvant D. Tumor deposit, N1c � Many factors affect recovery � Pathologist/surgeon experience and diligence � Patient age, sex, obesity, immune response � Length colon, procedure, site, size 48% � Future- lymph node ratio? No definite residual LN so TD; Do not 32% use N1c since another positive LN; Do not add to LN count (so not N1b) Goldstein N, Am J Surg Pathol, 2002; Cserni G, J Surg Oncol, 2002; Le Voyer TE, J Clin Oncol 11% 9% 2003; Chang GJ, JNCI, 2007; Dillman RO, Cancer, 2009; Govindarajan, J Clin Onc, 2011; de Campos-Lobato, Ann Surg Oncol, 2013 A. B. C. D. 9
5/28/2016 Tumor Budding Tumor Budding � Currently not recommended AJCC or CAP checklist � Groups of up to 5 cells at the invasive front of tumor � Associated with aggressive behavior � Most evidence where it may affect therapy � Polypectomy (?resection), Stage II CRC (?adjuvant) � Variability in criteria, high and low grade, cytokeratin, intratumoral budding (ITB) � Many studies published and ongoing Jass, JCP, 2003; Lugli, Br J Can, 2010; Lugli Hum Pathol, 2011; Bosch, Endosc, 2013; Horcic, Hum Pathol, 2013; Rogers, Mod Path, 2014 38 AJCC TNM 8; Will it be Clearer? Molecular Tests and Biomarkers � +Not required; may be clinically important � Histologic features suggestive of microsatellite instability (MSI) and Lynch � CAP biomarker template- December 2014 � MSI status � Immunohistochemistry for MMR proteins � BRAF V600E analysis � KRAS mutational analysis � MLH1 promoter methylation, NRAS , PIK3CA , PTEN 10
Recommend
More recommend