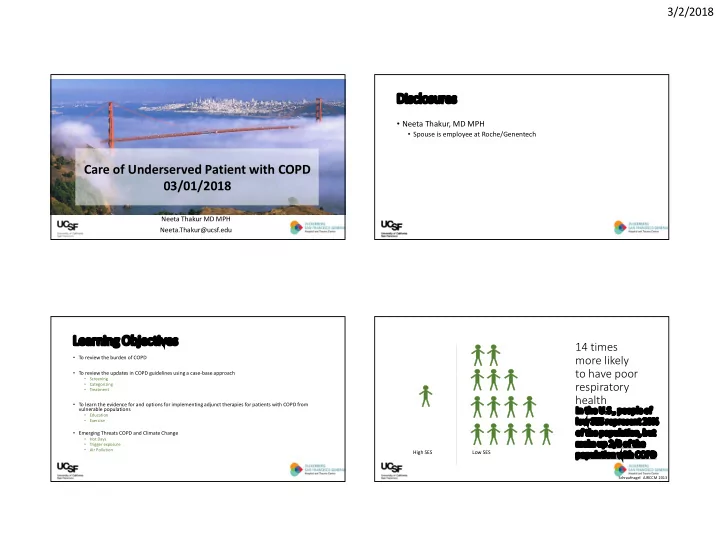
3/2/2018 Disclosures • Neeta Thakur, MD MPH • Spouse is employee at Roche/Genentech Care of Underserved Patient with COPD 03/01/2018 Neeta Thakur MD MPH Neeta.Thakur@ucsf.edu Learning Objectives 14 times • To review the burden of COPD more likely to have poor • To review the updates in COPD guidelines using a case-base approach • Screening • respiratory Categorizing • Treatment health • To learn the evidence for and options for implementing adjunct therapies for patients with COPD from vulnerable populations In the U.S., people of • Education • low SES represent 20% Exercise of the population, but • Emerging Threats COPD and Climate Change • Hot Days make up 2/3 of the • Trigger exposure • Air Pollution High SES Low SES population with COPD Schraufnagel AJRCCM 2013 1
3/2/2018 Risk Factors for COPD Exposures over the life course lead to Environmental Host Factors COPD in adulthood • TOBACCO TOBACCO • Alpha-1 antitrypsin TOBBACO and worsen disease deficiency (young age, • Cigarette, pipe, cigar, secondhand smoking hx not congruent tobacco exposure with symptoms, degree of • Biomass fuel cooking obstruction) • SES • HIV – accelerated decline • Occupational dusts and • Long-standing asthma fumes • Previous hx of TB Methods for addressing Disparity Case 1 • A 58 yo M presents with 9 months progressive SOB and fatigue • Improve Case Detection • Reports cough productive of thick white sputum every morning • Improve access to evidence-based care and management • Increase smoking cessation efforts, decrease exposure to Tobacco Hx bio-mass fuel and occupational exposure • 30 pack-yr, • Current ¼ ppd smoker ROS • Denies chest pain, weight loss, F/C/NS High SES Low SES 2
3/2/2018 When to Consider COPD When to Consider COPD Patients >40 years + 20 pack-year history of smoking, visiting a NO Does everyone need to be screened? primary care physician for any reason (n=1003) When should we screen? Screening for COPD • Age > 40 yo Patients meeting • SYMPTOMATIC: Dyspnea worse with exercise, chronic Dx of COPD, No evidence of Overall Prevalence criteria for COPD cough, chronic sputum production obstruction (n=43; 5.6%) (n=208; 20.7%) • CASE FINDING: History of exposure to known risk factors Previous diagnosis of No previous diagnosis of COPD (n=67; 32.7%) COPD (n=141; 67.3%) goldcopd.org2017, Hill CMAJ 2010 goldcopd.org2017, Hill CMAJ 2010, Martinez JAMA 2016 Classification of severity of airflow Next diagnostic steps could include limitation in COPD Based on post-bronchodilator FEV1 • CXR – for alternative diagnoses In patients with FEV1/FVC < 0.70 • Chest CT – another method for alternative diagnoses GOLD 1: Mild FEV 1 ≥ 80% • Full PFTs – not essential for management but can further characterize severity GOLD 2: Moderate 50% ≤ FEV1 < 80% • Spirometry with bronchodilator reversibility testing – essential for management GOLD 3: Severe 30% ≤ FEV1 < 50% Post-bronchodilator FEV1/FVC < 0.70 GOLD 4: Very severe FEV1 < 30% confirms presence of persistent airflow limitation goldcopd.org, 2017 goldcopd.org, 2017 3
3/2/2018 Case 1, revisited • A 55 yo M presents with 9 months progressive SOB • Also c/o cough productive of thick white sputum QAM • 30 pk yr smoking history, current ¼ ppd smoker • Denies chest pain, weight loss, F/C/NS But what if he does not meet spirometric criteria for COPD? What should we make of his symptoms? Medication use COPD Assessment Test (CAT) Symptomatic ever-smokers with preserved spirometry Symptoms (CAT≥10) are • 42% used bronchodilators common in smokers with • 23% used inhaled glucocorticoids preserved pulmonary function …They are currently using a range of respiratory medications without any evidence base. 50 vs 65% Target Smoking NON- Current/ Current/ Cessation smokers Former Former Smokers Smokers NO COPD Mild/Mod COPD Woodruff NEJM 2016 Woodruff NEJM 2016 4
3/2/2018 Combined COPD assessment Case 2 Spirometric Grade Symptoms & Future risk • 64 yo W 40 pk-yr smoker with COPD, quit 2 yrs ago • Modified British Medical • Airflow limitation using • c/o cough, chest tightness, fatigue, and DOE Research Council GOLD classification • Exercise tolerance of 2 blocks (mMRC) Dyspnea Scale (post-FEV 1 ) • ED visits x 2 in the past 6 months for COPD flares • COPD Assessment Test • Population-level • HTN, hyperlipidemia, CAD (CAT) outcomes • CXR w/large lung volumes and flattened diaphragms • Exacerbations in the • Useful for prognosis • Post-bronchodilator FEV1 0.81 (27%) previous 12 months • ratio 0.29 • Guide treatment Goldcopd.org2017 Classification of severity of airflow mMRC Dyspnea Scale limitation in COPD Based on post-bronchodilator FEV1 Grade Intensity or amount of activity that provokes SOB In patients with FEV1/FVC < 0.70 0 Strenuous physical activity GOLD 1: Mild FEV 1 ≥ 80% 1 Hurrying on the level or walking up slight incline GOLD 2: Moderate 50% ≤ FEV1 < 80% 2 Walking at own pace on the level GOLD 3: Severe 30% ≤ FEV1 < 50% 3 Walking a few minutes on the level 4 Unable to leave the house or getting GOLD 4: Very severe FEV1 < 30% dressed/undressed goldcopd.org, 2014 Goldcopd.org 2017 Stenton C Occup Med (Lond) 2008;58:226-227 5
3/2/2018 Symptoms: COPD Assessment Test Assess Risk for Exacerbations Never 0 1 2 3 4 5 Cough always • Past events treated with oral steroids predicts future No phlegm (mucus) Full of phlegm (mucus) 0 1 2 3 4 5 risk No chest tightness Very tight chest 0 1 2 3 4 5 Very SOB up a hill or 1 flight of No SOB up a hill or 1 flight of stairs 0 1 2 3 4 5 stairs • HIGH risk based on frequency and severity Not limited doing any activities at Very limited doing activities at 0 1 2 3 4 5 home home ≥ 2 per year 0 1 2 3 4 5 Confident leaving home Not confident leaving home ≥ 1 hospitalization 0 1 2 3 4 5 Sleep soundly Do not sleep soundly 0 1 2 3 4 5 Lots of energy No energy at all Modified from 2009 GlaxoSmithKline Goldcopd.org 2017 GOLD: “Combined assessment” Hosp ≥ 1/yr Hosp ≥ 1/yr Exac ≥ 2/yr Exac ≥ 2/yr mMRC ≥2 mMRC 0-1 Future risk CAT ≥10 CAT <10 (exacerbations) Exac/yr ≤ 1 Exac/yr ≤ 1 No hosp No hosp mMRC 0-1 mMRC ≥2 CAT <10 CAT ≥10 Symptoms (mMRC, CAT) Korpershoek International Journal of COPD 2017 Goldcopd.org 2017 6
3/2/2018 GOLD: “Combined assessment” Case 2 • 64 yo W 40 pk-yr smoker with COPD, quit 2 yrs ago Hosp ≥ 1/yr Hosp ≥ 1/yr • c/o cough, chest tightness, fatigue, and DOE (CAT > 10) Exac ≥ 2/yr Exac ≥ 2/yr 6 Minute • Exercise tolerance of 2 blocks (mMRC ≥ 2) Walk mMRC ≥2 mMRC 0-1 • ED visits x 2 in the past 6 months for COPD flares (≥ 2) Future risk CAT ≥10 CAT <10 • HTN, hyperlipidemia, CAD (exacerbations) • CXR w/large lung volumes and flattened diaphragms Exac/yr ≤ 1 Exac/yr ≤ 1 No hosp No hosp Adherence • Post-bronchodilator FEV1 0.81 (27%) (< 30%) / • ratio 0.29 mMRC 0-1 Technique mMRC ≥2 CAT <10 CAT ≥10 Symptoms (mMRC, CAT) Goldcopd.org 2017 Management of Stable COPD GOLD: “Combined assessment” ICS + LABA and/or LAAC ICS + LABA or Hosp ≥ 1/yr LAAC Hosp ≥ 1/yr LAAC or Exac ≥ 2/yr Grade 4 Alternate choices: Exac ≥ 2/yr Alternate choices: LABA LAAC & LABA Albuterol PRN or LAAC & LABA or Class D or LAAC & PDE-4 inhibitor Ipratropium PRN mMRC ≥2 mMRC 0-1 LAAC & PDE-4 inhibitor or Alternate choice: Alternate choice: Future risk or ICS + LABA & PDE-4 inhibitor CAT ≥10 LAAC & LABA CAT <10 Combivent PRN LABA & PDE-4 inhibitor (exacerbations) Patient Group A, B, C, D : Tobacco cessa�on, ↓ of risk factors, physical ac�vity, Flu & Exac/yr ≤ 1 Exac/yr ≤ 1 Pneumococcal vaccines No hosp Patient Groups B, C, D : Referral to pulmonary rehabilitation, Better Breather Courses No hosp Patient Groups C, D : Home oxygen if SpO2 ≤ 88%RA A B D C mMRC 0-1 mMRC ≥2 ↓ sx/Low risk ↑ sx/Low risk CAT <10 CAT ≥10 ↓ sx/High risk ↑ sx/High risk Symptoms (mMRC, CAT) Goldcopd.org 2017 goldcopd.org, 2017 7
3/2/2018 National Lung Screening Trial Case 2 64 yo woman 40 pack-year smoker Quit 2 years ago Do you screen for lung cancer? 53,454 randomized to annual CXR vs. CT scans N Engl J Med. 2011; 365: 395-409. National Lung Screening Trial (NLST) Exclusions Inclusion: • Prior diagnosis of lung cancer • Age 55 - 74 years • Chest CT within 18 months • Hemoptysis • History of cigarette • Unexplained weight loss smoking > 30 pack yrs USPSTF • If former smokers, • STOP once a person has not smoked quit within 15 years for 15 years • Health problem (functional status) that substantially limits life expectancy or the ability or willingness to have curative lung surgery Overall 39% with positive results 96% were FALSE positive N Engl J Med. 2011; 365: 395-409. N Engl J Med. 2011; 365: 395-409. 8
Recommend
More recommend