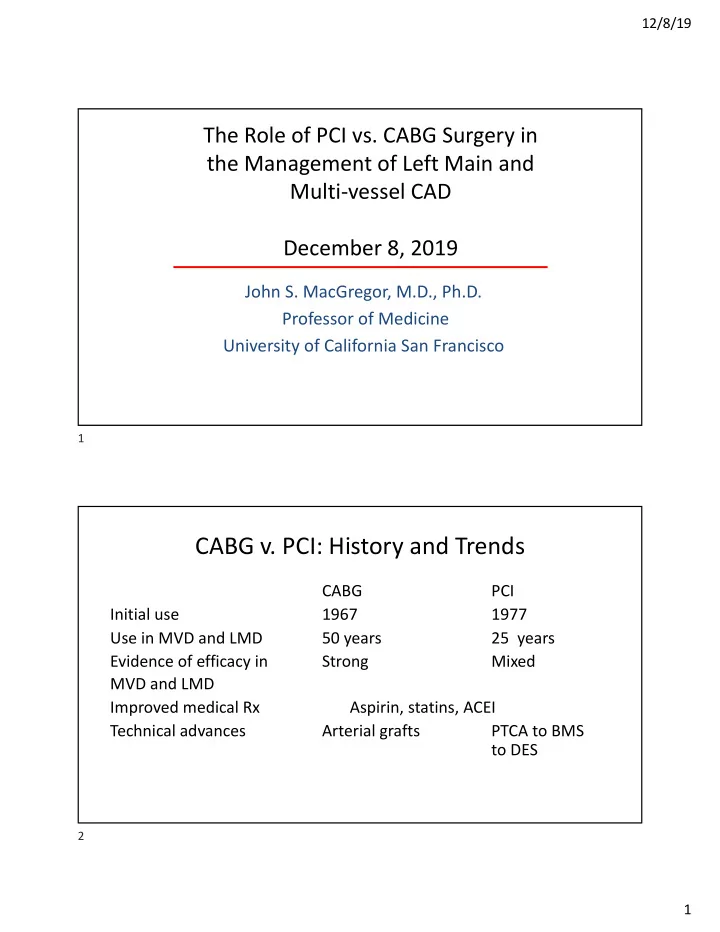
12/8/19 The Role of PCI vs. CABG Surgery in the Management of Left Main and Multi-vessel CAD December 8, 2019 John S. MacGregor, M.D., Ph.D. Professor of Medicine University of California San Francisco 1 CABG v. PCI: History and Trends CABG PCI Initial use 1967 1977 Use in MVD and LMD 50 years 25 years Evidence of efficacy in Strong Mixed MVD and LMD Improved medical Rx Aspirin, statins, ACEI Technical advances Arterial grafts PTCA to BMS to DES 2 1
12/8/19 Limitations of Studies Comparing CABG and PCI • Highly selected patients • Less severe CAD • Limited duration of follow-up • Surgical patients often receive inferior medical therapy • Crossover 3 Prospective, Randomized, Controlled Trials Comparing CABG to PCI Doenst et al. J Am Coll Cardiol. (2019) 73(8):964-976. 4 2
12/8/19 Mechanistic Differences Between PCI v. CABG Doenst et al. J Am Coll Cardiol. (2019) 73:964-976. 5 SYNTAX Score A measure of the severity and complexity of coronary disease. Coronary arteries divided into over 25 segments and the assessment includes: location and severity of stenosis, CTO, calcification, presence of thrombus, lesion length, tortuosity of artery, caliber of artery, bifurcation or trifurcation, aorto-ostial lesion. Higher scores indicate more severe and complex coronary disease. 6 3
12/8/19 SYNTAX Study 4337 patients with 3VD or LM disease were screened. 1800 randomized to either CABG (897) or PCI (903). Recruitment from March 2005 through April 2007. 1287 patients (29.4%) excluded based on heart team review. Primary end point: MACCE at one year (death, CVA, MI, revasc.). Non-inferiority (pre-specified delta value 6.6%). Result: Taxus stent failed to meet non-inferiority v. CABG. Medical Rx in CABG group was significantly inferior to PCI group. Serruys et al., NEJM (2009) 360: 961-72. 7 SYNTAX Trial: 5 Year MACCE for Patients with 3-VD According to SYNTAX Score Doenst et al. J Am Coll Cardiol. (2019) 73(8):964-976. 8 4
12/8/19 SYNTAX Trial: Probability of Death up to 10 Years Thuijs et al. Lancet, (2019) 394:1325-1334. 9 SYNTAX Trial: Probability of death at maximum follow up Thuijs et al. Lancet, (2019) 394:1325-1334. 10 5
12/8/19 SYNTAX Trial: Probability of Death up to 10 Years In Patients with 3-Vessel (A) and LM (B) Disease Thuijs et al. Lancet, (2019) 394:1325-1334. 11 SYNTAX Trial: Probability of Death up to 10 Years In Patients With (C) and Without (D) Diabetes Thuijs et al. Lancet, (2019) 394:1325-1334. 12 6
12/8/19 SYNTAX Trial: Probability of Death up to 10 Years, SYNTAX Score 22 or Less Thuijs et al. Lancet, (2019) 394:1325-1334. 13 SYNTAX Trial: Probability of Death up to 10 Years, SYNTAX Score 23 through 32 Thuijs et al. Lancet, (2019) 394:1325-1334. 14 7
12/8/19 SYNTAX Trial: Probability of Death up to 10 Years, SYNTAX Score 33 or Greater Thuijs et al. Lancet, (2019) 394:1325-1334. 15 SYNTAX Trial: Subgroup Analysis of 10 Year Mortality Thuijs et al. Lancet, (2019) 394:1325-1334. 16 8
12/8/19 FREEDOM Trial: Probability of Survival, CABG v. PCI Farkouh et al. J Am Coll Cardiol. (2019) 73(6):629-638. 17 NOBLE Trial (LM Disease): MACCE at 5 Years Mäkikallio et al. Lancet. (2016) 388:2743-2752. 18 9
12/8/19 NOBLE Trial (LM Disease): Individual Components of MACCE at 5 Years Mäkikallio et al. Lancet. (2016) 388:2743-2752. 19 EXCEL Trial: PCI v. CABG in left main disease Primary end-point: Death stroke, MI at 3 years Secondary end-point: Primary plus repeat revascularization Non-inferiority trial (non-inferiority margin 4.2%) Result: PCI CABG Primary end-point 15.4% 14.7% Secondary end-point 23.1 19.1 (4% difference) Study concluded – Non-inferior. Stone et al., NEJM (2016), 375:2223-35. 20 10
12/8/19 SYNTAX Trial: Probability of death at 10 years Thuijs et al. Lancet, (2019) 394:1325-1334 21 NYS Cardiac Registry Between 1/1/1997 and 12/31/2000 37,212 patients with MVD had CABG 22,102 patients with MVD had PCI Compared with PCI patients, CABG patients were older, had lower EF, more CVD, diabetes, renal failure, 3 VD, CHF, COPD. Hannan et al., NEJM, 2005 22 11
12/8/19 NYS cardiac registry: Kaplan-Meier curves adjusted for comorbidity (Hannan et al., NEJM, 2005) Three-Vessel HannanmDisease with Disease of the Proximal LAD Artery nn an et al. NE J M 20 05 . 23 Survival for DES v. CABG: New York State Clinical Registries for PCI and CABG Surgery Hannan et al. Ann Thorac Surg. (2015) 100(6):2227-36. 24 12
12/8/19 Survival for DES v. CABG: New York State Clinical Registries for PCI and CABG Surgery Hannan et al. Ann Thorac Surg. 2015 Dec;100(6):2227-36. 25 MASS II: Probability of Event-Free Survival at 10 Years With Medical Rx. v. PCI v. CABG Surgery Hueb et al. Circulation. (2010)122(10):949-57. 26 13
12/8/19 MASS II: Hazard ratios for MACE CABG v. MT Hueb et al. Circulation. (2010) 122(10):949-57. 27 MASS II: Hazard ratios for MACE CABG v. PCI Hueb et al. Circulation. (2010) 122(10):949-57. 28 14
12/8/19 MASS II: Hazard ratios for MACE MT v. CABG Hueb et al. Circulation. (2010) 122(10):949-57. 29 ACC/AHA PRACTICE GUIDELINE Revascularization in Stable CAD Patients For Symptom Relief: Class I, Level of Evidence A CABG or PCI to improve symptoms is beneficial in patients with 1 or more significant (70% or more diameter) coronary artery stenosis amenable to revascularization and unacceptable angina despite GDMT (JACC 60: (2012) 2564- 2603). 30 15
12/8/19 ACC/AHA PRACTICE GUIDELINE Revascularization in Stable CAD Patients For Improved survival.: Class I, Level of Evidence B CABG to improve survival is recommended for patients with significant (50% or more diameter stenosis) left main coronary artery stenosis. CABG to improve survival is beneficial in patients with significant (70% or more diameter) stenosis in 3 major coronary arteries, or the proximal LAD plus one other major artery. (JACC 60: (2012) 2564- 2603). 31 ACC/AHA Practice Guidelines “No study to date has demonstrated that PCI in patients with SIHD improves survival rates.” (JACC 58:e44-122 (2011)). Class IIa – PCI to improve survival is reasonable as an alternative to CABG in LM CAD with low (22 or less) SYNTAX score. Class IIb – PCI may be reasonable to improve survival as an alternative to CABG in LM CAD with low to intermediate (less than 33) SYNTAX score. Class IIb – The usefulness of PCI to improve survival is uncertain in patients with 2 or 3-vessel CAD (with or without proximal LAD involvement) or 1-vessel proximal LAD disease. 32 16
12/8/19 Conclusion: Factors Favoring CABG Clinical characteristics: Diabetes, Reduced LV function (EF <35%), Contraindication to DAPT, Recurrent diffuse in- stent restenosis, patient preference. Anatomical and MVD with SYNTAX score greater than 22, Anatomy technical factors: likely to result in incomplete revascularization with PCI (CTOs), Severely calcified lesions. Need for Ascending aorta pathology with indication for concomitant surgery: surgery, indication for valve surgery or other cardiac surgery. 33 Conclusion: Factors Favoring PCI Clinical characteristics: Severe co-morbidity, advanced age, frailty, reduced life expectancy, restricted mobility and conditions that affect rehabilitation process, patient preference. Anatomical and MVD with low SYNTAX score (0 to 22), low quality technical factors: or missing conduits for CABG, severe chest deformity or scoliosis, sequelae of chest radiation, porcelain aorta. 34 17
12/8/19 35 MAIN-COPMPARE Study: Mortality at 10 Years Park et al. J Am Coll Cardiol. (2018) 72:2813-2822. 36 18
12/8/19 37 19
Recommend
More recommend