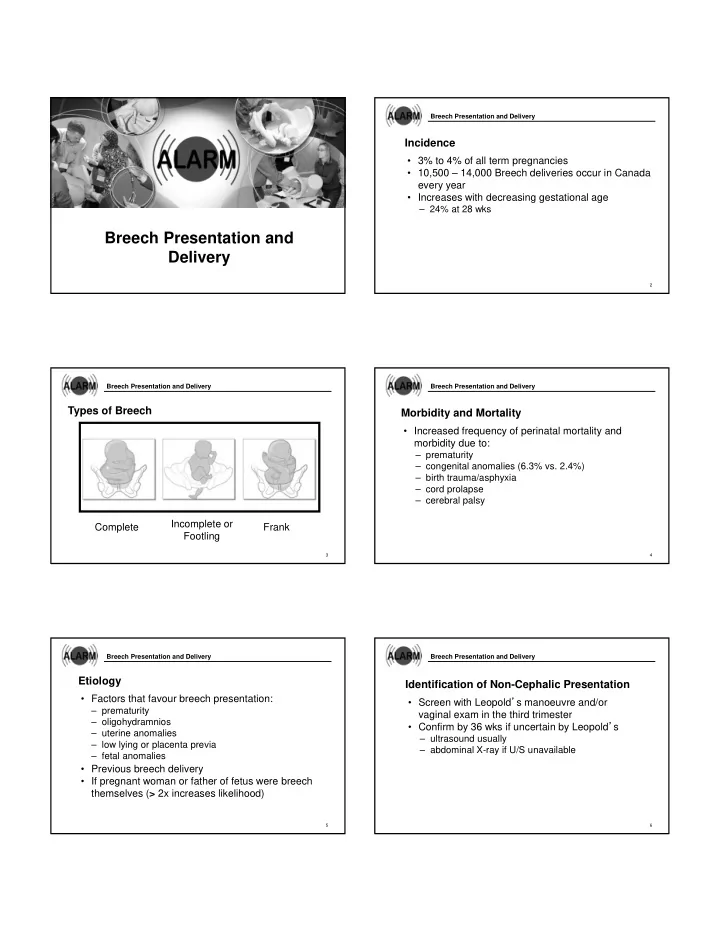
Breech Presentation and Delivery Incidence • 3% to 4% of all term pregnancies • 10,500 – 14,000 Breech deliveries occur in Canada every year • Increases with decreasing gestational age – 24% at 28 wks Breech Presentation and Delivery 2 Breech Presentation and Delivery Breech Presentation and Delivery Types of Breech Morbidity and Mortality • Increased frequency of perinatal mortality and morbidity due to: – prematurity – congenital anomalies (6.3% vs. 2.4%) – birth trauma/asphyxia – cord prolapse – cerebral palsy Incomplete or Complete Frank Footling 3 4 Breech Presentation and Delivery Breech Presentation and Delivery Etiology Identification of Non-Cephalic Presentation • Factors that favour breech presentation: • Screen with Leopold ’ s manoeuvre and/or – prematurity vaginal exam in the third trimester – oligohydramnios • Confirm by 36 wks if uncertain by Leopold ’ s – uterine anomalies – ultrasound usually – low lying or placenta previa – abdominal X-ray if U/S unavailable – fetal anomalies • Previous breech delivery • If pregnant woman or father of fetus were breech themselves ( > 2x increases likelihood) 5 6
Breech Presentation and Delivery Breech Presentation and Delivery External Cephalic Version (ECV) – Definition Term Breech Management Options are • A procedure whereby a fetus is turned in utero from 1. External Cephalic (ECV) a non-cephalic to a cephalic presentation by 2. CS manipulation of the maternal abdomen 3. Assisted Vaginal Breech Delivery • Meta-analysis comparing ECV at term to no attempt at ECV showed a significant reduction in: – non-cephalic births – CS • No significant effect on perinatal mortality or other measures of perinatal outcome 7 8 Breech Presentation and Delivery Breech Presentation and Delivery External Cephalic Version (ECV) – Timing External Cephalic Version (ECV) – Timing • 34-36 weeks vs > 37 weeks • Not before 34 weeks – fewer fetuses remain breech at delivery (51% vs – likely unnecessary as most turn spontaneously 59%) by term – 4% in delivery by CS – if emergency delivery indicated, NN morbidity – 2% in PTB < 37 weeks – no difference in NN morbidity – no perinatal deaths related to ECV – waiting allows spontaneous version to occur more often (25% vs 14%) 9 10 Breech Presentation and Delivery Breech Presentation and Delivery Prerequisites for ECV ECV Contraindications – Absolute • Singleton pregnancy • Any contraindications to labour • > 34 wks gestation • APH • No contraindication to labour • Some major anomalies • Fetal well-being established prior to procedure • Multiple gestation (except delivery of second twin) • Amniotic fluid volume adequate • Rupture membranes • Ultrasound available • Position of fetus confirmed • Facilities and personnel available for timely C/S 11 12
Breech Presentation & Delivery Breech Presentation and Delivery Risks of ECV ECV Contraindications – Relative • Abruption (0.4% – 1%) • Oligohydramnios • Rupture of membranes with possible cord • Hyperextension of the fetal head • ≥ 2 previous CS prolapse • Labour • Morbid obesity • FHR abnormalities; transient bradycardia (1.1% – • Active labour 47%) • Uterine malformation • Alloimmunization/fetomaternal hemorrhage (0%- • Fetal anomaly 5%) 13 14 Breech Presentation and Delivery Breech Presentation and Delivery ECV Procedure • Informed consent • Facility must have capability of performing immediate CS • U/S to confirm position and to monitor FHR throughout procedure • May lubricate abdomen with gel or powder 15 16 Breech Presentation and Delivery Breech Presentation and Delivery ECV – Possible Helpful Tools ECV Procedure • Tocolytics • STOP – evidence limited – patient too uncomfortable • Epidural or spinal analgesia – abnormal FHR – insufficient trials but some evidence to show • NST (even if attempt was unsuccessful) increased success (60% vs 35%) • Rh immunoglobulin • Moxibustion – conflicting evidence – some small trials support its use • Postural management (knee-chest) – not shown to be effective 17 18
Breech Presentation and Delivery Breech Presentation and Delivery Caesarean Section Planned CS for Breech – In Developed Countries Planned CS vs planned vaginal birth for breech Planned Planned presentation at term: LSCS vaginal birth • Lower risk of perinatal and neonatal mortality and neonatal morbidity with planned LSCS vs planned Perinatal or neonatal death 0/641 4/694 (0.6%) (excludes fetal anomalies) vaginal birth • e.g. 70% reduction in perinatal/neonatal death (RR Serious short term neonatal 2/514 (0.4%) 29/511 (5.7%) 0.29, 95% CI 0.10 – 0.86) morbidity 19 20 Breech Presentation and Delivery Breech Presentation and Delivery Term Breech Trial Revisited Term Breech Trial Revisited • Did not address the breech with anomalies or growth • Inadequate case selection and intrapartum restrictions management • Among survivors, there was no significant differences • Different skill levels amongst caregivers in outcomes at age 2 • Short term morbidity used as a surrogate marker • The reduction in peri/neonatal death was found mostly for long-term neurological impairment in developing countries with a baseline perinatal mortality > 20/1000 • No significant difference in perinatal or neonatal mortality in developed countries with low baseline perinatal mortality rates 21 22 Breech Presentation and Delivery Breech Presentation and Delivery Vaginal Breech Delivery – SOGC 2009 PREMODA Study • Vaginal breech birth can be associated with • 4x larger than Term Breech Trial increased perinatal mortality and short term NN • No difference in morbidity – perinatal mortality (0.08% vs 0.15%) – short term NN morbidity nearly always resolves – serious NN morbidity (1.6% vs 1.45%) – increase in perinatal mortality is small • 5 min Apgar < 4 higher in TOL vs C/S group (0.16% • Careful case selection and labour management may vs 0.02%) achieve a level of safety similar to elective CS • Long-term neurological outcomes do not differ by planned mode of delivery 23 24
Breech Presentation and Delivery Breech Presentation and Delivery Labour Management Vaginal Breech Delivery – Contraindications • Offered if EFW 2500-4000g • Cord presentation • Macrosomia – clinical pelvic examination – pre or early labour ultrasound • Presentation other than frank or complete breech – continuous EFM with flexed or neutral head – immediate vaginal exam with ROM • Clinically inadequate maternal pelvis - delay AROM • Fetal anomaly incompatible with vaginal delivery – oxytocin • Fetal growth restriction - induction not recommended 25 26 Breech Presentation and Delivery Breech Presentation and Delivery Risks/Complications with Vaginal Breech Delivery Management of Second Stage • Low 1 minute Apgar scores • Up to 90 minutes passive second stage • Entrapment of the fetal head • CS after 60 minutes of active pushing if delivery • Nuchal arms (0%-5%) not imminent • Cervical spine injury with hyperextended head • Active second stage to take place in or near OR • Cord prolapse (5%) • Health care provider for a planned vaginal breech delivery needs to possess the requisite skill and experience • NRP trained personnel in attendance for delivery 27 28 Breech Presentation and Delivery Breech Presentation and Delivery Entering the Pelvis Descent of the Breech Obstetrics - Normal and Problem Pregnancies, 2nd Edition Edited by SG Gabbe, JR Niebyl, JL Simpson. (1991) Obstetrics - Normal and Problem Pregnancies, 2nd Edition Edited by SG Gabbe, JR Niebyl, JL Simpson. (1991) 29 30
Breech Presentation and Delivery Breech Presentation and Delivery Spontaneous Expulsion Hurry up & Wait! • Spontaneous expulsion to • DON ’ T PULL! the umbilicus • Traction deflexes • The sacrum should be the fetal head gently guided anteriorly • May cause nuchal • Singleton breech arm extraction is contraindicated • CS is indicated for failure of descent or expulsion Obstetrics - Normal and Problem Pregnancies, 2nd Edition Obstetrics - Normal and Problem Pregnancies, 2nd Edition Edited by SG Gabbe, JR Niebyl, JL Simpson. (1991)) Edited by SG Gabbe, JR Niebyl, JL Simpson. (1991) 31 32 Breech Presentation and Delivery Breech Presentation and Delivery Deliver Legs by Pinard’s Manoeuvre; insert 2 Delivery of Arms fingers along one leg to the knee, then pushed away from midline (abducted) while flexing at hip • Good maternal pushing • Deliver when scapulae visible • Rotate to shoulder anterior • Sweep humerus across the chest and deliver • Rotate to other shoulder anterior and sweep second arm to deliver 33 34 Breech Presentation and Delivery Breech Presentation and Delivery Avoid Over-Extension Delivery of the Head • Mauriceau Manoeuvre • Flexion maintained with suprapubic pressure • Pressure on maxilla Obstetrics - Normal and Problem Pregnancies,2nd Edition Edited by SG Gabbe, JR Niebyl, JL Simpson. (1991) 35 36
Recommend
More recommend