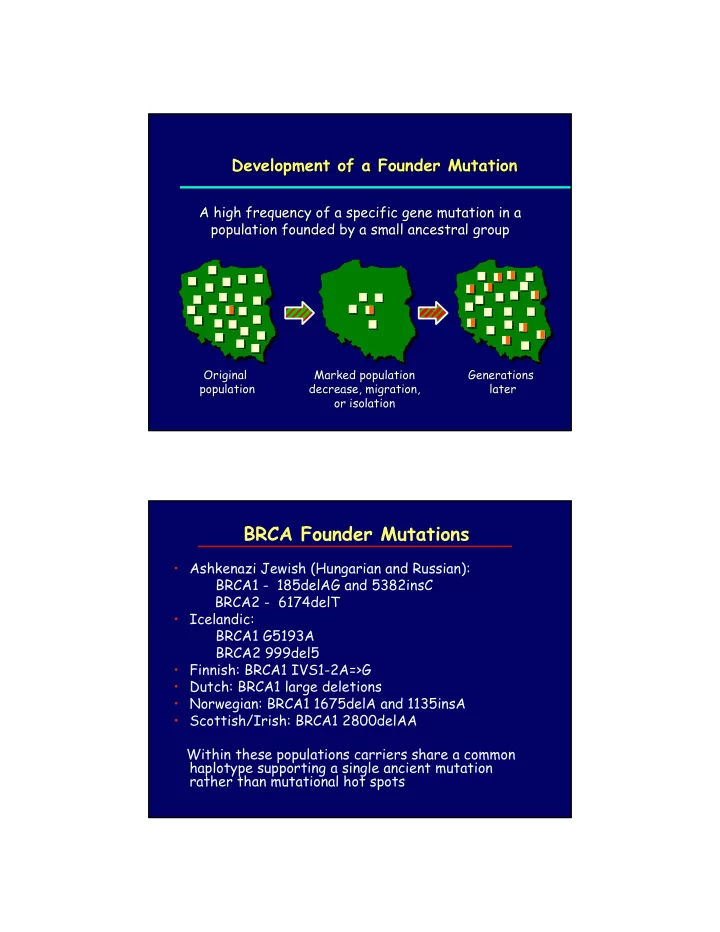
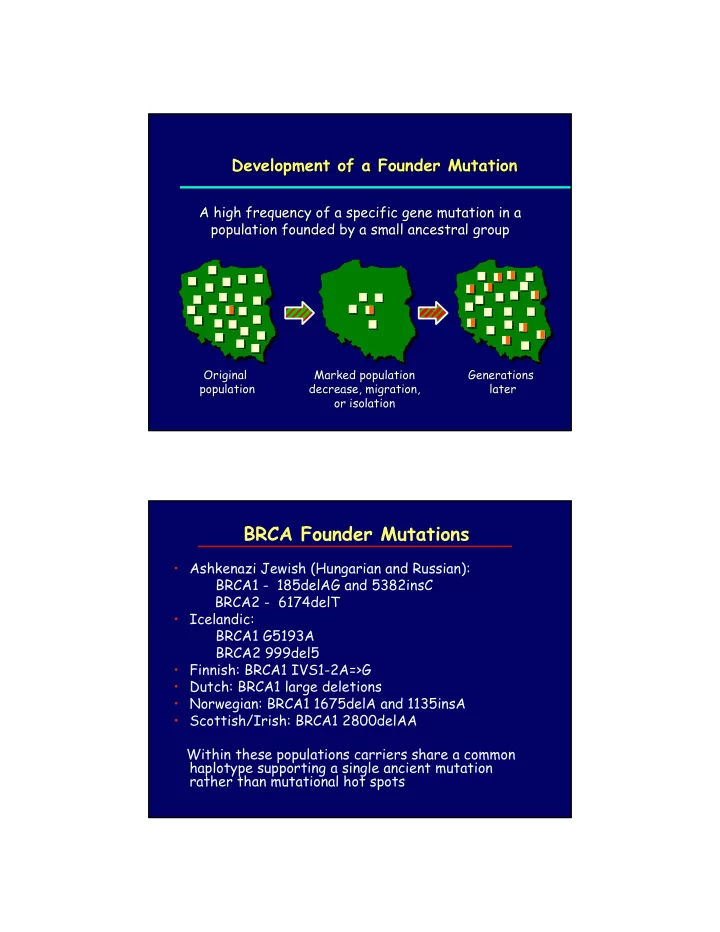
Development of a Founder Mutation Development of a Founder Mutation A high frequency of a specific gene mutation in a A high frequency of a specific gene mutation in a population founded by a small ancestral group population founded by a small ancestral group Original Original Marked population Marked population Generations Generations population population decrease, migration, decrease, migration, later later or isolation or isolation BRCA Founder Mutations • Ashkenazi Jewish (Hungarian and Russian): BRCA1 - 185delAG and 5382insC BRCA2 - 6174delT • Icelandic: BRCA1 G5193A BRCA2 999del5 • Finnish: BRCA1 IVS1-2A=>G • Dutch: BRCA1 large deletions • Norwegian: BRCA1 1675delA and 1135insA • Scottish/Irish: BRCA1 2800delAA Within these populations carriers share a common haplotype supporting a single ancient mutation rather than mutational hot spots
BRCA1 and BRCA2 • Estimated carriers of a deleterious mutation 1 per 1,000 • Breast cancer risk 35% – 80% by age 80 depending upon study population • Ovarian cancer risk 20% - 40% by age 80 • Founder mutations have been identified in: Icelanders Ashkenazi Fins African BRCA1 and BRCA2 Mutations in the Ashkenazi Jewish Population An estimated 1 in 40 Ashkenazi Jews An estimated 1 in 40 Ashkenazi Jews carries a BRCA1 carries a BRCA1 or or BRCA2 BRCA2 mutation mutation BRCA1 BRCA1 185delAG 5382insC 185delAG 5382insC Prevalence = ~1% Prevalence = ~0.15% Prevalence = ~1% Prevalence = ~0.15% BRCA2 BRCA2 6174delT 6174delT Prevalence = ~1.5% Prevalence = ~1.5% Roa Roa BB et al. BB et al. Nat Genet Nat Genet 14:185, 1996 14:185, 1996 Oddoux C et al. C et al. Nat Genet Nat Genet 14:188, 1996 14:188, 1996 Oddoux Struewing Struewing JP. JP. N N Engl Engl J Med J Med 336:1401, 1997 336:1401, 1997
Benefits, Risks, and Limitations Benefits, Risks, and Limitations of BRCA Testing of BRCA Testing Benefits Risks and Limitations Risks and Limitations Benefits • Does not detect Does not detect all all • Identifies high Identifies high- -risk risk • • mutations individuals individuals mutations • Identifies non Identifies non- - • Continued risk of • Continued risk of • carriers in families sporadic cancer sporadic cancer carriers in families with a known mutation with a known mutation • Efficacy of interventions Efficacy of interventions • Allows early Allows early • • unproven detection and detection and unproven prevention strategies prevention strategies • • May result in May result in • May relieve anxiety May relieve anxiety psychosocial psychosocial • or economic harm or economic harm Familial Clustering of Cancer Family history among blood relatives may reflect: • Presence of a single inherited genetic risk [APC] • Multiple genetic factors [BRCA + ATM] • Inheritance of genetic markers of metabolism • Shared environmental factors with/without inheritance of susceptibility [tobacco smoke] • Culturally transmitted risk factors [reproductive decisions, hormone use]
Genetic Epidemiology •Multiple cases in some families may be due to: inherited susceptibility, environmental exposures, lifestyle, reproductive patterns, health behaviors, etc •Understanding these causal patterns will assist in defining avenues for prevention and optimum treatment. •Data and biospecimens from family members are essential for g enetic and environmental studies •A confidential centralized data repository with DNA samples is required for groundbreaking research Factors Affecting Genetic Testing Decisions • Cost of counseling & testing • Concerns about health & life insurance • Confidentiality of test results • Family dynamics • Barriers to screening/testing (financial/psychological) • Clinical decision-making: a burden for mutation carriers • Unresolved grief • Survivor guilt among non-carriers • Patient/physician/counselor communication
Disparities in Genetic Testing •African American women have been less likely to receive genetic counseling and testing than Caucasian women OR 0.3 [0.1 -0.9] •Myriad Genetics: among the first 10,000 individuals tested for BRCA mutations, <10% were from under-represented racial/ethnic subgroups •Access and knowledge increases use of genetic testing to wealthy, well-insured and medically well informed populations. •To correct disparities genetic services must be racially and culturally tailored to meet the needs of specific populations •Federally –funded low cost preventive health programs are needed to provide reliable estimates of inherited risks & genetic penetrance Hall MJ, Olopade OI. JCO 2006;24: Disparities in Genetic Testing Factors potentially contributing to low acceptance of genetic services by some racial/ethnic populations: •Limited communication among family members restricting awareness of diseases diagnosed among relatives •Inaccurate personal assessment of disease risk •Lack of knowledge of inherited risk in predicting future disease •Inadequate understanding of the value of genetic counseling & testing •Highly technical genetic services may not be available in local setting •Distrust of risk reduction interventions coupled with greater reliance on religion Hall MJ, Olopade OI. JCO 2006;24
Risk Models May Be Inadequate for Some Racial/Ethnic Groups •Predictive statistical models using family history have been developed primarily with data from white families & may not be applicable to diverse populations •Models are based upon accurate estimates of population- specific prevalence of high-risk genotypes – data not available for most minority populations due to limited genetic testing •Heterogeneity within African American and other minority populations may also complicate estimates Concerns Associated with Genetic Testing •Fears of genetic discrimination by employer or insurance company •High cost if self pay considered •Confidentiality of genetic results in medical records &/or among relatives •Limited laws protecting genetic information •Fear of recommended screening methods & their frequency •Distrust/distaste for preventive medications or surgery •Potential need for psychological assessment and support not covered by health insurance
Breast-Ovarian Ashkenazi Family Mother & Daughter with 5382insC Stomach Ov 70 Br 80 Br 70 Br 32 88 50 65 64 Ov 59 Br 34,39 65 Br 36,43 Ov 58 Ov 59 5382insC 41 36 34 No Mutation Br 34 5382insC Family 5-37 Racial & Ethnic Differences May Impact Inherited Factors & Environmental Exposures Environment Environment Exposures Exposures Affected Affected Genetic Factors Genetic Factors Manipulation of environmental exposures can modify risk of developing breast cancer
Paired Sisters Discordant for Breast Cancer Resource for Gene-Environment Studies 84 83 Breast 66 Ovarian 54 Br 50 55 56 Br 57 35 Br 34 32 NY Registry: 450 families with one or more discordant sister sets including 120 BRCA carrier families DNA Repair Capacity in Paired Sisters Discordant for Breast Cancer • % DNA repair capacity of lymphoblastoid cell lines derived from samples donated by 158 case and 154 control sisters from 137 NY Registry families • Conditional logistic regression controlled for potential confounding due to age at blood donation, body mass index, and smoking • Mean repair capacity was lower in sisters with breast cancer compared to unaffected siblings [difference=8.6,95% CI 4.3,13.8] 84 Breast 72 56 Br 50 Kennedy etal. JNCI 2005;97:127-32
Recommend
More recommend