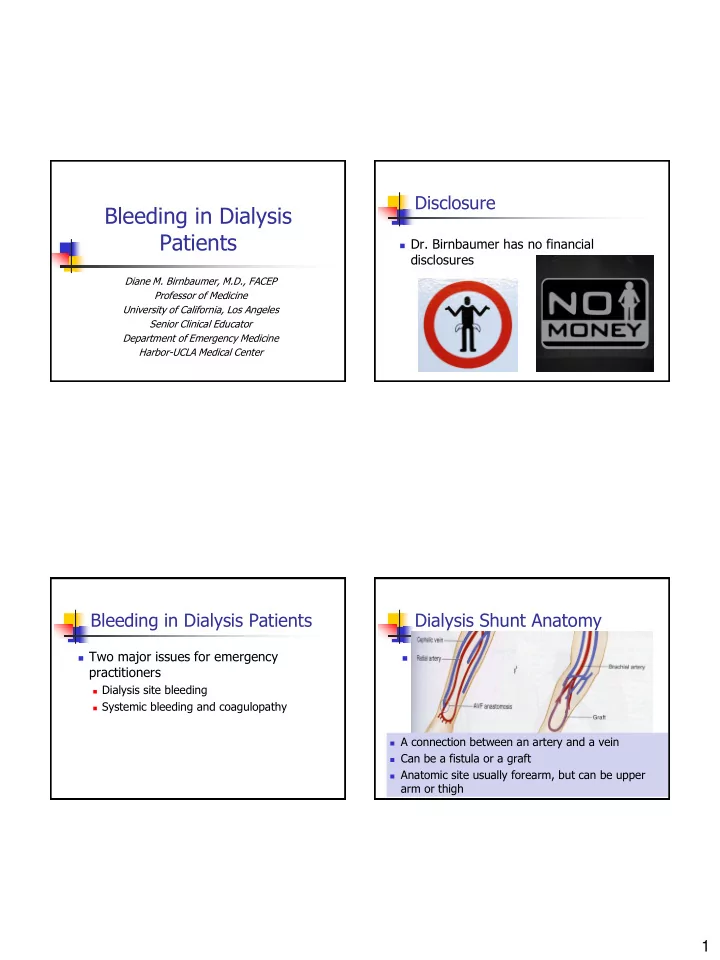
Disclosure Bleeding in Dialysis Patients Dr. Birnbaumer has no financial disclosures Diane M. Birnbaumer, M.D., FACEP Professor of Medicine University of California, Los Angeles Senior Clinical Educator Department of Emergency Medicine Harbor-UCLA Medical Center Bleeding in Dialysis Patients Dialysis Shunt Anatomy Two major issues for emergency Shunt anatomy practitioners A connection between an artery and a vein Dialysis site bleeding Can be a fistula or a graft Systemic bleeding and coagulopathy Anatomic site usually forearm, but can be upper arm or thigh A connection between an artery and a vein Can be a fistula or a graft Anatomic site usually forearm, but can be upper arm or thigh 1
Dialysis Shunt Anatomy Dialysis Shunt Anatomy AV fistula AV fistula Direct subcutaneous anastomosis of an artery Radial-cephalic (Brascia- and vein without prosthetic material Cimino forearm) most commonly used Preferred means of vascular access for Venous portion receives hemodialysis high pressure, becomes arterialized Typically end-to-side (hypertrophied and vein-to-artery dilated), then suitable for dialysis Dialysis Shunt Anatomy Dialysis Site Bleeding AV graft: AV A potential life threat bridge using a A very high pressure system donor vein or Can be from three types of breaks in the site synthetic integrity material Repeated access punctures Pseudoaneurysms True aneurysms Timing after dialysis helpful in determining type of bleeding 2
Dialysis Site Bleeding Dialysis Site Bleeding Bleeding immediately after dialysis The balance Often due to puncture site Stop the bleeding Easiest to manage Do not compromise the shunt Bleeding between dialyses More concerning However, if the bleeding is life threatening, May be due to shunt infection, clotting of the shunt is an acceptable risk to pseudoaneurysm or true aneurysm rupture save the patient’s life Can bleed to death in minutes Dialysis Site Bleeding Dialysis Site Bleeding Approach to bleeding The basics Very little published on the topic Resuscitation, including IV access with fluids and blood products, may be necessary Many of the recommendations are based on anecdote and opinion Consultation with a vascular surgeon may be necessary if bleeding cannot be controlled in the ED 3
Dialysis Site Bleeding Dialysis Site Bleeding Direct pressure to the site of bleeding for Put pressure directly at the site of a minimum of 5 minutes bleeding with fingertip or folded gauze pad Holes are usually small (from dialysis needle) If true aneurysm or pseudoaneurysm ruptures, patient can rapidly exsanguinate Dialysis Site Bleeding Bleeding in Dialysis Patients AVOID bulky dressing or using elastic Direct pressure on feeding vessels bandages as they lead to increased risk of Digital pressure over feeding and draining clot formation in the dialysis access vessels above and below bleeding site Wrong Way 4
Bleeding in Dialysis Patients Bleeding in Dialysis Patients Direct pressure on feeding vessels If tunnel catheter is bleeding, pressure should be at site of vascular insertion (if AVOID proximal occlusion (e.g. BP cuff, possible), NOT at subcutaneous exit site tourniquet) unless absolutely necessary Not possible with subclavian catheters Bleeding in Dialysis Patients Bleeding in Dialysis Patients Suture Suture Adequate visualization is crucial to localize Subcutaneous injection of bleeding site with bleeding site lidocaine with epinephrine Digital pressure to proximal and distal Figure-of-eight or horizontal mattress suture ends of shunt or fistula with 4-0 nonabsorptive suture using a noncutting needle Pneumatic blood pressure cuff Suture as superficially as possible to prevent Distal to fistula or graft (impedes distal-to- damage to graft/fistula proximal arterial flow), or proximal to a loop graft Remove suture in several days 5
Bleeding in Dialysis Patients Suture May require venogram to evaluate patency before next use Bleeding in Dialysis Patients Bleeding in Dialysis Patients Thrombogenic agents Vasoconstrictive agents Not effective for massive bleeding Subcutaneous injection of 2-4 mL lidocaine with epinephrine in a wheel around bleeding Best used for residual oozing remains after site other methods to control bleeding May vasoconstrict and Apply directly to site of oozing and hold in and / or compress place May pose a potential site for future infection 6
Bleeding in Dialysis Patients Bleeding in Dialysis Patients Chemical cautery Correcting coagulopathy Not effective for massive bleeding If massive bleeding that cannot be controlled with above Use for residual oozing as with thrombogenic agents Consider DDAVP (for uremic platelet dysfunction) Consider reversing other anticoagulants as Silver nitrate directly at site indicated Dry area first as much Heparin (used in dialysis) as possible Warfarin Do not apply aggressively as Novel oral anticoagulants – extremely difficult to reverse may dislodge or dissolve clot and contraindicated in renal failure patients, so patients should not be on these agents Bleeding in Dialysis Patients Bleeding in Dialysis Patients After the bleeding stops After the bleeding stops Patient should be observed for 1-2 hours for There are no possible rebleeding recommendations regarding how or when Rare if bleeding from puncture site is controlled in ED to evaluate the access for patency after More likely if bleeding was from pseudoaneurysm / true aneurysm; these patients may need to be treatment for bleeding observed longer 7
Bleeding in Dialysis Patients Bleeding in Dialysis Patients Coagulopathy Treatment of uremic platelet dysfunction Uremia causes platelet dysfunction by Desmopressin (DDAVP) mechanisms that are not entirely clear Dose for uremic platelet dysfunction is 0.3 µg/kg IV single dose or every 12 hours Uremia alone not usually a significant issue, Onset of action is 1-2 hours but added anticoagulants increase the risk of Duration of action is 6-8 hours bleeding Costly May cause anaphylaxis, water intoxication or hyponatremia, or rare thrombotic events Bleeding in Dialysis Patients Bleeding in Dialysis Patients Cryoprecipitate Heparin-associated coagulopathy May be useful, but DDAVP is preferred 3000-5000 units of heparin are used during dialysis and are stopped 1 hour before the end of a dialysis session Usually not an issue in the ED unless patient starts to bleed during dialysis If necessary, can reverse with protamine sulfate 1 mg per 100 units of heparin If patient on LMWH, use 1 mg per 1 mg of LMWH, but is less effective 8
Bleeding in Dialysis Patients Bleeding in Dialysis Patients Warfarin-associated coagulopathy (in Tranexamic acid patients with severe or life-threatening Minimal data on its use in renal failure bleeding) patients At this point, probably should not be used Administer prothrombin complex concentrates (4-factor preferred) – low volume, much more Reversing NOACs rapid than FFP Contraindicated in renal failure Vitamin K 5-10 mg IV (takes 12 hours for Very few options for reversal at this point effect) FFP an option, but high volumes (1-2 liters), takes time to thaw and administer Bleeding in Dialysis Patients Bleeding in Dialysis Patients Take Home Points Take Home Points Bleeding from dialysis access can be life Clotting of the access site is a potential threatening complication of treatment of significant bleeding A systematic approach starting with direct pressure is effective in most cases of Uremic platelet dysfunction can be treated bleeding from vascular access sites in with DDAVP, but little data exists dialysis patients regarding when it is truly indicated 9
Bleeding in Dialysis Patients Take Home Points Thank You For Your Attention! Dialysis patients on warfarin with severe or life-threatening bleeding may need to be reversed, preferably using prothrombin complex concentrates 10
11
12
13
14
Recommend
More recommend