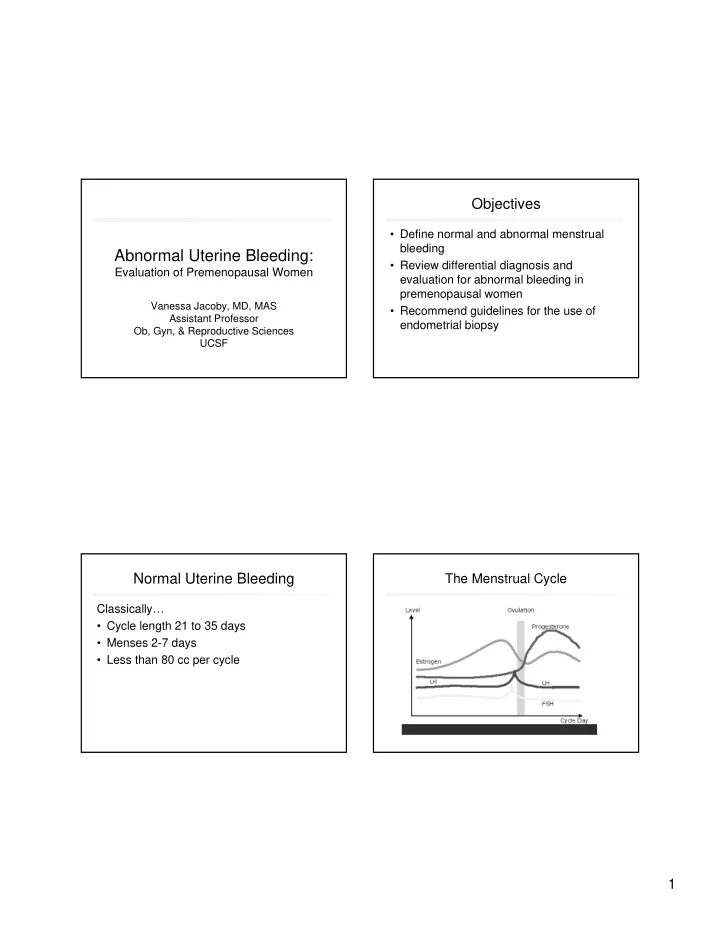
Objectives • Define normal and abnormal menstrual bleeding Abnormal Uterine Bleeding: • Review differential diagnosis and Evaluation of Premenopausal Women evaluation for abnormal bleeding in premenopausal women Vanessa Jacoby, MD, MAS • Recommend guidelines for the use of Assistant Professor endometrial biopsy Ob, Gyn, & Reproductive Sciences UCSF Normal Uterine Bleeding The Menstrual Cycle Classically… • Cycle length 21 to 35 days • Menses 2-7 days • Less than 80 cc per cycle 1
Case 1 Classic Definitions A 24 year old G0 presents with heavy irregular Excess Bleeding bleeding for 6 months. Her bleeding is every • Menorrhagia: heavy, regular timing 15-35 days, lasts 4-15 days. • Metrorrhagia: light, frequent intervals • Menometrorrhagia: heavy, frequent, irregular She has… • Polymenorrhea: regular, <24 days apart A. Menorrhagia • Intermenstrual spotting: bleeding between menses B. Dysfunctional uterine bleeding (DUB) Decreased bleeding C. Menometrorrhagia • Oligomenorrhea: bleeding >35 days apart Challenges with Classic Definitions Dysfunctional Uterine Bleeding • Excessive noncyclic bleeding not caused • Data is from women in Minnesota, 1930s by anatomic lesion, medications, pregnancy or systemic disease • Lack of uniformity across clinical settings • Primarily due to anovulation Treloar EA, Boynton, Int J Fertil 1967 Hallberg L, Hogdahl AM et al, Acta Obstet Gynecol Scand 1966 2
Challenges with Classic Definitions New Descriptive Terms for AUB • International meeting of experts 2007 Clinical Dimensions Descriptive Terms Normal limits (5 th to 95 th percentiles) (Menstrual Agreement Process) Frequent <24 FREQUENCY (days) Normal 24-38 Infrequent >38 • Recommendations: Absent - – Discontinue use of classic terms REGULARITY Regular Variation +2-20 days Cycle to cycle variation over Irregular Variation >20 days – Use descriptive terms that patients 1 year understand Prolonged >8 DURATION (days) Normal 4.5-8 – Create uniformity for research Shortened <4.5 Heavy >80 VOLUME (monthly mL) Normal 5-80 Fraser I, Critchley H, et al Fertil Steril 2007 Light <5 Fraser I, Critchley H, et al Fertil Steril 2007 Case 2 Evaluation: premenopausal women A 33 yo G1P1 with regular, normal periods Four steps: but three months of light spotting in 1) Is it uterine? between periods. Spotting is 5-9 days a 2) Is she pregnant? month, randomly distributed between 3) Describe the bleeding. cycles. She uses a copper IUD for 4) Is it ovulatory? contraception. What is the differential diagnosis? 3
FIGO Classification: PALM-COEIN Evaluation: premenopausal women – Fraser I, Hilary OD, et al Fertil Steril 2007 Four steps: 1) Is it uterine? • Detailed history to r/o GI/GU sources • Exam to r/o obvious vulvar, vaginal, cervical lesions • Up to date Pap smear Munro et al, Fertil Steril 2011;95:2204–8 Case 2 Evaluation: premenopausal women During the pelvic exam, the patient is noted to Four steps: have a 2cm cervical polyp which is removed in 1) Is it uterine? the office. She has full resolution of her bleeding at 6 week follow-up. 2) Is she pregnant? Check pregnancy test in at-risk women 4
Case 3 Evaluation: premenopausal women A 41 yo G3P2 with 4 months of abnormal Four steps: bleeding. Regular cycle length every 29-32 1) Is it uterine? days, lasts 7 days, but bleeding is heavy. 2) Is she pregnant? She changes a tampon every hour for the 3) Describe the bleeding. first 3 days and has to get up at night to • Detailed history will guide w/u and treatment change tampons/pads. • Consider menstrual calendar X 2-3 cycles Case 3 Tips to assess bleeding history Factors associated with heavy bleeding: A 41 yo G3P2 with 4 months of abnormal bleeding. Regular cycle length every 29-32 days, lasts 7 1. Bleeding history (but only 34% with “heavy days, but bleeding is heavy. She changes a bleeding” had EBL >80cc) tampon every hour for the first 3 days and has to 2 Change pads/tampons <3 hour intervals get up at night to change tampons/pads. 3. High number of pads/tampons per cycle (>21) 4. Require change of tampon/pad during night Bleeding is REGULAR in timing and duration but 5. Have clots >1 inch HEAVY volume (menorrhagia). Warner, Critchley et al, Am Jo Obstet Gynecol, 2004 5
Evaluation: premenopausal women Classic Definitions Four steps: Ovulatory 1) Is it uterine? • Menorrhagia: heavy, regular timing 2) Is she pregnant? • Polymenorrhea: regular, <24 days apart • Intermenstrual spotting: bleeding between regular 3) Describe the bleeding. menses Anovulatory 4) Is it ovulatory? • Metrorrhagia: light, frequent intervals – Regular intervals • Menometrorrhagia: heavy, frequent, irregular • Moliminal symptoms • Oligomenorrhea: bleeding >35 days apart • Intermenstrual spotting: bleeding between menses Ovulatory AUB Ovulatory AUB: Differential Diagnosis OVULATORY AUB GnRH Hypothalamic-pituitary- ovarian axis intact Bleeding disorder/ Anatomic Idiopathic Medication Fibroids VonWillibrands Adenomyosis ITP Coumadin Polyps 6
Ovulatory AUB: History Ovulatory AUB: Physical exam • Medical comorbidities • Medications • Thyroid symptoms (see Thyroid slides) • Disorder of hemostasis – Heavy menses since menarche OR – History of postpartum hemorrhage, bleeding with surgery/dental work OR – 2 or more of the following---bruising >5cm or epistaxis 1-2/month, frequent gum bleeding, family history of bleeding Kouides P, Conrad J, et al, Fertil Steril 2005 Fibroids Adenomyosis Ovulatory AUB: Blood tests Ovulatory AUB: Imaging Options • Pelvic ultrasound vs. MRI • CBC, TSH • In 108 premenopausal women with ovulatory AUB scheduled for • Screen for disorders of hemostasis according hysterectomy: *both performed well for fibroid detection to history or if pt plans major surgery *MRI better for exact fibroid location – PT, APTT – VWF antigen, ristocetin cofactor, factor VIII DETECTION OF FIBROIDS Pelvic Ultrasound Pelvic MRI Sensitivity (%) 99 99 Specificity (%) 91 86 Kouides P, Conrad J, et al, Fertil Steril 2005 Positive predictive value (%) 96 92 Negative predictive value 97 97 (%) Dueholm, et al, Am J Obstet Gynecol:2002 7
Ovulatory AUB: Imaging Options Case 3 Overall evaluation of endometrial cavity: A 41 yo G3P2 with 4 months of abnormal bleeding. Regular cycle length every 29-32 days, lasts 7 days, but bleeding is heavy. She MRI, Hysterosalpingogram (HSG), hysteroscopy superior to US changes a tampon every hour for the first 3 days and has to get up Endomterial polyps: HSG and hysteroscopy superior to MRI and US at night to change tampons/pads. Submucosal fibroids: MRI superior to all Bleeding is REGULAR in timing and duration but HEAVY volume (menorrhagia). EVALUATION OF UTERINE CAVITY MORPHOLOGY Pelvic Pelvic MRI HSG Hysteroscopy • No PMH Ultrasound • No medications Sensitivity (%) 69 76 83 84 • Exam: nl size uterus Specificity (%) 83 92 90 88 • Hct 29 PPV(%) 85 80 71 86 NPV (%) 89 91 82 86 Dueholm, et al, Fert Sterility, August 2001 Submucosal Fibroid: Ovulatory AUB: Treatment Ultrasound vs. MRI Proven benefit in randomized trials: SURGICAL MEDICAL Endometrial Ablation NSAID Hysterectomy Tranexamic Acid Fibroids Hormonal contraception Myomectomy Cyclic progestin Uterine Artery Embolization LNG-IUD (more effective than other hormonal treatment or NSAIDs) GnRH agonists Mifepristone (fibroids) No randomized trials to date: SURGICAL MEDICAL MR Guided Focused Ultrasound Myolysis 8
Case 4: Ovulatory bleeding Ovulatory AUB: Medicine vs. Surgery 49 yo G2P2 with 5 months of heavy In meta-analysis of 12 randomized trials (n=1,049 women): -- 58% of “medical management” group had undergone surgery bleeding. Regular cycle length and within 2 years. duration, but heavy bleeding – Surgery (hysterectomy or endometrial ablation) decreased bleeding more than oral medication. resulting in significant anemia with – LNG-IUD comparable to surgery for improvement in quality of life. hct of 25%. Marjoribanks J, et al, Surgery versus medical therapy for heavy menstrual bleeding. Cochrane Does she need an endometrial biopsy? Database of Systematic Reviews 2006. 1) Yes 2) No Case 5: Anovulatory bleeding Endometrial Biopsy 38 yo G2P2 with 5 months of irregular Endometrial Cancer Facts bleeding. Bleeding is every 2-3 weeks, • 4th most common cancer in lasts 5-12 days, and heavy. Has to women (2.5% lifetime risk) change tampon every 1-2 hours for the • Average age 61 but 25% first few days . occur pre-menopausally Does she need an endometrial biopsy? • Rare to have cancer without abnormal bleeding 1) Yes • Risk factors: unopposed estrogen (anovulation), 2) No obesity, nulliparity, diabetes, hypertension 9
Recommend
More recommend