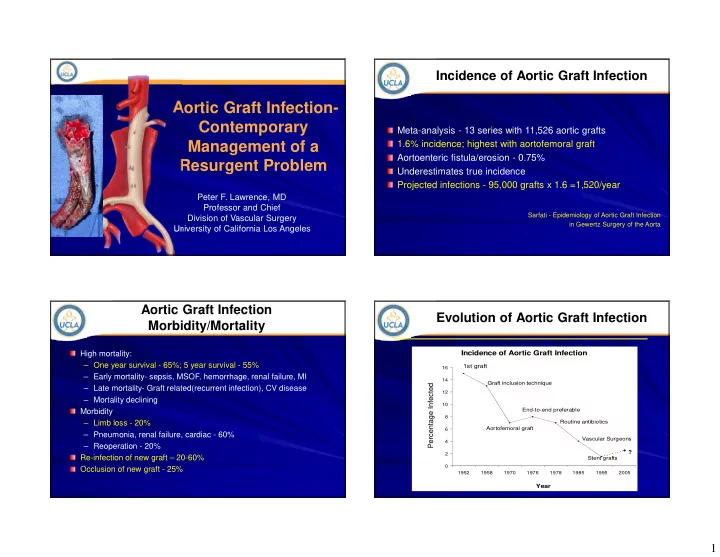
Incidence of Aortic Graft Infection Aortic Graft Infection- Contemporary Meta-analysis - 13 series with 11,526 aortic grafts Management of a 1.6% incidence; highest with aortofemoral graft Aortoenteric fistula/erosion - 0.75% Resurgent Problem Underestimates true incidence Projected infections - 95,000 grafts x 1.6 =1,520/year Peter F. Lawrence, MD Professor and Chief Sarfati - Epidemiology of Aortic Graft Infection Division of Vascular Surgery in Gewertz Surgery of the Aorta University of California Los Angeles Aortic Graft Infection Evolution of Aortic Graft Infection Morbidity/Mortality High mortality: Incidence of Aortic Graft Infection – One year survival - 65%; 5 year survival - 55% 1st graft 16 – Early mortality- sepsis, MSOF, hemorrhage, renal failure, MI 14 Graft inclusion technique Percentage Infected – Late mortality- Graft related(recurrent infection), CV disease 12 – Mortality declining 10 Morbidity End-to-end preferable 8 – Limb loss - 20% Routine antibiotics Aortofemoral graft 6 – Pneumonia, renal failure, cardiac - 60% Vascular Surgeons 4 – Reoperation - 20% ? 2 Re-infection of new graft – 20-60% Stent grafts 0 Occlusion of new graft - 25% 1952 1958 1970 1976 1978 1985 1995 2005 Year 1
Endograft Infection: The New Diagnosis – Direct Culture and Epidemic? Graft Exploration Increasing reports of endograft infection (~35 papers since 2005) Infected grafts show lack of Incidence ranges from 0.2 to 0.7% incorporation, purulent exudate, and Absence of incorporation is “ gold 1431 aortic endografts placed evaluated with 11 a perigraft capsule standard ” endograft infections (EVAR + TEVAR)= 0.6% Gram stain may help with operative decision Graft culture may include sonication Ducasse et al Ann Vasc Surg 2004 Hobbs et al J Cardiovs Sur 2010 Sharif et al JVS 2007 Cernohorsky JVS 2011 Diagnosis: Computed Diagnosis: Endoscopy Tomography GI bleeding common Characteristic appearance - collections of fluid or air following aortic surgery around graft (21%) Air and fluid are normal GEF comprise only 1% of immediately postop, but GI bleeders diminish over time Endoscopy indicated in all Lack of air and fluid helps stable patients with an exclude graft infection aortic prosthesis and GI bleeding 2
Diagnosis: DSAngiography Diagnosis of Aortic Graft Infection: Radiologic Nuclide Scans (Indium 111) (or CTA/MRA) Useful in stable patients Identifies graft infections Depends on intense inflammatory response, so better for associated with anastomotic virulent bacteria false aneurysms and graft occlusions Confirms presence or absence of infection Nonspecific for graft infection Determines extent of infection Useful in planning surgery for May identify other sites of infection stable patients + for 2-3 weeks postop in normal patients PET and SPECT scan being reported in Europe for 3-D scanning Indium 111 Leukocyte Diagnosis Typical Patient of Aortic Graft Infection 57 YO woman underwent uncomplicated - + aorto-bifemoral bypass with PTFE for claudication in 2004 – Rx ’ ed with steroids-24 ops – Severe rheumatoid arthritis, + 12 0 Scan – Heavy smoker for 45 years - – + troponins in post op period 2 – Rx ’ ed with sartorius muscle flap 13 – Post op right groin infection Indeterminate = 4 Two month history of spontaneous drainage from right inguinal region Recent left groin erythema Lawrence, PF . J. Vasc Surg 1985 3
Treatment Definitive Graft Infection Treatment – Less Invasive Approaches Excision Without Revascularization Entire graft removal is conventional IV / topical antibiotics approach; revascularization not always required Muscle coverage without If graft thrombosed, then removal graft excision alone is OK Drainage with Abx irrigation May also work when indication was claudication or proximal anastomosis VAC was E-S Replacement with Abx Aortic aneurysms unlikely to tolerate graft removal alone bonded femoral graft 15/101 patients in one series Never “cure” infection not revascularized Seminars in Vascular Surgery 2011 Test to Determine Graft Excision with Revascularization Need Extra-anatomic Revascularization 1st described by Blaisdell in 1961 Segmental pressures for Gold standard for aortic infection multilevel disease involving more than isolated area of Ankle pressure > 40 and graft ABI with graft occlusion/ Early results resulted in 40% compression mortality and 25% amputation Ankle pressure > 40 and Recent results with improved ABI with angiographic anesthesia and sequencing of balloon occlusion procedures have 25% mortality 4
Staged Treatment of Aortic Graft Extraanatomic Bypass Infection Graft Thrombosis: 10-20% at 5 years Graft Residual or reinfection: 5-20% at 5 years Aortic stump disruption: 0-5%, but may occur years later Revascularization precedes graft excision by 1-2 days This image cannot currently be displayed. Eliminates period of prolonged ischemia Allows for better hemodynamic stability Rests surgical team Does not result in increased graft infection rate Reilly J Vasc Surg 1987 McCann Ann Surg 1993; Bunt Cardiovasc Surg 1993; Lawrence 1984 Revascularization with Prosthetic Insitu Replacement Autogenous Tissue (venous) Not appropriate when suture line is involved with bleeding Major risk is recurrent infection Debridement of infected aortic wall is critical Most appropriate for patients with normal defenses and no extensive purulence Best prosthesis is antibiotic bonded Dacron, using Rifampin with a gelatin bond Jicha, Reilly, Goldstone JVS 1996 Lachapelle J Vasc Surg 1994 5
In Situ Replacement with Femoral NAIS Results Veins (NAIS) Major Patients Follow-Up 30-day Study Amputatio (n) (Months) Mortality n Clagett 21 23 10% 10% (1993) Ehsan 48 56 2% 0% (2009) Popularized by Claggett and colleagues at Southwestern “Neoaortoiliac system” (NAIS) Ali (2009) 144 32 10% 7% Insitu Revascularization NAIS Results with Allograft Reported 9% mortality and 5% amputation rate Used with all organisms Mean age = 65 ± ± 9 years ± ± Peripheral edema occurs, but usually 1988-2002 controllable Indication for allograft use: Good durability 179 Patients – Primary graft infection (n=125, 70%) Long procedure(10-12 hrs) – Secondary aorto-enteric fistula (n=54, 62% of patients underwent 3 ± ± ± ± 2 30%) Cryopreserved Fresh allograft: Clagett GP J Vasc Surg 1997 repeat operations before allograft allograft: 111 Patients 68 Patients replacement 6
Kieffer E, et al Cyropreserved Allograft Previous aneurysm concerns have been addressed with changes in preservation Late mortality = 25.9% (allograft-related Options include Cryovein and Cryoartery = 2.1%) – All 3 patient deaths were due to Expensive- are Cryoartery costs justified by better outcomes? allograft rupture at 9, 10, and 27 months. – 2 patients received fresh allograft (66%) Allograft-related complications are significantly reduced by using cryopreserved allografts rather than fresh allografts Advantages of CryoArtery vs. Uses of Allograft Cryovein for In-Line Reconstruction Thicker wall vs. vein conduit – Durable material--less rupture risk – Less risk for recurrent infection Excellent fit: available as bifurcated conduit Expensive but cost-competitive – Does not require time in OR for construction of neo-aortoiliac segment Duncan, et al, Allograft registry; JVS 2003 7
Technique Explanted Graft • Need proximal and distal control above and below the infection • Often requires supra-celiac clamping • Opening the retroperitoneum may still result in significant bleeding • Necrotic tissue requires debridement • Sew up to the orifices of the renal arteries • Occasionally need autogenous transplant of renal arteries Aortic Graft Infection: Single-Institution (UCLA) Experience The Use of Cryopreserved Aortoiliac Allograft for Aortic Reconstruction in the United States On behalf of the Investigators Vardanian AJ et al, Am Surgeon 2009 8
Results Procedure Details 220 Patients at 14 institutions (M:F = 1.6/1, Mean age = 65 ± 12 yrs) Operative Variable (N=220) n (%) Type of Initial Aortic Procedure n (%) Graft Excision Open reconstruction 209 (95%) Full excision 149 (68%) Endovascular 11 (5%) Distal Anastomosis Bilaterally to external iliac artery 139 (63%) Indication for Use of CAA n (%) Bilaterally to femoral artery 66 (30%) Prosthetic graft infection 134 (61%) Unilateral to femoral and external iliac artery 15 (7%) Concomitant Procedures with CAA Placement Primary abdominal aortic infection 35 (16%) Femoral artery to distal artery bypass 42 (19%) Graft enteric fistula/erosion 33 (15%) Duodenal repair or colon resection 7 (3%) Infection pseudoaneurysm 9 (4%) Other vascular procedures 32 (15%) Other, including high risk of graft infection 9 (4%) Technique Early and Late Complications Complication (n = 55) n (%) Persistent sepsis 17 (8%) 92% 86% CAA thrombosis/occlusion 9 (4%) 80% 71% CAA rupture 8 (4%) Recurrent CAA infection 8 (4%) CAA pseudoaneurysm 6 (3%) Fistula recurrence 4 (2%) Lower extremity 1 (<1%) compartment syndrome Mean follow-up = 30 ± 3 months Colonic perforation 1 (<1%) Lower limb ischemia 1 (<1%) Range = 1 to 160 months 9
Recommend
More recommend