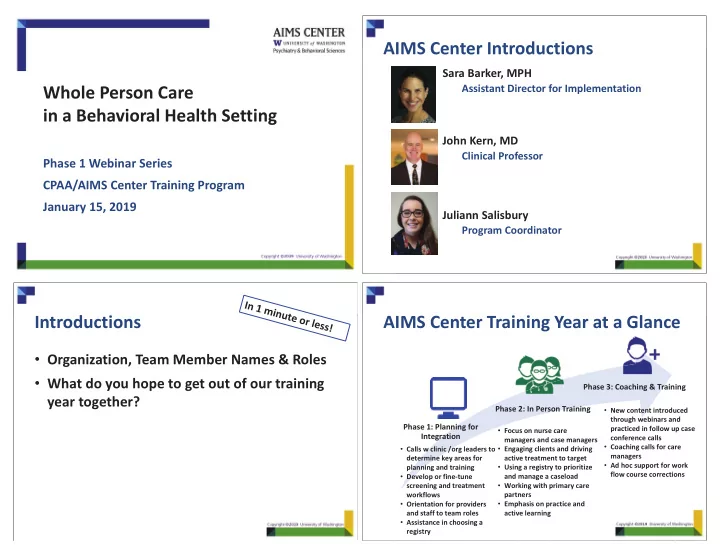
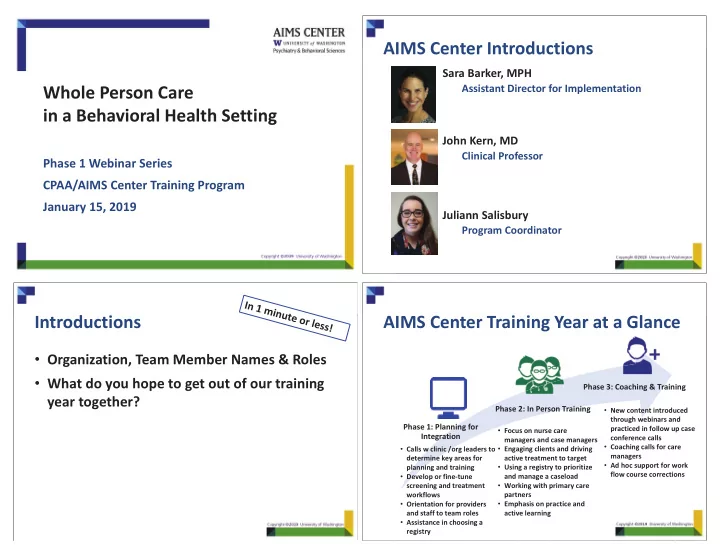
AIMS Center Introductions Sara Barker, MPH Assistant Director for Implementation Whole Person Care in a Behavioral Health Setting John Kern, MD Clinical Professor Phase 1 Webinar Series CPAA/AIMS Center Training Program January 15, 2019 Juliann Salisbury Program Coordinator Introductions AIMS Center Training Year at a Glance • Organization, Team Member Names & Roles • What do you hope to get out of our training Phase 3: Coaching & Training year together? Phase 2: In Person Training • New content introduced through webinars and Phase 1: Planning for practiced in follow up case • Focus on nurse care Integration conference calls managers and case managers • Coaching calls for care • Calls w clinic /org leaders to • Engaging clients and driving managers determine key areas for active treatment to target • Ad hoc support for work • Using a registry to prioritize planning and training flow course corrections • Develop or fine-tune and manage a caseload • Working with primary care screening and treatment workflows partners • Orientation for providers • Emphasis on practice and and staff to team roles active learning • Assistance in choosing a registry
Phase 1 and Phase 2 Announcements • Save the Date! – All Day In-Person Training on May 7, 2019 – Olympia, WA FOUNDATIONAL CONCEPTS FOR – CEU Available INTEGRATINIG PRIMARY CARE IN • Monthly Webinar Series BEHAVIORAL HEALTH SETTINGS – Third Tuesday of the Month, 10-11am • Site Planning Calls – To schedule starting February – Frequency & length of calls flexible, monthly to start – For operations & clinical leadership New York Times Article: May 2018 Learning Objectives By the end of this webinar, teams will: • Identify key health conditions that impact people with serious mental illness and/or substance use disorders • Understand how to adopt core principles of bi-directional integration and apply to their setting https://www.nytimes.com/2018/05/30/upshot/mental-illness-health-disparity-longevity.html
Background: Life Expectancy in SMI My Sudden Introduction to the Short and NOT Improving p g Mortality Gap • Hard to pursue recovery goals when dead • No one else is doing it • Opportunity for frequent touches • Now part of our mission Bar 1 & 2: Druss BG, Zhao L, Von Esenwein S, Morrato EH, Marcus SC. Understanding excess mortality in persons with mental illness: 17-year follow up of a nationally representative US survey. Med Care. 2011 June;49(6):599-604 Bar 3: Daumit GL, Anthony CB, Ford DE, Fahey M, Skinner EA, Lehman AF, Hwang W, Steinwachs DM. Pattern of mortality in a sample of Maryland residents with severe mental illness. Psychiatry Res. 2010 Apr 30;176(2-3):242-5 Most Premature Mortality Due to Prevalence of Current Smoking Cardiovascular Disease (CVD) • Life expectancy 15 years shorter • CVD accounts for 60% of premature deaths among persons with SMI • Every CVD risk factor is more than twice as common Dickerson F, et.al,. Psychiatr Serv 2013; 64 (1): 44
Impact of Antipsychotic Medications What Can Reduce CVD Risk? Estimated Weight Change at 10 Weeks on “Standard” Dose • Meta-analysis for AHRQ: 33 RCTs from 1980-2012 1 • 28 studies addressed weight 6 13.2 Weight Change (kg) 5 11.0 • One weight loss study of Schizophrenia and Diabetes 2 Weight Change (lb) † 4 8.8 • 3 6.6 Comprehensive review for NIMH3 (80 of 108 studies 2 4.4 related to obesity) * 1 2.2 • Strong evidence for use of four interventions 0 0 • -2.2 -1 Metformin for obesity -4.4 -2 • Lifestyle modification for obesity -6.6 -3 • Bupropion for tobacco cessation • Varenicline for tobacco cessation * 4–6 week pooled data (Marder SR et al. Schizophr Res. 2003;1;61:123-36; † 6-week data adapted from 1 Gierisch JM, et al. J Clin Psychiatry. 2014 May;75(5):e424-40. ; 2 McKibbin CL, et.al. Schizophr Allison DB,Mentore JL, Heo M, et al. Am J Psychiatry. 1999;156:1686-1696; Jones AM et al. ACNP; 1999. Res. 2006 Sep;86(1-3):36-44.; 3 McGinty EE et al. Schizophr Bull. 2016 Jan;42(1):96-124. Small Changes Big Difference First Steps Towards Planning a Response • Team-based • Data-driven 5% �� in cardiovascular 10% �� in cardiovascular Triglycerides disease disease Cholesterol � 10 mm/L • How do you do it? � 10% ������ in cardiovascular ������ in diabetes related disease deaths Blood HbA1c 42% �� in stroke ������ in heart attacks Pressure � 1 pt � 6mm/Hg ������ in microvascular complications
Missouri CMHC Healthcare Homes Outcomes Improving uncontrolled A1c 10.2 10 10 9.8 Missouri CMHC � 1.48 points For individuals with A1c > 9.0 9.6 at initial test result Healthcare Homes 9.4 N = 909 9.2 First Result: 10 Year 5 | 2016 8.9 Last Result: 8.9 9 8.8 8.6 8.4 8.2 First Result Last Result Regional MHC 2015: Moving From ‘At-risk’ To ‘No Longer At-Risk’ Over the first 4 years, CMHC Healthcare Homes produced a net savings of $98 million! 100% 90% $ 80% 70% 60% 50% Cost Savings savings in millions 40% (2012-2015) 30% At-risk at Baseline 20% 10% Current per member per Outcome Improved month (PMPM) rate for 0% No Longer At-risk CMHC Health Homes is $85.23 (Jan 2016)
Measurement-Based Care Principles for Evidence-Based Integration Team-Based and Person-Centered Primary care and behavioral health providers collaborate effectively, using shared care plans. “Involves the systematic use of symptom rating scales to drive Population-Based and Data-Driven clinical decision making.” A defined group of patients or clients is tracked in a registry so that no one “falls through the cracks.” Measurement-Based Treatment to Target Treatment goals clearly defined and tracked for every patient. Treatments actively changed until clinical goals are achieved . https://chp-wp- uploads.s3.amazonaws.com/www.thekennedyforum.org/uploads/2017/06/KennedyForum- MeasurementBasedCare_2.pdf Integration of Care in Behavioral Health What is a Registry and How to Use It? Needs Someone to Drive the Registry: Nurse Care Manager / Registry Function Psychiatrist and /or Case Manager PCP consultant Mental Health Center Psychiatrist and /or Case Manager PCP Partner Behavioral Health Agency Patien Pat Pat Patient ien ie ent Patient PCP PCP Primary Care Primary Care
Addressing Physical Health Examples of Care Management Staff in Pediatric Populations • Multiple staff can perform these functions with • Weight gain is severe and rapid in antipsychotic- different strengths/weaknesses naïve patients treated not only with olanzapine – Behavioral health case managers but also with quetiapine, risperidone, and • Used to coordinating care, interfacing with the outside world • aripiprazole 1 Less medical background – Nurses • Child psychiatrists 2 • More medical background • Sometimes less comfort with SMI population – Over 95% aware of all guidelines • More expensive! – Over 80% agreed with most guidelines – Peers • – Less than 20% had adopted and adhered to most The benefit of lived experience • Less medical background guidelines 1 JAMA. 2009;302(16):1765–1773. ; 2 Psychiatr Serv. 2017 Sep 1;68(9):958-961. Training Website Action Items • Find webinar recordings, training resources & calendar 1. Schedule team meetings • Share your best practice documents, workflows, or and calls with AIMS Center presentations! 2. Complete Project • “None of us is as smart as all of us” Description Worksheet – Overall Project AIM – Target Population – Measures 3. Email to Juliann (salisj2@uw.edu) by Friday, 2/15/19 4. Be prepared to share by Tuesday, 2/19/19 https://aims.uw.edu/wastate/content/whole-person-care-training-program
Webinar Series Overview 1. Foundational • Attend webinar, "Foundational Concepts for Integration in a Behavioral Health Setting" Concepts for Integration • Project Description submitted before next webinar • Attend webinar, "Team Roles and Readiness for Integrating Care" and share 2. Team Roles and Readiness for final Project Description THANK YOU! Integrating Care • AIMS Task List submitted before next webinar • Attend webinar, "Develop Your Clinical Workflow for Integrated Care" and 3. Develop Your share team roles Clinical Workflow • Drafted workflow for screening or treatment of your target population for Integrated Care submitted before next webinar 4. Population • Attend webinar, "Population Management - Using a Registry to Track Management - Outcomes" and share workflow development Using a Registry to • Finalize workflow and registry strategy Track Outcomes
Recommend
More recommend