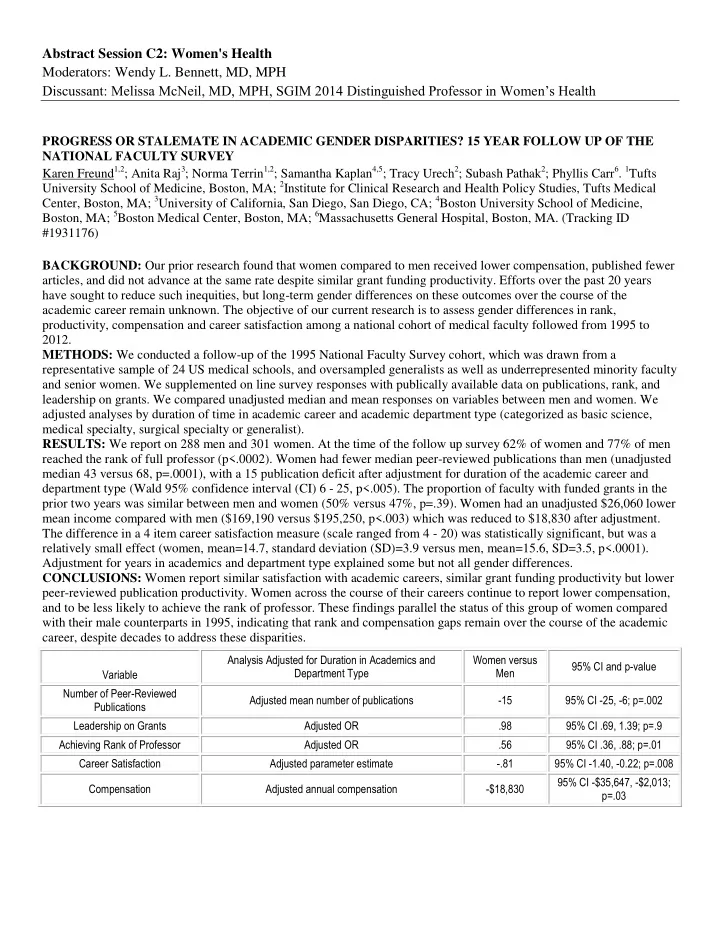
Abstract Session C2: Women's Health Moderators: Wendy L. Bennett, MD, MPH Discussant: Melissa McNeil, MD, MPH, SGIM 2014 Distinguished Professor in Women’s Health PROGRESS OR STALEMATE IN ACADEMIC GENDER DISPARITIES? 15 YEAR FOLLOW UP OF THE NATIONAL FACULTY SURVEY Karen Freund 1,2 ; Anita Raj 3 ; Norma Terrin 1,2 ; Samantha Kaplan 4,5 ; Tracy Urech 2 ; Subash Pathak 2 ; Phyllis Carr 6 . 1 Tufts University School of Medicine, Boston, MA; 2 Institute for Clinical Research and Health Policy Studies, Tufts Medical Center, Boston, MA; 3 University of California, San Diego, San Diego, CA; 4 Boston University School of Medicine, Boston, MA; 5 Boston Medical Center, Boston, MA; 6 Massachusetts General Hospital, Boston, MA. (Tracking ID #1931176) BACKGROUND: Our prior research found that women compared to men received lower compensation, published fewer articles, and did not advance at the same rate despite similar grant funding productivity. Efforts over the past 20 years have sought to reduce such inequities, but long-term gender differences on these outcomes over the course of the academic career remain unknown. The objective of our current research is to assess gender differences in rank, productivity, compensation and career satisfaction among a national cohort of medical faculty followed from 1995 to 2012. METHODS: We conducted a follow-up of the 1995 National Faculty Survey cohort, which was drawn from a representative sample of 24 US medical schools, and oversampled generalists as well as underrepresented minority faculty and senior women. We supplemented on line survey responses with publically available data on publications, rank, and leadership on grants. We compared unadjusted median and mean responses on variables between men and women. We adjusted analyses by duration of time in academic career and academic department type (categorized as basic science, medical specialty, surgical specialty or generalist). RESULTS: We report on 288 men and 301 women. At the time of the follow up survey 62% of women and 77% of men reached the rank of full professor (p<.0002). Women had fewer median peer-reviewed publications than men (unadjusted median 43 versus 68, p=.0001), with a 15 publication deficit after adjustment for duration of the academic career and department type (Wald 95% confidence interval (CI) 6 - 25, p<.005). The proportion of faculty with funded grants in the prior two years was similar between men and women (50% versus 47%, p=.39). Women had an unadjusted $26,060 lower mean income compared with men ($169,190 versus $195,250, p<.003) which was reduced to $18,830 after adjustment. The difference in a 4 item career satisfaction measure (scale ranged from 4 - 20) was statistically significant, but was a relatively small effect (women, mean=14.7, standard deviation (SD)=3.9 versus men, mean=15.6, SD=3.5, p<.0001). Adjustment for years in academics and department type explained some but not all gender differences. CONCLUSIONS: Women report similar satisfaction with academic careers, similar grant funding productivity but lower peer-reviewed publication productivity. Women across the course of their careers continue to report lower compensation, and to be less likely to achieve the rank of professor. These findings parallel the status of this group of women compared with their male counterparts in 1995, indicating that rank and compensation gaps remain over the course of the academic career, despite decades to address these disparities. Analysis Adjusted for Duration in Academics and Women versus 95% CI and p-value Department Type Men Variable Number of Peer-Reviewed Adjusted mean number of publications -15 95% CI -25, -6; p=.002 Publications Leadership on Grants Adjusted OR .98 95% CI .69, 1.39; p=.9 Achieving Rank of Professor Adjusted OR .56 95% CI .36, .88; p=.01 Career Satisfaction Adjusted parameter estimate -.81 95% CI -1.40, -0.22; p=.008 95% CI -$35,647, -$2,013; Compensation Adjusted annual compensation -$18,830 p=.03
PHYSICIAN VISITS AND SURVEILLANCE TESTING AMONG BREAST CANCER SURVIVORS IN TAIWAN Yong A. Wang 1,2 ; An-Chen Feng 2 ; Patricia Ganz 1 . 1 UCLA Jonsson Comprehensive Cancer Center, Los Angeles, CA; 2 Koo Foundation Sun Yat-Sen Cancer Center, Taipei, Taiwan. (Tracking ID #1933474) BACKGROUND: The resource demands from the expanding cancer survivor population pose a significant challenge to health care systems worldwide. Guidelines recommend regular history, physical examination and mammography, but against routine surveillance imaging for detecting distant metastasis in survivors of breast cancer treated with curative intent. Studies of health services utilization of cancer survivors in Asia are limited. We examined patterns of physician visits and surveillance testing in a major cancer center in Taiwan, and assessed their relationship to various patient and physician factors and trends over time. METHODS: All stage 0, I, II breast cancer cases were identified from the Taiwan Cancer Registry that were treated in the cancer center during 2002 to 2009. After excluding cases with recurrence, cases and institutional claims data were merged to measure the number of outpatient visits, breast imaging, and surveillance tests for detecting metastatic recurrence including serum tumor markers, abdominal imaging, chest X-ray, bone scan and PET, during the disease-free follow-up period from 13 to 60 months after initiation of breast cancer treatment. Poisson regression and logistic regression analyses were used to examine factors contributing to physician visits and testing, and separate analyses were conducted to look at individual patient cohorts from years 2002 to 2008 where sufficient follow up was available. RESULTS: A total of 3,488 women ages 19 to 88 were identified from the registry. The number of breast cancer-specific physician visits in the 48-month follow up period (mean 18.7 per patient, SD 8.5) and the rates of surveillance testing to detect distant metastasis were greater than those recommended by ASCO/NCCN guidelines. Variables predicting the number of physician visits included age, cancer stage, year of treatment, hormonal therapy, chemotherapy, radiotherapy, whether the patient had seen psychiatry or medical subspecialties other than oncology, and the primary physician/specialty following the patient for breast cancer. After adjusting for covariates, the number of visits was highest among patients primarily followed by medical oncologists and lowest among those followed by breast surgeons (Figure 1). The adjusted 48-month visit rates decreased progressively from the 2003 cohort (mean 22.7) to the 2008 cohort (mean 17.7), related to an institutional effort in care coordination for breast cancer survivors. There was a significant decrease in the adjusted rate of tumor marker testing from the 2002 cohort (99.7%) to the 2008 cohort (38.0%) associated with the change in the institutional guideline (Figure 2). Greater number of visits was correlated with more frequent testing. Patients primarily followed by medical oncologists had the highest adjusted testing rates for tumor markers, bone scan, and abdominal imaging. CONCLUSIONS: Early stage breast cancer survivors in Taiwan had high utilization of physician visits and surveillance testing for distant metastasis. This might be improved by greater coordination of care among breast cancer specialists. Implementation of an evidence-based guideline regarding the number of visits, imaging and tumor marker testing may be necessary to reduce the overutilization of testing.
Recommend
More recommend