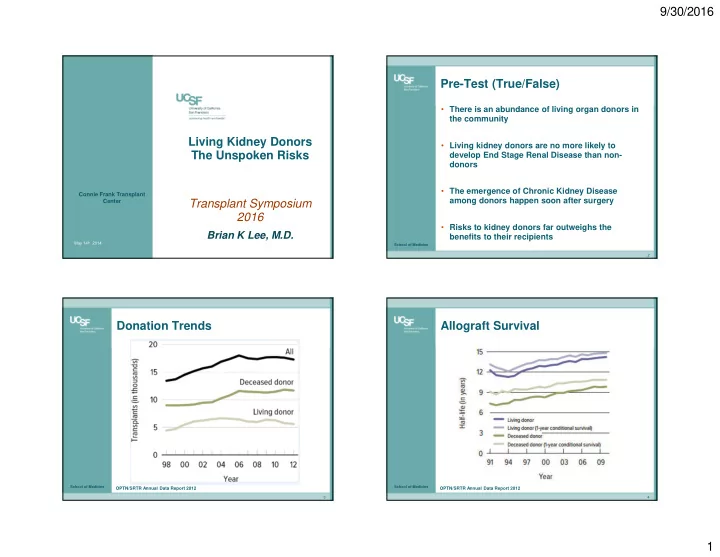
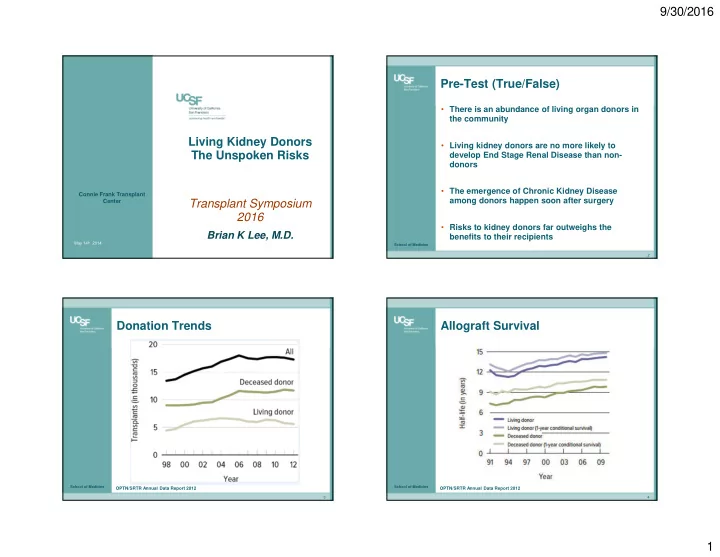
9/30/2016 Pre-Test (True/False) • There is an abundance of living organ donors in the community Living Kidney Donors • Living kidney donors are no more likely to The Unspoken Risks develop End Stage Renal Disease than non- donors • The emergence of Chronic Kidney Disease Connie Frank Transplant Transplant Symposium among donors happen soon after surgery Center 2016 • Risks to kidney donors far outweighs the Brian K Lee, M.D. benefits to their recipients May 14 th 2014 School of Medicine 2 Donation Trends Allograft Survival School of Medicine School of Medicine OPTN/SRTR Annual Data Report 2012 OPTN/SRTR Annual Data Report 2012 3 4 1
9/30/2016 Once Apron A Time….. Health of Donor…. • “ The health of the donor dominates all other considerations. A major operation on a normal person, not for his own benefit, requires a brusque re-evaluation of traditional surgical thought….moral justification is found in the safety and security of the donor as well as in the expected degree of success when there is no other alternative.” School of Medicine School of Medicine Murray et al. Ann Surg 1958; 148:343-59 5 6 Uninephrectomy in Childhood The State of Affairs Pre-2013 • 111/224 eligible candidates evaluated • FU range 7-52 yrs • Inulin and PAH clearances done • Solitary kidney regained 75-80% GFR expected of two kidneys Donor Survival • ERPF was ↑ 30% in single kidney • 23% had microalbuminuria, of whom 6 had excretion ≥ 250mg/day School of Medicine School of Medicine Baudoin et al. AJKD 1993; 21:603-11 7 8 2
9/30/2016 Donor vs. Gen Pop Survival Data Country Setting N= Years FU (yrs) Origin studied Sweden Single 430 1964-1994 1-35 center Sweden Japan Japan Single 481 1970-2006 1-35 center France Single 310 1952-2008 1-53 center USA Single 3698 1963-2007 1-45 center USA France School of Medicine School of Medicine 9 10 Donor vs. Selected “Healthy” Population Donor vs. Selected “Healthy” Population • 80K + live kidney donors in US, 1994-2009 • Comparison group – selected cohort from NHANES III ‘88-’94 • Median FU period 6.3 yrs School of Medicine School of Medicine Segev et al. JAMA 2010; 303:959-66 Garg et al. BMJ 2012; 344:e1023 11 12 3
9/30/2016 ESRD in Donor Population The State of Affairs Pre-2013 Kidney Dysfunction • 1112 consecutive donors in Sweden • Median time from donation to ESRD 20 yrs (14-27) • Of the 6 with ESRD, 4 reported from nephrosclerosis, only single case was verified • Based on advanced age of donors at time of ESRD, rates were comparable to general population School of Medicine School of Medicine Fehrman-Ekholm et al. Transplantation 1996; 82:1646-48 13 14 Effect on GFR – Pooled Analysis A Landmark Paper ….. School of Medicine School of Medicine Garg et al. KI 2006; 70:1801-10 15 16 4
9/30/2016 Causes of ESRD in Donors 4 3 • 3698 Kidney donors – ’63 through ‘07 @ U Minn 2 • Cohort of 255 donors also had iohexol GFR and albuminuria measured 1 • Patient survival of donors compared to life 0 tables from Human Mortality Database • Rates of ESRD in general population estimated to be 268 cases/million person-yrs (USRDS 2007 annual report) ESRD Rate 180/ million person-yrs • NHANES 2003-4 and 2005-6 cohorts were Female 7/11 matched by age, sex, ethnicity, and BMI to Caucasian 8/11 donors in whom GFR was measured Siblings 7/11 (all ESRD cases were LRRT) School of Medicine School of Medicine Ibrahim et al. NEJM 2009; 360:459-69 17 18 School of Medicine School of Medicine 19 20 5
9/30/2016 Limitations • 99% donors were Caucasian • Increasing acceptance of older donors, those with HTN, obesity • Relied on patient contact/recall for diagnosis of ESRD • Control group gleaned from general population, vs. highly selected donor cohort School of Medicine School of Medicine 21 22 School of Medicine School of Medicine 23 24 6
9/30/2016 All Cause Mortality School of Medicine School of Medicine Mjoen et al. KI 2014. 86:162-7. 25 26 All-Cause and CV Mortality ESRD Risk in Donors • Absolute risk of ESRD – 9/1901 donors = 0.47% • Median time to ESRD 18.7 yrs • 7/9 cases of ESRD was caused by immunologic disease – hereditary component (most were close relatives) • Crude incidence - 302/million person-yrs amongst donors vs. 100/milion person-yrs in Norway population School of Medicine School of Medicine 27 28 7
9/30/2016 Limitations • 100% donors were Caucasian of Scandivian ancestry • Most donors were relatives of recipients, not • 96,217 donors from 1994-2011 necessarily generalizable to LURT / non- directed donations • 2/3 of live donors were biologically related to recipient • Donors were selected from throughout Norway, • Repeated matched done with 9364 non-donors, drawn from the while controls belonged to single county NHANES ‘88-’94 cohort, who had no contraindications to donation exceptionally low mortality rates • ESRD defined as initiation of dialysis (CMS 2728), wait-listing for • Differing eras (donors 1963-2007) while controls kidney transplant, or receipt of Ktx 1984-87, with general mortality having improved between ‘63 and ’84 • Baseline characteristics were similar, but noted 22% of donors had eGFR < 80 cc/min • Longer FU amongst controls may have affected mortality and ESRD rates School of Medicine School of Medicine Muzaale et al. JAMA 2014; 311: 579-86 29 30 Stratified by Ethnicity Cumulative ESRD incidence School of Medicine School of Medicine 31 32 8
9/30/2016 Absolute Risk Increases Life-time Risk of ESRD Donor Non-Donor ∆ AR (per 10,000) (per 10,000) (per 10,000) All 30.8 3.9 26.9 AA 74.7 23.9 50.8 Hispanics 32.6 6.7 25.9 Caucasian 22.7 0 22.7 School of Medicine School of Medicine Limitations Focus on Absolute Risks • Differing cohorts (donors 1994-2011, controls drawn from ‘88-94) – recent increased ESRD incidence • Underestimation of ESRD risk in controls % donors with ESRD a) Long event free survival repeatedly sampled Mjoen et al. 0.47% b) Different competing risks of death • Increased surveillance for ESRD amongst donors Muzaale et al. 0.1% • Prioritization of previous donors to the waitlist for transplantation (so long as eGFR < 20cc/min) • Crude vs.15 yr cumulative incidence of ESRD Muzaale et al. 15 yr risk % Lifetime Risk % Incidence Donors Non-Donors (per 10,000) (per 10,000) Donors 0.0031 0.009 Healthy Controls 0.0004 0.0014 Crude 10.3 18.2 General Pop N/A 0.033 15 yr cumulative 30.8 3.7 School of Medicine School of Medicine 9
9/30/2016 The BottomLine … • Mjoen et al. “Most potential living donors are willing to accept a degree of risk when the recipient is a family member or a close friend. Our findings will not change our opinion in promoting live-kidney Informing Consent donation.” • Muzaale et al. “.. the magnitude of the absolute increase is small. These findings may help inform discussions with persons considering live kidney donation.” School of Medicine School of Medicine 37 38 Framing Risk Discussion School of Medicine School of Medicine Turin et al. 2012; 23:1569-78 39 40 10
9/30/2016 Counseling of Living Donors – Framing Risk Discussion Changing Paradigm ? School of Medicine School of Medicine Turin et al. 2012; 23:1569-78 Steiner et al. AJT 2014; 14: 538-44 41 42 Non-maleficence Autonomy • Primum non nocere • “ How do the risks and benefits of donation compare to those of not donating? ” • Loss of a loved one • Care-giver burden • Disability, loss of household income, childcare/family support (non-health benefits) • Labeling of potential donor as “unfit” � disappointment and guilt School of Medicine School of Medicine 43 44 11
9/30/2016 OPTN Policy 12 – Living Donation School of Medicine School of Medicine Allen et al. AJT 2014; 14: 531-37 45 46 Normal GFR vs Age and Gender Summary • Donors have to accept that risks are ever- changing as more information/data becomes available • Information/education presented in a comprehensible manner is crucial in defining this risk • Absolute risk values may be more representative • Caution towards close relatives of living donor recipients (e.g. SLE, primary glomerular dz etc.) • Awareness on professionals part that there are also “harms” to refusing a donor School of Medicine School of Medicine Wetzels et al. KI 2007; 72: 632-37 47 48 12
9/30/2016 Future Directives Post-Test (True/False) • Establishing prospective databases to assess • There is an abundance of living organ donors in impact of reduced renal mass on mortality/GFR the community in the long term • Building a comparable cohort of “healthy” non- • Living kidney donors are no more likely to donors (e.g. siblings of donors with similar develop End Stage Renal Disease than non- health status) donors • Eliminating barriers to longitudinal donor followup (advent of tele-medicine, reimbursing • The emergence of Chronic Kidney Disease donors for local lab testing) among donors happen soon after surgery • Identifying risk alleles in evaluation/selection of potential donors (MYH9, APOL1 etc.) • Risks to kidney donors far outweighs the benefits to their recipients School of Medicine School of Medicine 49 50 School of Medicine 51 13
Recommend
More recommend