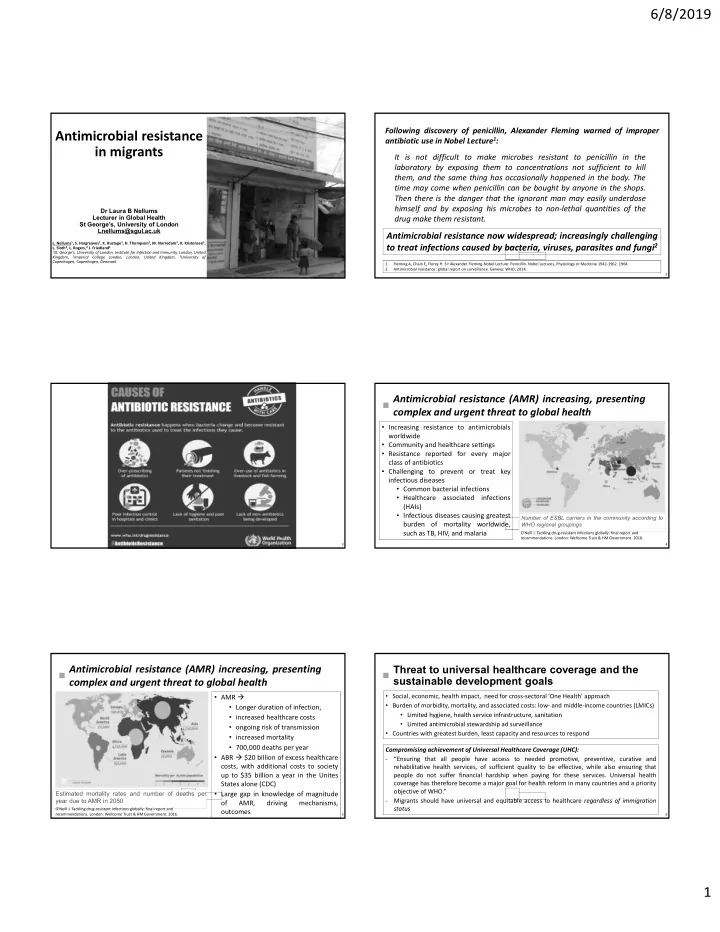
6/8/2019 Following discovery of penicillin, Alexander Fleming warned of improper Antimicrobial resistance antibiotic use in Nobel Lecture 1 : in migrants It is not difficult to make microbes resistant to penicillin in the laboratory by exposing them to concentrations not sufficient to kill them, and the same thing has occasionally happened in the body. The time may come when penicillin can be bought by anyone in the shops. Then there is the danger that the ignorant man may easily underdose himself and by exposing his microbes to non‐lethal quantities of the Dr Laura B Nellums Lecturer in Global Health drug make them resistant. St George’s, University of London Lnellums@sgul.ac.uk Antimicrobial resistance now widespread; increasingly challenging L. Nellums 1 , S. Hargreaves 1 , K. Rustage 1 , H. Thompson 2 , M. Norredam 3 , K. Kristensen 3 , to treat infections caused by bacteria, viruses, parasites and fungi 2 L. Sloth 3 , L. Rogers, 2 J. Friedland 1 1 St. George's, University of London, Institute for Infection and Immunity, London, United Kingdom, 2 Imperial College London, London, United Kingdom, 3 University of Copenhagen, Copenhagen, Denmark 1. Fleming A, Chain E, Florey H. Sir Alexander Fleming‐Nobel Lecture: Penicillin. Nobel Lectures, Physiology or Medicine 1942‐1962. 1964. 2. Antimicrobial resistance: global report on surveillance. Geneva: WHO; 2014. 1 2 Antimicrobial resistance (AMR) increasing, presenting complex and urgent threat to global health • Increasing resistance to antimicrobials worldwide • Community and healthcare settings • Resistance reported for every major class of antibiotics • Challenging to prevent or treat key infectious diseases • Common bacterial infections • Healthcare associated infections (HAIs) • Infectious diseases causing greatest Number of ESBL carriers in the community according to burden of mortality worldwide, WHO regional groupings such as TB, HIV, and malaria O'Neill J. Tackling drug‐resistant infections globally: final report and recommendations. London: Wellcome Trust & HM Government. 2016. 3 4 Threat to universal healthcare coverage and the Antimicrobial resistance (AMR) increasing, presenting sustainable development goals complex and urgent threat to global health • AMR • Social, economic, health impact, need for cross‐sectoral ‘One Health’ approach • Burden of morbidity, mortality, and associated costs: low‐ and middle‐income countries (LMICs) • Longer duration of infection, • Limited hygiene, health service infrastructure, sanitation • increased healthcare costs • Limited antimicrobial stewardship ad surveillance • ongoing risk of transmission • Countries with greatest burden, least capacity and resources to respond • increased mortality • 700,000 deaths per year Compromising achievement of Universal Healthcare Coverage (UHC): • ABR $20 billion of excess healthcare ‐ “Ensuring that all people have access to needed promotive, preventive, curative and costs, with additional costs to society rehabilitative health services, of sufficient quality to be effective, while also ensuring that up to $35 billion a year in the Unites people do not suffer financial hardship when paying for these services. Universal health States alone (CDC) coverage has therefore become a major goal for health reform in many countries and a priority objective of WHO.” Estimated mortality rates and number of deaths per • Large gap in knowledge of magnitude year due to AMR in 2050 ‐ Migrants should have universal and equitable access to healthcare regardless of immigration of AMR, driving mechanisms, status O'Neill J. Tackling drug‐resistant infections globally: final report and outcomes recommendations. London: Wellcome Trust & HM Government. 2016. 5 6 1
6/8/2019 Globalisation and AMR Global Action Plan on AMR • Travel, tourism, migration, inter-hospital transfer, movement of animals or agricultural products • Research focus predominantly on travellers and patients returning from hospitals abroad 2015: WHO endorsed global action plan to tackle AMR • Concern migration contributing to global spread of AMR limited evidence Five key pillars of action 1 1) improving awareness and understanding of antimicrobial resistance through effective communication, education and training; 2) strengthening the knowledge and evidence base through surveillance and research; 3) reducing the incidence of infection through effective sanitation, hygiene, and infection prevention measures; 4) optimizing the use of antimicrobial medicines in human and animal health; and 5) developing the economic case for sustainable investment taking into account the needs of all countries, and increasing investment in new medicines, diagnostic tools, vaccines, and other interventions 1. Global action plan on antimicrobial resistance. Geneva: WHO; 2015. World Health Organization; 2017. 7 Holmes et al. Understanding the mechanisms and drivers of antimicrobial resistance. The Lancet, 2016. 8 Global migration Previous focus on infectious diseases in migrants predominantly in HIV and Unprecedented rates of migration TB • 244m migrants worldwide; 65.3m forced Migrants experience burden of TB in high‐ migrants – refugees, asylum seekers, or IDPs worldwide income countries • 73.4% of MDR‐TB cases in EU and EEA • 1 in 113 people on the planet displaced • Over 2m forced migrants to Europe since 2015; member states in foreign‐born Highest rates since records began • Evidence of MDR‐TB being imported as • 61.4% have health problems during journey; 93% well as acquired or transmitted in host of those with health issue on arrival had symptom countries onset during migration; Median travel time: 100 days • AMR risk factors: High-incidence country, social inequalities/living conditions (e,g. camps, detention centres), cost of healthcare/Rx, barriers to care, disrupted health systems, poor quality Rx 9 10 Limited evidence on relationship between migration and Concerns increasing MDR‐TB drug‐resistance attributed to poor treatment adherence Increasing AMR; migration contributing to burden in host countries? Not known whether migrants experience high rates of AMR or where acquired Systematic review and meta‐analysis Higher due to increased incidence in countries of origin, poor social conditions, on MDR‐TB treatment adherence in barriers to care? migrants: Lower due to more limited access/exposure to antibiotics or healthcare facilities? • Migrant adherence to MDR‐TB Limited surveillance/data collection treatment regimens is approaching global treatment targets (71% vs 75%) • Migrant adherence and non‐adherence to MDR‐TB treatment regimens is comparable to non‐migrant populations 11 12 2
6/8/2019 Systematic review and Results meta-analysis 23 observational studies reporting on Preferred Reporting Items for Systematic Reviews and Meta- Analysis (PRISMA) guidelines antibiotic resistance in 2319 migrants Databases: MEDLINE, Embase, PubMed, Scopus Pooled prevalence of any AMR Primary data (2000-2017) on carriage or infection in migrants carriage or infection: 25.4% (95% CI: 19.1 – 31.8) (foreign-born) from observational studies reporting antibacterial resistance in common bacterial pathogens Meticillin‐resistant Migrants to EU/EEA Staphylococcus aureus (MRSA) (7.8%, 4.8–10.7) Data extraction and quality assessment using piloted • Antibiotic resistant Gram‐negative standardised forms bacteria (27.2%, 17.6–36.8) Random effects models to calculate pooled prevalence PROSPERO CRD42016043681 13 14 Systematic review and meta-analysis Elevated rates among refugees and asylum seekers 33.0% (95% CI: 18.3 – 47.6) compared to ‘other’ migrants (6.8%; 95% CI: 2.1 – 11.5) High prevalence in high migrant community settings 33.1% (95% CI: 11.1 – 55.1) compared to 24.4% (95% CI: 16.2 – 32.6) in hospital settings Migrants overrepresented among community acquired MRSA 62.7% (95% CI: 50.2 – 75.3) PVL positive MRSA isolates (marker for CA-MRSA). Evidence antibiotic resistant organisms being acquired during migration trajectory in transit or host countries limited evidence of onward transmission 15 MDRO screening: asylum seekers admitted to university hospital or presenting to emergency department • 273 patients • Carriage rate of 31% ‐ E.coli most common Duration of MDRO carriage in asylum seekers Duration of MDROs in asylum seekers in the Netherlands • Screening and clinical samples from asylum seekers in the Netherlands; Rates of MRSA and MDRE detected calculated every four weeks after arrival • 2091 asylum seekers • No decline in MDROs in first obtained sample was observed after arrival in Netherlands • Carriage rate of MDRO in asylum seekers remains high even after prolonged stay 18 3
Recommend
More recommend