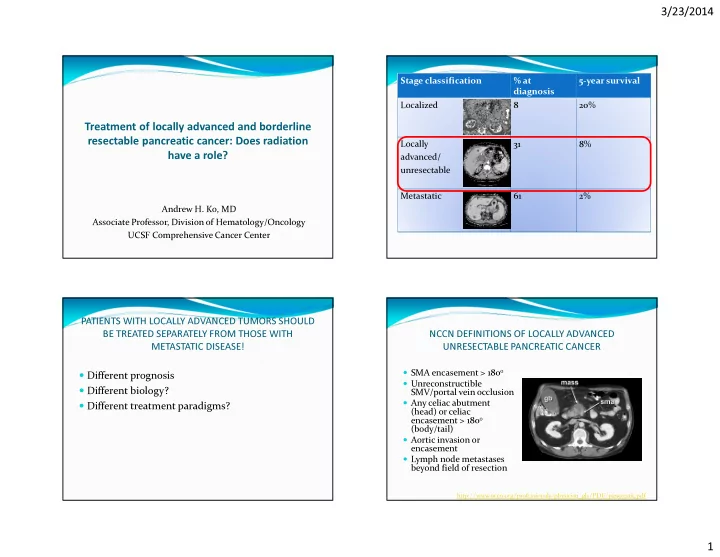
3/23/2014 Stage classification % at 5-year survival diagnosis Localized 8 20% Treatment of locally advanced and borderline resectable pancreatic cancer: Does radiation Locally 31 8% have a role? advanced/ unresectable Metastatic 61 2% Andrew H. Ko, MD Associate Professor, Division of Hematology/Oncology UCSF Comprehensive Cancer Center PATIENTS WITH LOCALLY ADVANCED TUMORS SHOULD BE TREATED SEPARATELY FROM THOSE WITH NCCN DEFINITIONS OF LOCALLY ADVANCED METASTATIC DISEASE! UNRESECTABLE PANCREATIC CANCER � SMA encasement > 180 o � Different prognosis � Unreconstructible � Different biology? SMV/portal vein occlusion � Any celiac abutment � Different treatment paradigms? (head) or celiac encasement > 180 o (body/tail) � Aortic invasion or encasement � Lymph node metastases beyond field of resection http://www.nccn.org/professionals/physician_gls/PDF/pancreatic.pdf 1
3/23/2014 THE SEQUENCING OF CHEMOTHERAPY AND RADIATION: LOCALLY ADVANCED PANCREATIC CANCER: UNRESOLVED QUESTIONS DOES IT MAKE A DIFFERENCE? WHAT WE KNOW WHAT WE STILL DON’T KNOW Start with radiation? Start with chemotherapy? ChemoRT is superior to RT alone - Is radiation absolutely necessary? (GITSG 1981) � Importance of obtaining � Greatest imperative is to - If so, when should it be given? Outcomes are different from those with - Most studies to date have optimal local control eradicate micrometastatic metastatic disease – should be studied examined initial chemoRT, with disease � Better symptom palliation in separate clinical trials, or stratified very mixed results (pain, bowel obstruction) � Select out patients who within a given study (multiple phase III - There may be a better rationale trials; Philip, J Clin Oncol for delaying radiation until later develop metastases during � Better likelihood of 2009;27:5660-9) initial chemotherapy (~ 25- cytoreduction to downstage a - How often are ‘borderline’ 30%), avoid morbidities unresectable patients successfully patient for potential surgery converted to being able to undergo assoc. with RT successful surgery? EARLY TRIALS OF LOCALLY ADVANCED COMPARISON OF MODERN RANDOMIZED STUDIES PANCREATIC CANCER IN LOCALLY ADVANCED PDAC Take home Study n Results FFCD/SFRO message? ChemoRT (6 weeks) Gemcitabine RT alone (6000 cGy): Concurrent cisplatin/5-FU � Locally median surv = 23 weeks advanced GITSG ChemoRT is superior RT (4000 cGy) + bolus 5-FU: � 194 disease (n=119) Chemotherapy median surv = 42 weeks Continue to RT alone 1981 gemcitabine � RT (6000 cGy) + bolus 5-FU: (gemcitabine) median surv = 40 weeks � 5-FU/RT (4000 cGy) followed by (ChemoRT followed GITSG SMF: median surv = 42 weeks ECOG 4201 43 by chemo) is superior ChemoRT (6 weeks) Gemcitabine SMF alone (streptozocin/MMC/5- 1988 � Gemcitabine to chemotherapy FU): median surv = 32 weeks Locally Concurrent gemcitabine x 5 cycles x 5 cycles (600 mg/m2 weekly) advanced (ChemoRT followed 5-FU/RT (4000 cGy) followed by � disease ECOG 5-FU: median survival = 8.3 mos by chemo) is Gemcitabine 91 Gemcitabine 5-FU alone: median surv = 8.2 (n=74) � equivalent to Gemcitabine (6 weeks) 1985 Gemcitabine (6 weeks) mos x 5 cycles x 5 cycles chemotherapy Chauffert et al. Ann Oncol 2008; Loehrer et al, J Clin Oncol 2011. 2
3/23/2014 COMPARING FFCD-SFRO vs. ECOG 4201 INDUCTION CHEMOTHERAPY SELECTS OUT PATIENTS WHO ARE NOT APPROPRIATE CANDIDATES FOR CHEMORADIATION FFCD/SFRO ECOG Cisplatin/5-FU + 6000 Gemcitabine + 5040 cGy LAD PDAC STUDIES WHERE INDUCTION CHEMOTHERAPY WAS GIVEN Induction regimen cGy RT (6 weeks) RT (6 weeks) n Induction regimen % NOT going on to receive Maintenance Gemcitabine until chemoRT 2o to disease Gemcitabine x 5 cycles chemotherapy progression progression/toxicity/other 11.0 vs. 9.2 months, in Ko (UCSF) 25 Gem/cisplatin 32% Median OS compared 8.6 vs. 13.9 months, in favor of induction Crane (MD 69 GemOx + cetuximab 13% to chemo alone favor of chemo alone chemoRT Anderson) Moureau-Zabotto 59 GemOx 15% 1-year survival 32% vs. 53% 50% vs. 32% (GERCOR) Kim (Korea) 37 Gem/cisplatin 19% 114 � Did ECOG study use a more effective radiosensitizing regimen? Mukherjeee Gem/capecitabine 35% � Was the induction regimen prescribed by FFCD/SFRO overly intensive � (SCALOP) delayed administration and total amount of subsequent systemic therapy? Huguet (GERCOR, 181 Gem-based 29% retrospective) � Further exploration of delayed chemoradiation is required RETROSPECTIVE ANALYSIS OF LOCALLY ADVANCED DISEASE IN GERCOR STUDIES Median PFS 10.8 vs. 7.4 mos (p=0.005) Median OS 15.0 vs. 11.7 mos (p=0.0009) Huguet, F. et al. J Clin Oncol; 25:326-331 2007 Huguet, F. et al. J Clin Oncol; 25:326-331 2007 3
3/23/2014 International phase III LAP-07 study (Hammel, J Clin Oncol 2013 (suppl; abstr LBA 4003) LAP-07 RESULTS � Original n=722 � interim analysis after 442 patients SECOND RANDOMIZATION allowed enough events to reach futility boundary FIRST MEDIAN OS 16.4 mos RANDOMIZATION � Results: Gemcitabine x 2 Stop until MEDIAN PFS 11.8 mos months progression Gemcitabine x 4 months After 4 months: 136 chemo alone RT (5400 cGy) + Stop until capecitabine progression Induction 269 randomized 442 enrolled, chemotherapy received induction Gemcitabine plus Erlotinib until erlotinib x 2 chemotherapy 133 chemoRT progression months Gemcitabine plus (gemcitabine +/- 173 dropped out erlotinib x 4 erlotinib) (mainly due to months MEDIAN OS 15.2 mos RT (5400 cGy) + Erlotinib until progressive dz) MEDIAN PFS 12.5 mos capecitabine progression � Secondary analysis: addition of erlotinib to gemcitabine Primary question: Does chemoradiation after induction chemotherapy improve conferred NO benefit (gem alone, 13.6 months; overall survival? (looking for HR 0.75 � increase from 9 to 12 mos) gem/erlotinib: 11.9 months) Secondary question: Does adding erlotinib to gemcitabine help? RTOG 1201 : Proposed study design IMPLICATIONS/UNRESOLVED ISSUES OF STUDY Locally advanced PDAC � Do we conclude on this basis that radiation Stratify: should not be routinely given to patients SMAD4 Status with locally advanced pancreatic cancer? � Do more effective systemic therapies, such as FOLFIRINOX, Gemcitabine/nab- and gemcitabine/Abraxane, attenuate any survival benefit paclitaxel that radiation might offer? x 3 months � Conversely, does the superior and more durable systemic disease control expected with FOLFIRINOX attach even greater importance to achieving local control with RT? � Does radiation impact local recurrence rate? What about IMRT + Continue 3D-CRT + cape QoL? cape gemcitabine/ 50.4 Gy � Do we have any biomarkers that can guide us on patterns of 63 Gy nab-paclitaxel recurrence? (SMAD4) 4
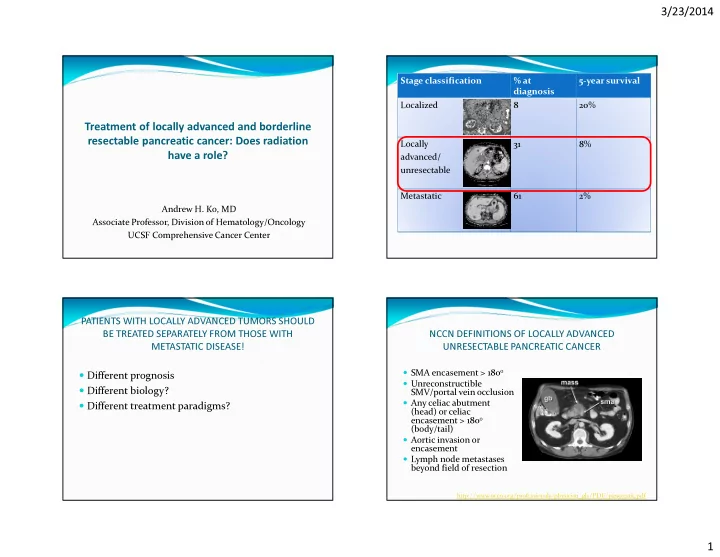
3/23/2014 SMAD4 (DPC4) AS A PREDICTIVE BIOMARKER Stage classification Stage classification % at % at 5-year survival 5-year survival Results of Hopkins rapid-autopsy series diagnosis diagnosis Localized Localized 8 8 20% 20% Locally destructive/ Extensive metastatic oligometastatic # of 0 1-10 11-99 100s-1,000s BORDERLINE ? ? Locally 31 8% metatstases RESECTABLE advanced/ DPC4 loss 22% 45% 71% 73% Locally 31 8% unresectable (2/9) (5/11) (14/24) (16/22) advanced/ 35% (7/20) 72% (33/46) unresectable Metastatic 61 2% Metastatic 61 2% Could DPC4 expression be used to guide treatment decisions re: radiation? Iacobuzio-Donahue, J Clin Oncol 2009; 27: 1806–1813. AHPBA/SSAT/SSO DEFINITION OF DISTINGUISHING BETWEEN LOCALLY ADVANCED vs. BORDERLINE RESECTABLE PANCREATIC CANCER “BORDERLINE RESECTABILITY” VESSEL Tumor involvement Superior mesenteric SMV Abutment, encasement, occlusion vein – portal vein SMV SMV SMA T SMA Superior mesenteric T Abutment T SMA artery Common hepatic Abutment artery Short-segment encasement R0 likely R0 impossible Resectable “Borderline” Unresectable Curative Palliative Celiac trunk No abutment or encasement Chance of R0 resection can be predicted on basis of relationship between the tumor and mesenteric vasculature 5
3/23/2014 Alliance A021101: TREATMENT SCHEMA N = 20 (primarily feasibility study) R 50.4g R R E FOLFIRINOX SURGERY F E EBRT E E GEM N O Borderline S + CAPE S S R 4 cycles L resectable T T T 2 x 28 O + 6 – 8 L disease A + 4 – 10 A A day L weeks O G weeks G G cycle L + 2 - 6 weeks break W E break E E break Is radiation necessary to successfully downstage? EFFICACY RESULTS OF CONTEMPORARY STEREOTACTIC BODY RADIOTHERAPY (e.g. Cyberknife) CHEMOTHERAPY REGIMENS � Alternative to conventionally fractionated XRT? FOLFIRINOX Gemcitabine � More intensified treatment in a single (25 Gy) or small # of fractions (5-6.5 Gy x 5) ORR 31.6% 9.4% � Greater convenience Median PFS 6.4 months 3.3 months � Treat tumor + small margin only; limited nodal coverage Median survival 11.1 months 6.7 months � Sharper dose fall-off gradients to normal tissue 1 year survival 48.4% 20.6% � Early studies raised concern re: late/chronic toxicity, e.g. DT Chang, Cancer 2009, 115:665-72. ulceration/mucositis of stomach and duodenum 6
Recommend
More recommend