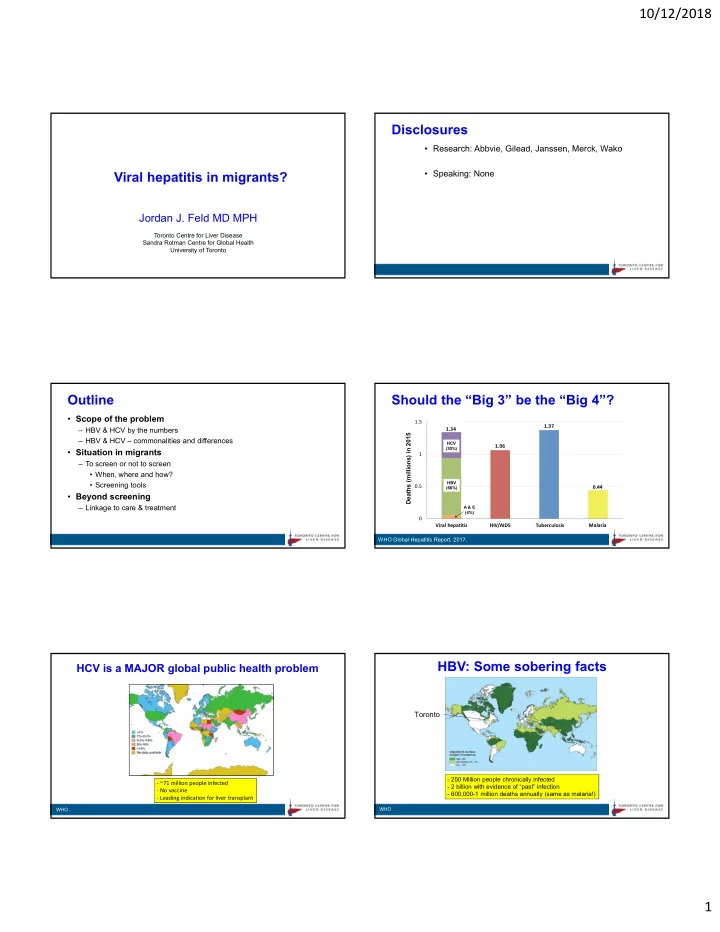
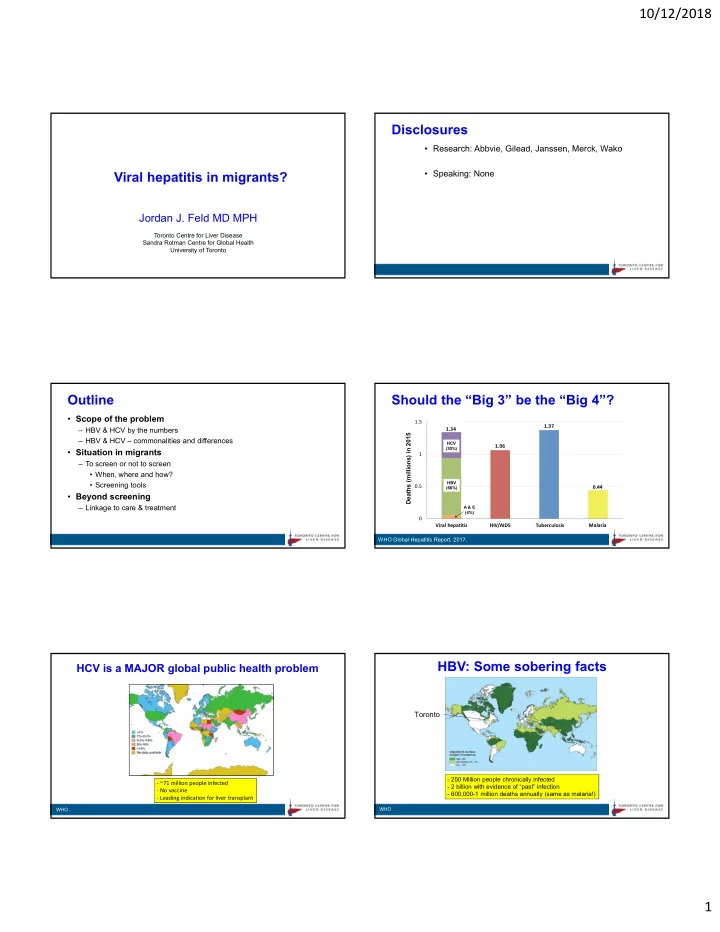
10/12/2018 Disclosures • Research: Abbvie, Gilead, Janssen, Merck, Wako • Speaking: None Viral hepatitis in migrants? Jordan J. Feld MD MPH Toronto Centre for Liver Disease Sandra Rotman Centre for Global Health University of Toronto Outline Should the “Big 3” be the “Big 4”? • Scope of the problem 1.5 1.37 – HBV & HCV by the numbers 1.34 Deaths (millions) in 2015 – HBV & HCV – commonalities and differences HCV 1.06 (30%) • Situation in migrants 1 – To screen or not to screen • When, where and how? • Screening tools HBV 0.5 0.44 (66%) • Beyond screening – Linkage to care & treatment A & E (4%) 0 Viral hepatitis HIV/AIDS Tuberculosis Malaria WHO Global Hepatitis Report, 2017. HBV: Some sobering facts HCV is a MAJOR global public health problem Toronto - 250 Million people chronically infected ‐ ~71 million people infected - 2 billion with evidence of “past” infection ‐ No vaccine - 600,000-1 million deaths annually (same as malaria!) ‐ Leading indication for liver transplant WHO WHO 1
10/12/2018 Dramatic improvement in HCV therapy Hepatitis is a MAJOR health problem in Canada DAAs 2014 PR + NI Hepatitis C virus 2013 95-99% PR + PI 100% Streptococcal pneumonia Peginterferon 90% Sustained Virological Response 2011 Human papilloma virus Hepatitis B virus Ribavirin 2002 E. Coli Standard 80% 75% HIV/AIDS 2001 Staphylococcus aureus Interferon Influenza 1998 ie. Cure 55% C. Dificile 60% Rhinovirus 1995 Respiratory syncytial virus 42% 39% Parainfluenza virus 1991 34% Group B Strep Years of Life Lost 40% Group A Strep Year-equivalents of reduced functioning Haemophilus influenza 16% Tuberculosis Legionella 20% Chlamydia 6% Adenovirus Gonorrhea 0% 0 2000 4000 6000 8000 1000 IFN IFN IFN/R IFN/R PegIFN PegIFN/R PR/PI PR/SOF DAAs 6-12 mo 3 mo 3 mo 6 mo 12 mo 6 mo 12 mo 12 mo 12 mo Health Adjusted Life Years (HALYs) Kwong PLoS One 2012 The first cancer vaccine – highly effective! WHO takes the lead Trend in 3 rd dose of vaccine coverage in Vision: “ A world where viral hepatitis transmission is halted and everyone infants global coverage living with viral hepatitis has access to safe, affordable and effective prevention, care and treatment services ” Global coverage 79% in 2012 Western Pacific HBsAg Positivity (%) Americas Americas 2004 European 1984 1989 No vaccine Vaccine<5 yo Africa Africa Eastern Eastern 1999 1994 Mediterranean Mediterranean SE Asia SE Asia Age (years) • Eliminate viral hepatitis as a public health problem • Increasing but plateauing global coverage 79% in 2012 and 82% in 2014 • Although called ‘Elimination’ – given the targets…maybe this is really ‘Control’ • Only 38% coverage of birth‐dose (reduces risk by 8‐fold) • Whatever we call it ‐ very ambitious! WHO, Ni Gastro 2007, WHO 2017 WHO Global Health Sector Strategy 2016‐2021 WHO Elimination Targets WHO Elimination Targets WHO WHO 2
10/12/2018 The cascade of care…not just treatment Treatment uptake more important than cure rate Modeled data for non-VA US population • Curing the individual is now easy • Curing the population will take a lot more work… SVR in individuals SVR in the population Diagnosis Access Treated SVR But won’t this all get better with IFN-free therapy? Improved therapy of no benefit unless treatment rates increase Thomas Nat Medicine 2010 Yehia PLoS One 2014 An elimination strategy Why are treatment rates so low? Reminder in EPR 92,012 visits 16,772 (18%) tested 715 Ab + (4.2%) Patients • Unaware of infection feel perfectly well until advanced disease • May have little interaction with the healthcare system Left side of 68% • Screening and active case finding required the cascade DAAs only help here Percentage 80% actually more Doctors important 90% • Poor awareness – late diagnosis and referral 57% (46% 90% RNA+) • Treatment capacity – few hepatologists, GIs, IDs – PCPs/addiction medicine…just starting to enter the field – Outdated models of care – based on the interferon days • Treatment access often limited – fibrosis stage, specialists Anti‐HCV RNA RNA Initiated Completed Achieved • Improved access, increased provider base and new models of Positive Tested Positive Treatment Treatment SVR N=715 N=488 N=388 N=223 N=201 N=180 care required Even with effective treatment, major gaps in cascade of care! Mera MMWR 2016 What about HBV? Highly effective therapy • Current therapy taken long-term Long‐term entecavir in eAg +ve HBV Tenofovir vs Tenofvir/emtricitabine in LAM‐R HBV – Suppresses HBV DNA – Normalizes ALT % suppressed HBV DNA % suppressed HBV DNA – Prevents fibrosis progression – Promotes fibrosis regression – even in cirrhosis – Prevents and even reverses hepatic decompensation – Reduces, but does not eliminate, the risk of HCC Highly effective BUT not curative Long‐term therapy with potent oral nucleos(t)ide analogues leads to suppression in almost all patients (even after resistance) Lim Gastro 2014, Papaetheodoridis J Hep 2015, Zoutendijk Gut 2013, Marcelllin Chang Hepatology 2010, Fung J Hep 2017 Lancet 2013, Chang Hepatology 2010 3
10/12/2018 HBsAg loss is the real goal of therapy HBV ≠ HCV: Some key differences • Transmission – HBV: At birth, (sexual) - HCV: Throughout life – medical, IDU 30% • Epidemiology HBsAg Loss after 1 year of therapy – Some overlap but some key differences 20% – HBV: Asia, SS Africa - HCV: S. Asia, Egypt, Eastern Europe • Natural History 10% – HBV: Dynamic, unpredictable - HCV: Slowly progressive 7% • Treatment 3% ~1% 1.1% 1.7% 1% – HBV: Complicated decisions, long-term/indefinite specialty care 0% PegIFN Lamivudine Adefovir Entecavir Tenofovir Placebo – HCV: Simple, finite, curative primary care Implication : Once you start…usually very long-term therapy! Summary data from multiple trials – not head‐to‐head Outline Benefits of screening for viral hepatitis • Scope of the problem Individual – HBV & HCV by the numbers • Access to treatment – prevent complications of – HBV & HCV – commonalities and differences the disease • Situation in migrants • Prevent additional harms to health – alcohol, – To screen or not to screen obesity (even if no treatment) • When, where and how? • Vaccination for HBV – personal & contacts • Screening tools Societal • Beyond screening • Harm reduction – reduce transmission – linkage to care & treatment • Assess burden in the population – plan for the future Screening Approaches Potential ‘harms’ of screening Risk-based Population-based Individual • Diagnosis in asymptomatic individuals Identify and test only those with Test a segment of the population risk factors eg. baby boomers, newcomers – Give a well person a ‘disease’ – Potentially stigmatizing – may affect employment, immigration Pros: Pros: • Potentially ‘harmful’ unless High yield High coverage rate – Linkage to care – minimum – information, harm reduction Cheaper Easy to implement – Access to treatment – this is really the key • Very frustrating to be told: Cons: Cons: • ‘No treatment available’, ‘No doctors available’ or ‘You’re not sick enough for treatment’ or ‘No treatment for you unless you stop using drugs/EtOH’ Contact with HC system Need to choose the population Societal Must know & discuss risk factors Low yield, expensive • Cost of screening Test may be stigmatized May be stigmatizing to population – • Cost of treatment cost effective is not cost saving – huge eg. migrants Miss those without RFs budget impact…opportunity cost! Not mutually exclusive 4
Recommend
More recommend