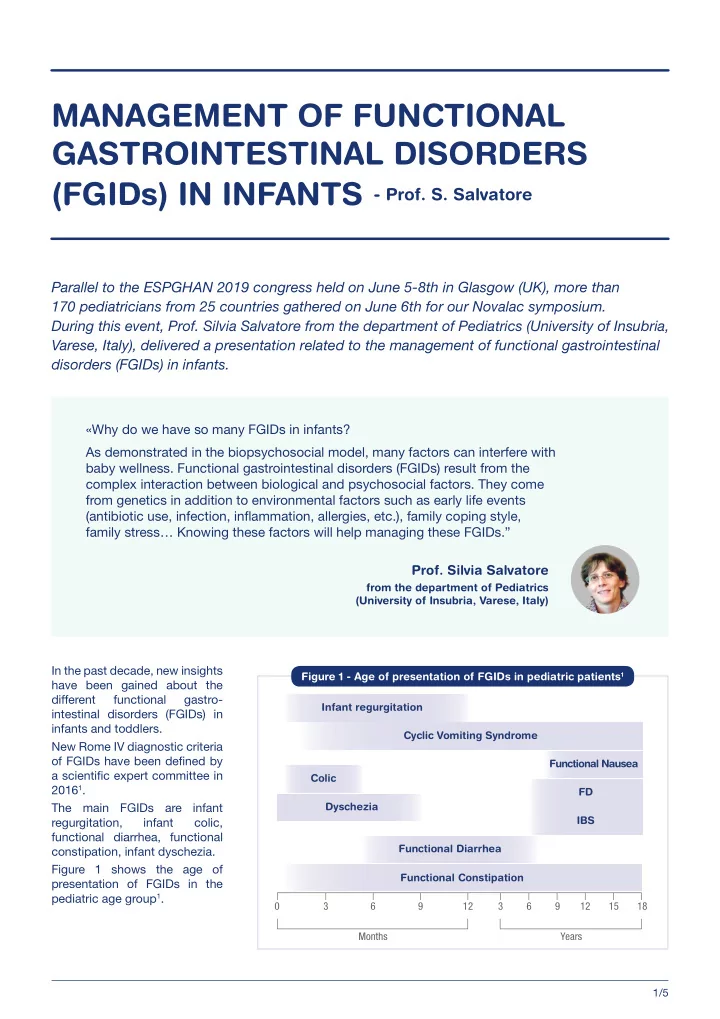
MANAGEMENT OF FUNCTIONAL GASTROINTESTINAL DISORDERS (FGIDs) IN INFANTS - Prof. S. Salvatore Parallel to the ESPGHAN 2019 congress held on June 5-8th in Glasgow (UK), more than 170 pediatricians from 25 countries gathered on June 6th for our Novalac symposium. During this event, Prof. Silvia Salvatore from the department of Pediatrics (University of Insubria, Varese, Italy), delivered a presentation related to the management of functional gastrointestinal disorders (FGIDs) in infants. «Why do we have so many FGIDs in infants? As demonstrated in the biopsychosocial model, many factors can interfere with baby wellness. Functional gastrointestinal disorders (FGIDs) result from the complex interaction between biological and psychosocial factors. They come from genetics in addition to environmental factors such as early life events (antibiotic use, infection, infmammation, allergies, etc.), family coping style, family stress… Knowing these factors will help managing these FGIDs.” Prof. Silvia Salvatore from the department of Pediatrics (University of Insubria, Varese, Italy) In the past decade, new insights Figure 1 - Age of presentation of FGIDs in pediatric patients 1 have been gained about the different functional gastro Infant regurgitation intestinal disorders (FGIDs) in infants and toddlers. Cyclic Vomiting Syndrome New Rome IV diagnostic criteria of FGIDs have been defjned by Functional Nausea a scientifjc expert committee in Colic 2016 1 . FD Dyschezia The main FGIDs are infant IBS regurgitation, infant colic, functional diarrhea, functional Functional Diarrhea constipation, infant dyschezia. Figure 1 shows the age of Functional Constipation presentation of FGIDs in the pediatric age group 1 . 0 3 6 9 12 3 6 9 12 15 18 Months Years 1/5
About 30-50% of infants present with symptoms of 2.1 Breast milk for FGIDs: the best FGIDs during the fjrst 12 months of life. functional and personalized food These FGID symptoms can have important Breastfeeding should be recommended and consequences on the families and the society . supported, even when infants display persistent and They vary from mild to extremely distressing for the severe FGIDs. Breast milk is a perfect orchestra for infant and parents and may lead to a cascade of infant micro/macro nutrients and for immune properties discomfort and crying, parental anxiety, poor quality (Figure 2). of life, short and longterm health consequences, shortened duration of full breastfeeding, frequent formula changes and medical consultations, overuse Figure 2 - Protective effects of drugs and high associated healthcare costs 2–9 . of breastfeeding 10 FGIDs result from complex interactions between biological, psychological, and social factors . Passive immunity Scientifjc and medical experts have developed and by the IgA antibodies discussed practical recommendations and algorithms to manage FGIDs 4,7 . The most relevant recommen • Protection against infections • Reduce risk of CD dations for the pragmatic management of FGIDs can be summarized as follows: • Observe : the infant, the parents and the meal. Regulation of • Educate and reassurance : provide information on gut permeability natural history of FGIDs, infant growth and feeding. • Reduce of gastrointestinal infections • Avoid : overload, smoking, tests, drugs. • Prevent of tissue transglutaminase expression 1 OBSERVATION FOR ANY ALARM SIGNS Bioactive antimicrobial factors The fjrst step in the management of FGIDs is to • Maturation of gut make sure the symptoms are functional. Thus, any • Development of the infant’s innate abnormal signs should be excluded when reviewing and acquired immunities the history of symptoms and onset of FGIDs, when evaluating the meal, parents’ interaction, performed tests, when assessing growth and development, and Exerted of immuneregulatory during physical examination. • Via suppression of 2 EDUCATION ON FGIDs autoimmunogenic Tcell Parental education and reassurance is recom mended as the fjrst line of management of FGIDs 7 : Antimicrobial and anti-inflammatory agents • Nutritional advice should emphasize the benefjts of breastfeeding and appropriate support should • Blocking of the infmammatory be offered whenever necessary. Parents should be cytokines production by lactoferrin • Protection against infections via aware that breastfeeding provides the most ideal oligosaccharides nutrition for infants. • Overfeeding infants may exacerbate their symptoms and should be avoided. 2.2 Special milk formulas in FGIDs, • Colic and regurgitation are temporary problems for whom? during the fjrst months of life and then sponta neously decrease and resolve in most infants within IIn nonbreastfed infants, special milk formulas may be the fjrst year. considered in case of FGIDs. Each infant is unique, but each infant formula is • Pharmacological approaches are not necessary unique, too. Thus, infant formula that shows clinical for infantile colic and regurgitation and could harm benefjts should be chosen . Special milk formulas are infants. Gastric acid inhibitors such as proton specifjc for infants with a particular gastrointestinal pump inhibitors (PPI) or prokinetic drugs have been symptom. Key nutrients in special milk formula include shown to have side effects, such as an increased protein, fat, carbohydrates, prebiotics and probiotics, rate of infection, and are mostly ineffective for these and have different properties of interest for specifjc conditions. Drug treatment is exceptionally used in situations. case of functional constipation. Management of functional gastrointestinal disorders (FGIDs) in infants Prof. S. Salvatore 06/2019 2/5
The role of proteins in the management Thickened formulas for infants of FGIDs with regurgitation The nature of proteins (casein or whey) and their Studies in infants with persistent regurgitation degree of hydrolysis (native, partial or extensive) will and poor weight gain have shown that thickened differently impact gastric emptying. Whey proteins are formulas signifjcantly reduce by half the number emptied faster than caseins, thus those last ones are of regurgitation episodes , increase the number of better to improve satiety. infants without regurgitation and increase weight gain compared to standard formulas 16 . Commonly used • Partial hydrolyzed formula (pHF) for FGIDs? thickening agents include carob/locust bean gum, Some studies show no benefjt of pHF on FGIDs corn starch and rice starch. whereas others show benefjts on colic, regurgitation and sometimes stool consistency. However, tested A commercial thickened formula has the advantage formulas differed not only by the nature of the to be homogeneous, to have a nutritionally balanced proteins but also by other components (GOS/FOS, composition, and a higher viscosity in the stomach, lactose content, etc.). Based on these confmicting but it is more expensive and there might be a risk results, no recommendation can be made on the of over use. In contrast, a “home-brew” thickened use of pHF for FGID management. formula is cheaper and easy to prepare, but there is a higher sucking effort for the infant, a delayed gastric • Extensively hydrolyzed formula (eHF) for FGIDs? emptying, an inconsistency in composition and it has For a faster gastric emptying, eHF should be a too high viscosity and many calories. selected. eHF will also treat 90 to 95% of infants For some babies with persistent symptoms or having CMA and reduce lactose related symptoms. regurgitating while breastfed, the thickening agent However, there are some disadvantages regarding alginate has been recently shown to signifjcantly the use of eHF in case of FGIDs: different eHFs decrease the number and extension of both acid and exist on the market, there are limited data on the nonacid refmux episodes and associated symptoms in longterm outcomes, eHFs can also infmuence taste infants with suspected GERdisease 17 . development, and the cost of these formulas is not negligible. • How to differentiate FGIDs from cow’s milk How to manage infant colic? allergy (CMA)? Infant colic results from normal developmental process. The diagnosis of CMA and its distinction from It is described as a behavioral syndrome in infants FGIDs is quite challenging since their age is over younger than 5 months old involving long periods of lapping, they do not have specifjc symptoms, CMA crying and hardtosoothe behavior 1 . is frequently nonIgE mediated, and a possible Parental reassurance is used as the fjrst line of association and confounding response may management of infant colic1. There is no evidence that exist 11–14 . pharmacologic intervention are useful. Some studies The Cow’s Milk-related Symptom Score suggest that particular probiotic supplements are (CoMiSS) , which considers general manifestations, effective for breastfed infants with colic but there are dermatological, gastrointestinal and respiratory insuffjcient data to make conclusions for formulafed symptoms, was developed as an awareness tool infants with colic 18 . for cow’s milkrelated symptoms 15 . Symptomatic children who score 12 or higher on the CoMiSS score with the presence of at least three symptoms and the involvement of two organ systems, are considered at a high risk of CMA. But the CoMiSS awareness tool is not a diagnostic test for CMA. It does not replace a food challenge with a cow’s milkfree diet. Management of functional gastrointestinal disorders (FGIDs) in infants Prof. S. Salvatore 06/2019 3/5
Recommend
More recommend