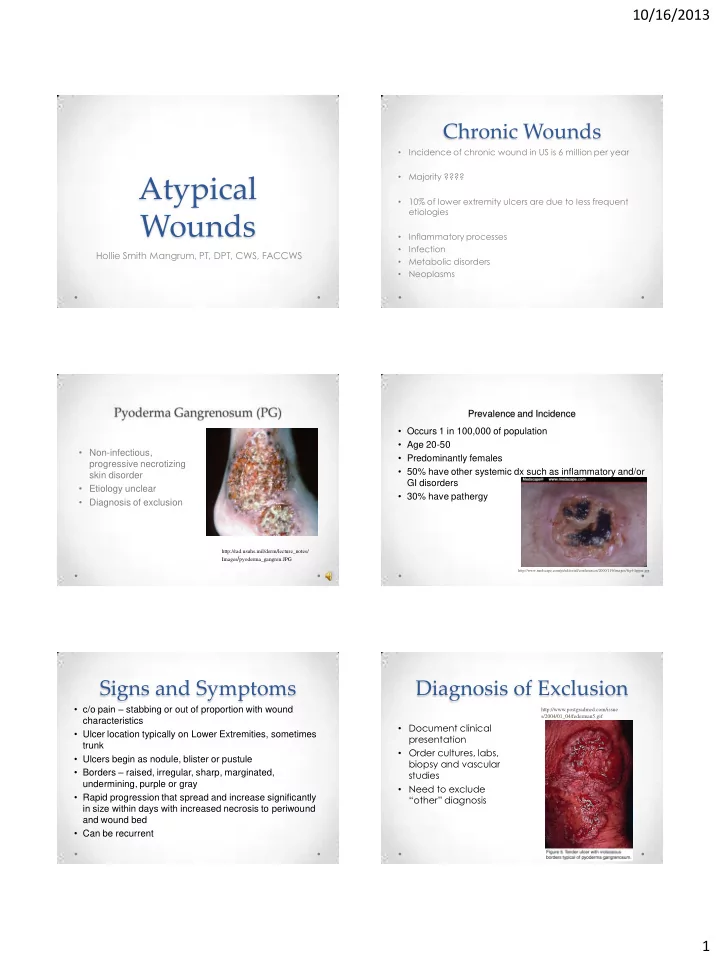
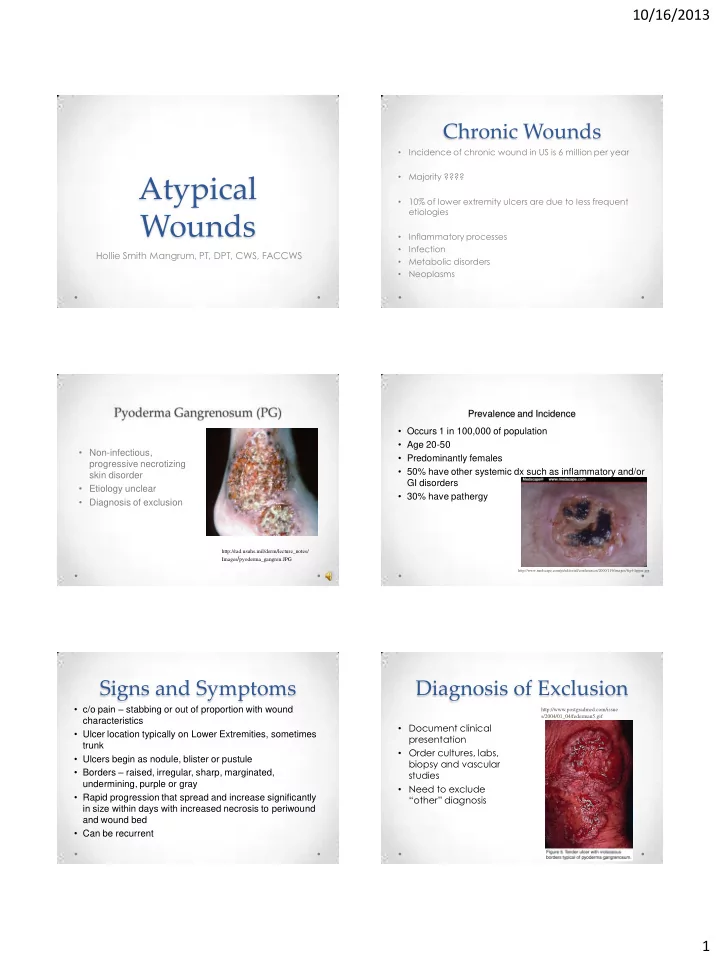
10/16/2013 Chronic Wounds Incidence of chronic wound in US is 6 million per year • Majority ???? • Atypical 10% of lower extremity ulcers are due to less frequent • etiologies Wounds Inflammatory processes • Infection • Hollie Smith Mangrum, PT, DPT, CWS, FACCWS Metabolic disorders • • Neoplasms Prevalence and Incidence • Occurs 1 in 100,000 of population • Age 20-50 • Non-infectious, • Predominantly females progressive necrotizing • 50% have other systemic dx such as inflammatory and/or skin disorder GI disorders • Etiology unclear • 30% have pathergy • Diagnosis of exclusion http://rad.usuhs.mil/derm/lecture_notes/ Images / pyoderma_gangren.JPG http://www.medscape.com/pi/editorial/conferences/2000/119/images/fig4-lipper.jpg Signs and Symptoms Diagnosis of Exclusion • c/o pain – stabbing or out of proportion with wound http://www.postgradmed.com/issue s/2004/01_04/federman5.gif characteristics • Document clinical • Ulcer location typically on Lower Extremities, sometimes presentation trunk • Order cultures, labs, • Ulcers begin as nodule, blister or pustule biopsy and vascular • Borders – raised, irregular, sharp, marginated, studies undermining, purple or gray • Need to exclude • Rapid progression that spread and increase significantly “other” diagnosis in size within days with increased necrosis to periwound and wound bed • Can be recurrent 1
10/16/2013 Differential Diagnoses Treatment Recommendations • 1-2 mg/dg/day prednisone • Venous Leg Ulcer • Pulsed IV 1g/day for 3-5 days if rapid treatment needed • Vasculitis • Low dose cyclosporin 3-5 mg/kg/day as primary or adjunct if • Trauma corticosteroids fail • Drug reactions • Dapsone as maintenance therapy with or without prednisone • Moisture retentive dressings for pain control, induce collagen • Bites production, facilitate autolytic debridement and promote • Non-healing burn angiogenesis • Irrigation for bacterial and fungal growth • Topical Triamcinilone Cream (TAC) to wound and borders twice weekly • Surgical or sharps debridement contraindicated 8 Case Study Initial Visit • (May) – 9 full thickness wounds with purple or lavender borders, • 58 yo African American female with recurrent ulcers to bilateral lower moderate slough, minimal granulation, good extremity pulses, extremities complaints of pain (burning, stinging, tingling) • Recent treatment in Wound Center 2 years prior to this admission for venous insufficiency • Initial Dx - DWLE Grade 1 with underlying venous disease and possible Pyoderma Gangrenosum • 7 year Hx of Diabetes • • Hx of recurrent ulcers to lower extremities Work Up: • labs for infection, inflammation, nutritional status, baseline kidney • HTN and liver function • Ultrasounds to rule out arterial and venous disease – no insurance • Asthma • Cultures of wounds • Recent cough • Biopsy of wound • Denied ulcerative colitis, Crohn’s disease, Inflammatory bowel related • Treatment – Selective sharps debridement and dressed with disease cadexamer iodine and light compression to be changed two times weekly . Follow Up Visit Progressive Plan of Care • Biopsy showed acute neutrophilic inflammation with necrosis and ulceration consistent with Pyoderma Gangrenosum • Over the course of 6 months: • Cultures – 3+ acinetobacter, 3+ strep, 3+ corynebacterium treated with augmentin • Labs – elevated glucose, low prealbumin, elevated ESR • Several antimicrobial dressings including silver, • No change in wounds except two new wounds cadexamer iodine, antibiotic ointment, methylene blue and gentian violet • POC – Dx changed to PG • Monthly cultures requiring several rounds of antibiotics • Weekly MD for selective debridement including for MRSA • Nursing 2-3 x weekly for dressing changes 2
10/16/2013 Progressive Plan of Care Progressive Plan of Care • Fourth month: • For first three months: • Developed rash – discontinued current antibiotics, • Wounds would improve then deteriorate initiated topical silver and ordered Benadryl • Patient had negative reactions to some topical • Next week – 3 wounds had healed agents 13 Progressive Plan of Care Progressive Plan of Care • Fifth month: • Sixth month: • Steadily healed 2-3 more wounds each week • Initiated Triamcinilone Cream (TAC) in November to • Zyvox initiated in October for MRSA wounds • Dec 2 – all wounds completely healed • Approved for Indigent Care by treating facililty • Referred again for ultrasounds to check arterial and • Referred to Infectious Disease – initiated 10mg venous insufficiency – negative for both Prednisone TID Outcome Hydradenitis Suppurativa • Considered a severe form of acne occurring deep • PG effectively suspected, excluded and included around the sebaceous glands and hair follicles • Likely misdiagnosed two years prior • Chronic skin inflammation with blackheads and/or • Did not treat with steroids initially bumps/lesions that break open and drain pus • Due to pain, irritation and rash, dressings sometimes changed • Groin and armpits where apocrine sweat glands weekly to something different making tracking progress difficult are located • Wound began to improve prior to steroid initiation • • Generally appears after puberty Selective debridement contraindicated for PG • Lack of insurance was an obstacle • Outcome ultimately achieved healing but could wounds have been healed quicker???? • http://www.mayoclinic.com/health/ hidradenitis-suppurativa/DS00818 3
10/16/2013 Prevalence and Incidence Risk Factors • 1-2% of general population • Obesity • All races but increased in African Americans • Smoking • Seen greater in hot, humid environments • Family history of acne • More women than men • Apocrine duct obstruction • Men – greater in anogenital region • Secondary bacterial infection • Females - greater in axilla • Hirsutism • Onset anytime between puberty and post • Chemical irritants – deoderants or antiperspirants menopause – ages 11-50 • Mechanical irritants – shaving or depilatory use Signs and Symptoms Signs and Symptoms • Early: • Papules or nodules o Itching • Abscesses o Erythema • Late: • Inflamed o Excessive localized • Erythema o Lesions perspiration o Pain • Purulent o Purulence • Dermal contractures o Disfigurement and ropelike elevation of the skin • Double-ended (bridged) comedones Diagnosis Differential Diagnosis • Clinical findings • Associated • Mimics Characteristic lesions lesions comorbidities: o o Folliculitis Typical distribution of lesions o Furunculosis o Crohn’s Disease o o Recurrence – remissions of long periods may delay diagnosis Pilonidal cysts o Irritable Bowel o • Must have one of the following: Actinomycosis o o Certain Arthritis One active primary lesion and history of 3 or more discharging and painful o o Catscratch disease Down Syndrome o lesions since puberty Graves Disease o Inactive disease (no current lesion) but history of 5 or more painful and o draining abscesses since puberty • Labs CBC with diff, ESR, CRP, CMP, Urinalysis, consider thyroid and anemia o workup • Cultures Ensures appropriate antibiotics o o Usually grow staph and/or strep 4
10/16/2013 Treatments Treatments (continued) • Local hygiene – soaps without dyes and perfumes • Corticosteriod injections into around lesions • Weight reduction • NSAIDS to manage pain • Warm compresses • I&D if large and fluctuant or painful nodules • Loose fitting clothes • Radical surgery (aggressive approach) but very effective if late stages – must remove the entire • Absorptive Antimicrobial and/or charcoal dressings affected and scarred area for odor • NPWT and/or skin grafting if surgical option chosen • Oral Antibiotics – to reduce inflammation – abx used for acne (erythromycin, tetracycline, • Specialist Referrals – Infectious Disease, Plastic minocycline, doxycycline) Surgeon, Surgeon, Immunologist • HBO – not CMS or UHMS approved Resources: www.familydoctor.org; www.hs-usa.org; www.aafp.org • Vasculitis Prevalence/Incidence • Autoimmune disease causing inflammatory changes in • Men > Women blood vessels leading occlusion causing poor lumen integrity,bleeding, ischemia and necrosis • Onset ages 65-74 yo Rare, chronic and relapsing disease • Can affect large and small vessels • http://www.dermnet.com/moduleSearch.php • Risk Factors Signs and Symptoms • Autoimmune disorders • Deep, punched out ulcers o RA • Red, purple or blue wound edges SLE o • Painful Sjogren’s Syndrome o • Rapid deterioration • Purpuric rash 5
Recommend
More recommend