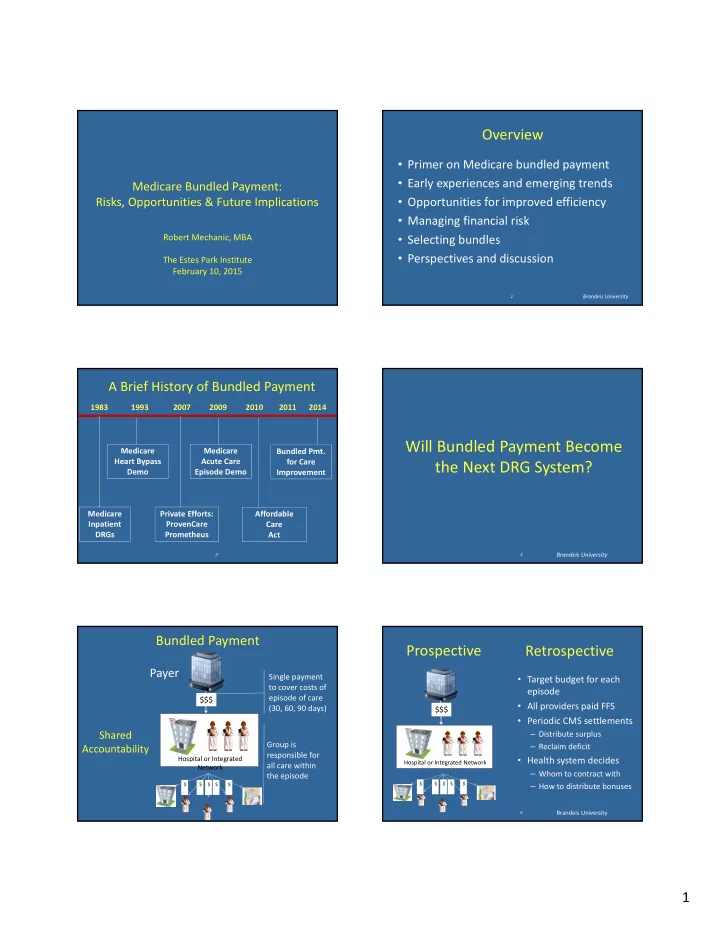
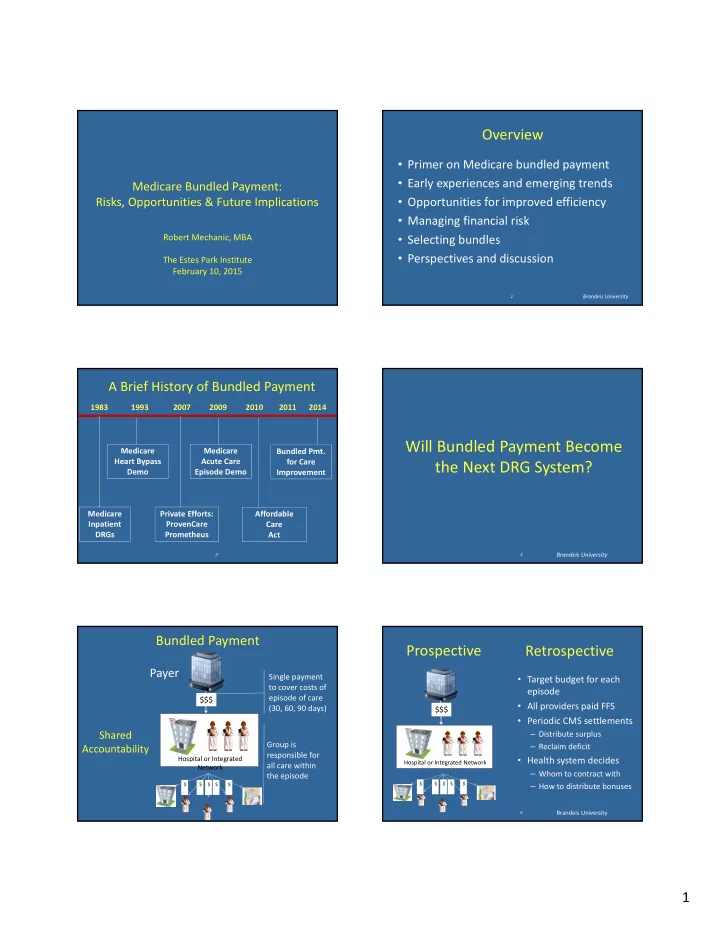
Overview • Primer on Medicare bundled payment • Early experiences and emerging trends Medicare Bundled Payment: Risks, Opportunities & Future Implications • Opportunities for improved efficiency • Managing financial risk Robert Mechanic, MBA • Selecting bundles • Perspectives and discussion The Estes Park Institute February 10, 2015 Brandeis University 2 A Brief History of Bundled Payment 1983 1993 2007 2009 2010 2011 2014 Will Bundled Payment Become Medicare Medicare Bundled Pmt. Heart Bypass Acute Care for Care the Next DRG System? Demo Episode Demo Improvement Medicare Private Efforts: Affordable Inpatient ProvenCare Care DRGs Prometheus Act 4 Brandeis University 3 Bundled Payment Prospective Retrospective Payer Single payment • Target budget for each to cover costs of episode episode of care $$$ • All providers paid FFS (30, 60, 90 days) $$$ • Periodic CMS settlements Shared – Distribute surplus Group is – Reclaim deficit Accountability responsible for Hospital or Integrated • Health system decides Hospital or Integrated Network all care within Network – Whom to contract with the episode $ $ $ $ $ $ $ $ $ $ – How to distribute bonuses Brandeis University 6 1
Opportunities to Improve Margins Primary • Reduce supply costs (e.g. implants) CMS Innovation Center: • Reduce unnecessary consults & testing Bundled Payment Pilot • Reduce errors and complications • Reduce post ‐ acute care costs Conditional (dependent on backfill) • Reduce readmissions • Reduce length of stay Brandeis University Brandeis University 7 8 CMMI Bundled Payment Pilot CMMI Bundled Payment Pilot Model 1 Model 2 Outpatient Professional Outpatient Professional Professional Professional Inpatient Professional Inpatient Professional services services Inpatient Inpatient Readmission Readmission SNF SNF Index Hospitalization Index Hospitalization Stays Stays 90 day look ‐ forward 30 ‐ 90 day look ‐ forward Brandeis University Brandeis University CMMI Bundled Payment Pilot CMMI Bundled Payment Pilot Model 3 Model 4: Prospective Payment Outpatient Professional Outpatient Professional Professional Professional Inpatient Professional Inpatient Professional services services Inpatient Inpatient Readmission Readmission SNF SNF Index Hospitalization Index Hospitalization Stays Stays 30 day look ‐ forward 30 day look ‐ forward Brandeis University Brandeis University 2
Choices for Bundlers Gainsharing • Select bundles • CMS gets first 2% of savings (90 ‐ day episodes) – 48 bundles (encompassing DRG families) • Additional savings can be shared between – Covering about 70% of Medicare payments facility, physicians, post ‐ acute providers – Must take all patients in selected bundles – Physician gain share capped at 50% of Medicare • Exclusions (not optional) – No cap on other providers – Readmissions and Part B services • Useful principals – Revised and improved but ….. (328 for 469) – Quality gates to ensure clinical performance • Select bundle length (30, 60, 90) – Distribute based on contribution and performance • Select risk track Brandeis University Brandeis University 13 14 Financial Model 2009 ‐ 12 2014 Historical Update Factor * Target Price Cost Per CMS Discount Episode $18,200 * For illustration $18,200 update = 1%/yr BPCI Experience Year 1 Settlement discount = 2% $900 Actual Episode Definitions FFS Cost Winsorization $17,300 15 16 Brandeis University Initial BPCI Enrollment Was Modest 2014 Model 2 Enrollment Was Limited Hospitals by Number of Episodes Selected Number of Organizations at Risk in 2014 60 120 50 100 40 80 30 56 60 111 20 89 40 10 20 16 11 9 20 0 15 10 0 1 2 3 ‐ 8 11 ‐ 18 24 ‐ 48 Model 1 Model 2 Model 3 Model 4 Number of Episodes Selected in 2014 Brandeis University Brandeis University 17 18 Source: BPCI participant file (July 24, 2014) downloaded from CMMI website. 3
BPCI Experience in 2014 BPCI Trend Factors: 2012 ‐ 2014 (Q2) • Program start delayed from Jan 13 to Jan 14. • New round announced ‐ LOI due April 2014 • Q1 reconciliation files distributed in October with many of surprises • Large bundler push back • CMS announces no downside risk for 2014 Source: CMS M2 common template file for BPCI reconciliation 2014 Q2. Brandeis University Brandeis University 19 20 Model 2: Conveners for Hospitals Applications for 2015 Model 2 Model 3 Institutions 1,054 3,280 MD Groups 957 645 Total 2,011 3,925 Source: BPCI participant file (July 24, 2014) downloaded from CMMI website. • Must commit to “risk” for at least one episode by April 13 • May add episodes up to October 1, 2015 Source: BPCI participant file (July 24, 2014) downloaded from CMMI website. 21 Brandeis University 22 Brandeis University Model 2: Conveners for Physicians The Financial Opportunity of Bundled Payment Medicare Spends a Tremendous Amount in the 30 – 90 Days After Patients Are Discharged from the Hospital Source: BPCI participant file (July 24, 2014) downloaded from CMMI website. Brandeis University 23 24 4
Average 2013 Medicare Inpatient Payments Medicare Post Acute Care Spending Select Episodes for Sample Hospital $40,000 2012 Medicare Spending by Type 2008 Medicare Spending for $35,000 Hospitalization plus 30 Days 21% $30,000 34% $25,000 $20,000 $15,000 $10,000 Hospital IP Professional $5,000 Hospital IP Professional Post ‐ Acute Post ‐ Acute Hospital OP $0 Major Joint CHF COPD Renal Fail. PCI Spinal Fusion Source: RTI Inc, Post ‐ Acute Care Episodes: Expanded Source: MedPAC, 2014 Data Book (Charts 1 ‐ 1, 8 ‐ 2). Analytic File, June 2011 p.216. Brandeis University Source: Brandeis University analysis of Medicare Claims. 25 26 Avg. 2013 Medicare 90 ‐ Day Episode Price for Index Stay & Post Acute: Sample Hospital $40,000 $35,000 29% $30,000 $25,000 45% $20,000 48% 70% $15,000 71% 69% $10,000 $5,000 $0 Major Joint CHF COPD Renal Fail. PCI Spinal Fusion Index Admission Post Acute Thinking About Post ‐ Acute Care Source: Brandeis University analysis of Medicare claims data. 27 28 Brandeis University Average 2009 Post ‐ Acute Care Spending per Episode for Total Joint Replacement (90 day) There is Significant Variation in Post ‐ Acute Care Spending Across $16,000 $12,000 $14,000 Hospitals …. $12,000 $10,000 $6,000 $8,000 …. And Many Opportunities to $6,000 Reduce Post ‐ Acute Care Spending $4,000 $2,000 $0 A B C D E F G H I J K L M N O P Q R “St. Minimus” “St. Maximus” Source: Brandeis University analysis of Medicare Claims data. Figures adjusted for hospital wage 29 30 index. 5
A Tale of Two Hospitals: Joint A Tale of Two Hospitals: Joint Replacement Episode Replacement Episode 80.0% 70.0% 60.0% 50.0% 40.0% St. Maximus St. Minimus 30.0% 20.0% 10.0% 0.0% Readmission Rate Pct. SNF Pct. Home Health 31 Source: Brandeis University analysis of Medicare Claims data. 32 Source: Brandeis University analysis of Medicare Claims data. Unadjusted data. Opportunities for St. Maximus • Expand home health and reduce use of SNF services where appropriate • Put a program in place to monitor patients Picking Bundles for BPCI following discharge – Medication reconciliation – Home assessment – Primary care visit within 7 days – Emergency plan for likely events • Consider preferred relationships with collaborative & high value facilities. 33 34 Spending for Top Clinical Episode: 2009 ‐ 12 Considerations for Bundle Selection • Commitment level – learning or major strategy • Stability of year to year bundle prices – Volume – Variation • Performance/spending relative to local market • Opportunity to reduce wasteful spending • Likely ability to effect clinical changes Source: Claims data from sample hospital. 6
**: DRG Spending by Category Episode Price vs. State Average Procedural Bundles Chronic Bundles $40,000 $35,000 $30,000 $25,000 $20,000 $15,000 $10,000 $5,000 $0 Inpatient Part B Post Acute Note: Hospital mean and state mean are winsorized and normalized to a common wage index. Illustrative Spending: Hospital vs. State Post ‐ Acute Spend: Hospital vs. State Spending per Case for Surgical Bundles Major Spending Categories for Surgical Bundles Note: All DRG bundle cost comparisons are unadjusted for geographic wage index. Note: All DRG bundle cost comparisons are unadjusted for geographic wage index. * Hospital spending for IRF/LTAC significantly exceeds state average. * Hospital spending for IRF significantly exceeds state average. Post ‐ Acute: Hospital vs. State Episode Price Variance: Risk Track A Spending per Case for Chronic/Medical Bundles Brandeis University 41 7
Recommend
More recommend