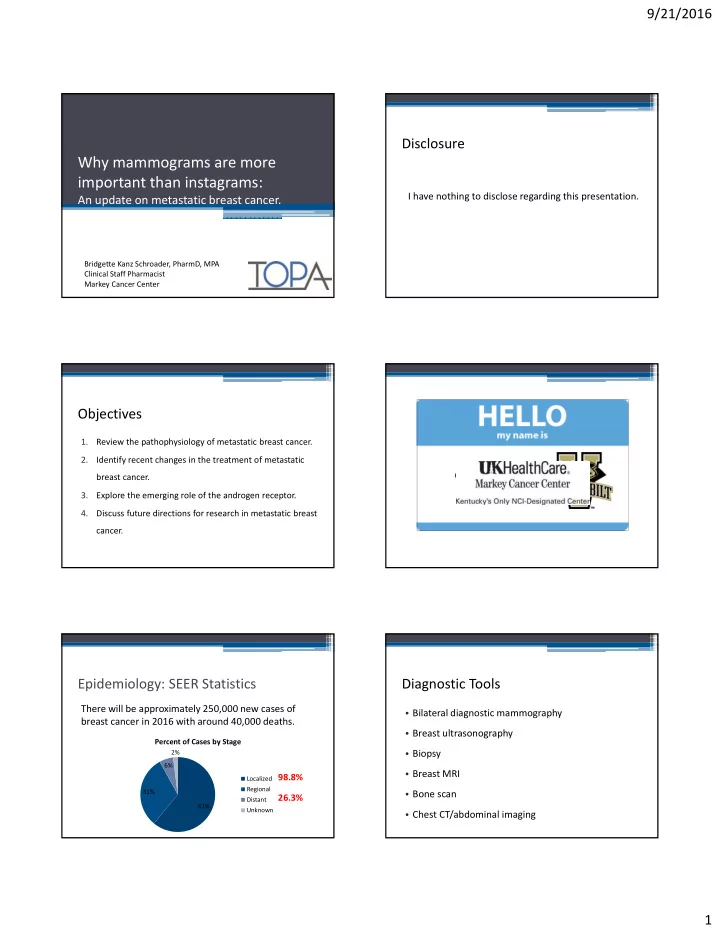
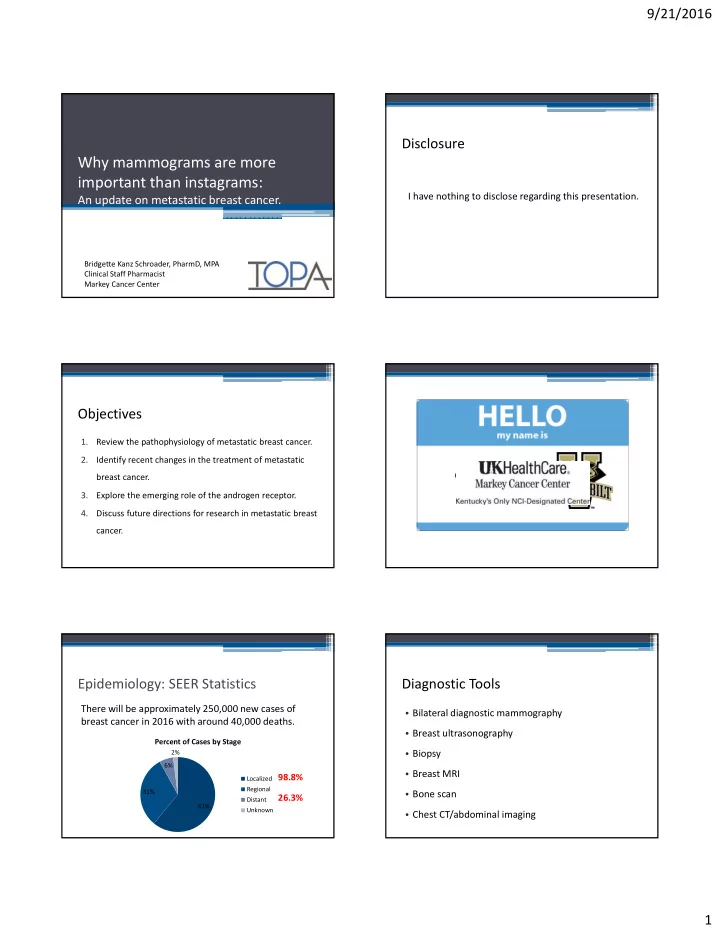
9/21/2016 Disclosure Why mammograms are more important than instagrams: I have nothing to disclose regarding this presentation. An update on metastatic breast cancer. Bridgette Kanz Schroader, PharmD, MPA Clinical Staff Pharmacist Markey Cancer Center Objectives 1. Review the pathophysiology of metastatic breast cancer. 2. Identify recent changes in the treatment of metastatic breast cancer. 3. Explore the emerging role of the androgen receptor. 4. Discuss future directions for research in metastatic breast cancer. Epidemiology: SEER Statistics Diagnostic Tools There will be approximately 250,000 new cases of • Bilateral diagnostic mammography breast cancer in 2016 with around 40,000 deaths. • Breast ultrasonography Percent of Cases by Stage • Biopsy 2% 6% • Breast MRI 98.8% Localized Regional • Bone scan 31% 26.3% Distant 61% Unknown • Chest CT/abdominal imaging 1
9/21/2016 Pathogenesis Staging • Staging is determined using the American Joint Committee on Cancer TNM Staging System for Breast Cancer (Tumor, Node, Metastases) • This includes traditional TNM as well as pathologic lymph node staging based on lymph node dissection • Staging also includes assigning a histologic grade and histopathologic subtype Pandya and Moore. Clin Obstet Gynecol, 2011. Wong and Rebelo. McMaster Pathophysiology Review, 2016. Pathogenesis Pandya and Moore. Clin Obstet Gynecol, 2011. National Cancer Institute, 2016. Wong and Rebelo. McMaster Pathophysiology Review, 2016. Histological Subtype Ductal Lobular Preinvasive Cancer Ductal carcinoma in situ Lobular carcinoma in situ Alphabet Soup 25% May spread through ducts Does not distort duct Cells limited to basement and distort duct architecture architecture membrane 1% progress to invasive 1% progress per year • Histological subtype cancer per year Can be bilateral Usually unilateral • Molecular subtype: Invasive Cancer Invasive ductal carcinoma Invasive lobular carcinoma ▫ HER2+ or HER2 ‐ 75% Usually from DCIS precursor Usually from LCIS precursor ▫ Hormone receptor (HR) + or HR ‐ Extension beyond the Cause fibrous response, Minimal fibrous response, basement membrane producing a palpable mass presents less often with ▫ Triple negative breast cancer (TNBC) on examination palpable mass Metastasis through Mets through abdominal lymphatics and blood viscera • Menopausal status Almost always ER+ Wong and Rebelo. McMaster Pathophysiology Review, 2016. 2
9/21/2016 Molecular Subtype: HER2/neu • Human Epidermal Growth Factor Receptor 2 • HER2/neu is a proto ‐ oncogene that encodes transmembrane receptors for growth factors including EGFR, HER2, 3 and 4. • HER2 has intracellular tyrosine kinase activity that affects physiology, growth and differentiation of cells while extracellular domains interact with HER family members and facilitate transduction. • There is no known ligand for HER2. • Amplification of the HER2/neu oncogene results in up to 100x physiologic levels of HER2 facilitating tumorigenesis. Burstein. N Engl J Med, 2005. Malhotra et al. Caner Biol Ther, 2010. Molecular Subtype: Hormone Receptor Status • Refers to expression of estrogen and progesterone receptors on tumor cells • The effects of estrogen are mediated through ER ‐α and ER ‐β . ER ‐α is the dominant isoform and correlates with the most prognostic factors in breast cancers. • The progesterone receptor is not as well studied but is an ER ‐ regulated gene. Two isoforms, PR ‐ A and B, are linked to cancer progression. Marker, 2016. Image: The Lancet. Pietras, RJ. Oncologist, 2006. Molecular Subtype: TNBC • ER, PR, HER2 negative • Represents 15 ‐ 20% of breast cancer carcinoma • Generally a large, aggressive primary tumor • More likely to occur in younger patients (< age 50), African American or Hispanic women or those with BRCA1 mutation Yager and Davidson. NEJM, 2006. Foulkes et al. N Engl J Med, 2010. 3
9/21/2016 Menopause Menopausal status: why does it matter? Defined as the permanent cessation of menses. • Production of estrogen varies. Since the inhibition of Criteria include: estrogen is related to therapy, it’s important to target • Age 60 years or older the appropriate production center. • Age less than 60 years and amenorrheic for 12 or more months in the absence of chemo, tamoxifen, toremifene • Premenopausal women produce the majority of 17 β‐ or ovarian suppression, and FSH and estradiol in the postemenopausal range estradiol in their ovaries while postmenopausal • If taking tamoxifen or toremifene and age younger than 60, then FSH and plasma estradiol in postmenopausal women produce the majority in extragonadal sites. ranges NCCN, 2016. Simpson. J Steroid Biochem Mol Biol, 2003. General Treatment: HR+, HER2 ‐ or + • Prior endocrine therapy within 1 year ▫ Ovarian ablation or suppression (OA/S) (if premenopausal) + endocrine therapy Current Treatment • No prior endocrine therapy within 1 year ▫ Premenopausal: OA/S + endocrine therapy or SERM ▫ Postmenopausal: AI or SERM or selective ER down ‐ • HR+, HER2 ‐ regulator • Continue sequential endocrine therapy until no benefit after 3 regimens or visceral crisis • HR+, HER2+ • Visceral crisis ▫ Chemotherapy • TNBC General Treatment: HR+, HER2 ‐ or + General Treatment: HR ‐ , HER2+ • Non ‐ steroidal aromatase inhibitors (anastrozole, • Preferred first line agents letrozole) ▫ Pertuzumab + trastuzumab + docetaxel (category 1) • Steroidal aromatase inactivator (exemestane) ▫ Pertuzumab + trastuzumab + paclitaxel • Exemestane + everolimus • Other options • Palbociclib + letrozole ▫ Ado ‐ trastuzumab emtansine (T ‐ DM1) • Palbociclib + fulvestrant (category 1) ▫ Trastuzumab + paclitaxel +/ ‐ carboplatin, + docetaxel, + • Fulvestrant • Tamoxifen or toremifene vinorelbine, + capecitabine • Megestrol acetate • Agents for trastuzumab exposed disease • Fluoxymesterone ▫ Lapatinib + capecitabine • Ethinyl estradiol ▫ Trastuzumab + capecitabine, + lapatinib or others 4
9/21/2016 General Treatment: Summary General Treatment: TNBC • Preferred single agents ▫ Anthracyclines: doxorubicin, liposomal doxorubicin ▫ Taxanes: paclitaxel ▫ Anti ‐ metabolites: capecitabine, gemcitabine ▫ Microtubule inhibitors: vinorelbine, eribulin • Combinations: CAF/FAC, FEC, AC, EC, CMF, docetaxel/capecitabine, GT, gem/carbo, paclitaxel/bevacizumab • There is no compelling evidence that combination regimens are superior to sequential single agents Wong and Rebelo. McMaster Pathophysiology Review, 2016. Hormone Receptor Positive Disease • CDK4/6 pathway inhibition • Endocrine therapy combinations Recent Advances • HR+ • TNBC Impact in Metastatic Disease: The action ‐ reaction hypothesis Estrogen Receptor Resistance • Over time estrogen receptor resistance develops to endocrine therapy • Ligand dependent resistance mechanisms ▫ Receptor amplification, increased circulating hormone or endogenous hormone ▫ Receptor hypersensitivity, changing ratio of coregulators • Ligand independent resistance mechanisms ▫ Receptor mutation, crosstalk, bypass receptors ▫ Loss of receptors Rau et al. Endocr Relat Cancer, 2005. 5
9/21/2016 Estrogen Receptor Resistance CDK4/6 Pathway • ER ‐α mutations promote ligand independent • Cyclin ‐ dependent kinases 4 and 6 phosphorylate proteins receptor activation and resistance to various such as retinoblastoma tumor suppressor protein and therapies others to promote synthesis of genes important for DNA • Chandarlapaty et al analyzed 541 patients from the replication and movement through the cell cycle BOLERO ‐ 2 trial (prior AI exposure) looking at D538G • Tumors increase CDK dependent activity through a and Y537S mutations variety of mechanisms including p16 inactivation, CDK4 • Mutation prevalence of 28.8% overall. amplification or mutation, cyclin D1 overexpression or ▫ WT OS 32.1mo (CI 28 ‐ 36mo) translocation or amplification of an encoding gene ▫ D538G OS 25.99 mo (CI 19 ‐ 32mo) • Inhibition of CDK4/6 results in cell cycle arrest from G 1 to ▫ Y537S OS 19.98 mo (CI 13 ‐ 29mo) the S phase of the cell cycle Chandarlapaty et al. JAMA Oncol, 2016. Murphy and Dickler et al. Oncol, 2015. CDK4/6 Pathway Palbociclib + Letrozole (P+L) PALOMA ‐ 2 P 125mg/d po 3 wks on/1 off + L (2.5mg/d) Phase III Key Eligibility: Randomized Controlled R ER+, HER2 ‐ advanced • Double ‐ 2:1 breast cancer blind N = 666 Treatment naive • Placebo + L *Patients were stratified by disease site, disease free interval from (neo)adjuvant tx, p prior HT (yes/no) (y / ) Murphy and Dickler et al. Oncol, 2015. Finn et al. JAMA Oncol, 2016. Palbociclib + Fulvestrant (P+F) PALOMA ‐ 2 Results PALOMA ‐ 3 P (125mg/d 3wk on/1 off) + F • Median PFS 24.8 months for combo vs 14.5mo (HR 0.58 Key Eligibility: (500mg IM D1, 15 C1 then D1 [0.46 ‐ 0.72], p <0.01) HR+, HER2 ‐ q28d) Phase III • • ORR improved with the combination from 34.7% to Randomized Progressed on previous • Controlled endocrine therapy 42.1% (p = 0.031) R Multicenter ECOG PS 0 ‐ 1 • 2:1 • Clinical benefit rate was defined as CR + PR + SD ≥ 24 Double Measurable disease or • N = 521 blind bone disease only weeks and was 84.9% with combo vs 70.3% (p<0.01) Relapse or progression • • ADE Placebo + F during tx or <12 mo ▫ Most common severity seen was G3 neutropenia (56.1%) *Patients were stratified by sensitivity to ▫ Discontinuation was higher in combo with 9.7% vs 5.9% previous tx, menopausal status, and • Caveat: overall survival data is pending p presence of visceral mets Cristofanilli et al. JAMA Oncol, 2016. 6
Recommend
More recommend