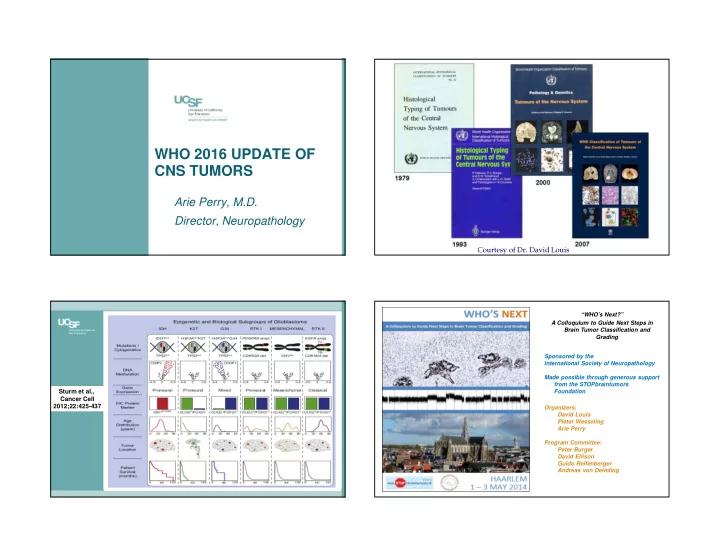
WHO 2016 UPDATE OF CNS TUMORS Arie Perry, M.D. Director, Neuropathology Courtesy of Dr. David Louis “WHO’s Next?” A Colloquium to Guide Next Steps in Brain Tumor Classification and Grading Sponsored by the International Society of Neuropathology Made possible through generous support from the STOPbraintumors Sturm et al., Foundation Cancer Cell 2012;22:425-437 Organizers: David Louis Pieter Wesseling Arie Perry Program Committee: Peter Burger David Ellison Guido Reifenberger Andreas von Deimling
Brain Pathology 24: 429-435, 2014 Challenge: balancing desires and needs • Do not disrupt current clinical diagnosis and patient management • Weigh the availability and cost of novel diagnostic techniques • Incorporate the latest • Preserve the ability for molecular signatures long-term clinical, • Utilize the most accurate, experimental and cutting-edge techniques etiological correlations Courtesy of Dr. David Louis “Don’t throw the baby out with the bathwater”: “Das Kind mit dem Bade ausschütten” • Baby = roughly a century of clinicopathologic experience, tight correlations with outcome, and cost efficiency of light microscopy • Bathwater = subjectivity, diagnostic pitfalls, histologic mimicry, lack of sufficient reproducibility Earliest record from Narrenbeschwörung Courtesy of Dr. Pieter Wesseling (Appeal to Fools) by Thomas Murner, 1512
World map by quartiles of Human ISN-Haarlem conclusions (1) Development Index in 2013 • Disease entities should be defined as narrowly as possible in order to establish highly biologically uniform groups (i.e., as previously undertaken by the hematopathology community) • Molecular information will be incorporated into the definitions of some diagnostic entities • For others, histology will remain the basis for definition and diagnosis Brain Pathology 24: 429-435, 2014 ISN-Haarlem conclusions (2) ISN-Haarlem format of “layered diagnoses” “Integrated Diagnoses”: a layered approach • Integrated Diagnosis (incorporating all aspects of tissue diagnosis) • Histological Classification • WHO Grade (natural history) • Molecular information (see parameters from previous slide) “ISN-Haarlem layered diagnosis format” I II III IV I II III IV I II III IV
BIOMARKER CONCEPTS • Types – Diagnostic – Prognostic – Predictive • Practicality issues – Cost and ease of implementation – IHC vs. FISH vs. PCR vs. genomics – Reimbursement School of Medicine
OLIGODENDROGLIOMA NGS SCATTER PLOT OLIGODENDROGLIOMA 1p19q FISH UCSF 500 Gene Panel 1p32 19p13 1q42 19q13 Courtesy of Dr. Nancy Joseph, UCSF Molecular Pathology E. Talevich, A. H. Shain, B. C. Bastian, CNVkit: Copy number detection and visualization for School of Medicine School of Medicine targeted sequencing using off-target reads. bioRxiv (2014), doi:10.1101/010876 GBM BIOMARKER: MGMT METHYLATION Hegi ME et al., NEJM 352;10:997, 2005 School of Medicine MGMT
Sanger DNA Sequencing of Normal and Methylated MGMT Promoter from GBM Tumor Sections Not Methylated Methylated 321(5897):1807-12, 2008 Methylated Courtesy of Dr. Farid Chehab, UCSF Molecular Pathology DIAGNOSTIC EXAMPLE OF HISTOLOGIC IDH-1 R132H IHC MIMICRY: “ELVIS IMPERSONATOR” • AO (IDHm and 1p/19q codeletion) – Average survival 15 years with 1p/19q loss if treated with combined PCV chemo and radiation – What about chemo alone up front? • SC-GBM (IDHwt, EGFR-AMP 70%, -10q 95%) – Average survival 1 year – Typically treated with combined radiochemotherapy – Different set of clinical trials than the high-grade oligodendrogliomas School of Medicine School of Medicine
CANCER CELLS ESCAPING SENESCENCE Reitman et al. Acta Neuropathol (2013) 126:789–792 Shay JW et al. Science 15:1388-1390, 2012 ATRX/H3.3 alterations � ALT Killela et al. PNAS 2013; 110: 6021–6026
ALT FISH ATRX IHC TERT ADULT ADULT TYPE ASTROCYTOMA GLIOMAS ATRX IDH1/2 TP53 Killela et al. PNAS 2013; 110: 6021–6026 TERT IDH 1p/19q-del IDH1 p53 ATRX
Astro, IDHm GBM, IDHwt IDHwt EGFR-amp DIFFUSE MIDLINE GLIOMA (DIPG, THAL, SC) Preneoplastic IDHm TERTm TP53m Cell ATRXm IDHm TERTm CICm 9p (CDKN2A/B) LOH 1p19q-codel FUBP1m AA, IDHm Oligo, IDHm, Diffuse midline 1p19q-codel glioma, H3-K27Mm PIK3R1/PIK3CAm 4q LOH? PIK3CAm? GBM, IDHm AO, IDHm, 1p19q-codel Note: no oligoastro! H3 K27M p53 ATRX DIFFUSE ASTROCYTOMA GRADING Atypia IS IT VALID TO COMBINE TRADITIONAL Mitoses GLIOMA GRADING CRITERIA WITH NEW Endothelial Proliferation (MVP, EH) MOLECULAR DEFINITIONS FOR CELL TYPE (e.g. IDHm)? Necrosis WHO II=A; III=A+M; IV=A+M+(E or N) School of Medicine School of Medicine
IDHwt 372: 2499-2508, 2015 NEW WHO GLIOMA ENTITIES, Oligos VARIANTS, AND PATTERNS Astros IDHm • Diffuse midline glioma, H3 K27M mutant ~90% (entity) 1 0 GBMs? • Diffuse leptomeningeal glioneuronal tumor (entity) • Epithelioid glioblastoma (provisional variant) IDHm • Glioblastoma with primitive neuronal 2 0 GBMs ~10% component (pattern) 1 0 GBMs • Anaplastic PXA (entity) School of Medicine
(2012) 124: 627-641 1p BRAF 1q KIAA1549 OLIG2 SYN AJSP 2010; 34:341-54 AJSP 2013; 37:658-98 NAN 2014; 40:327-36
GFAP OLIG2 BRAF-V600E
PXA Epithelioid EMBRYONAL CNS TUMORS WHO 2016 SCHEME • Medulloblastomas – Large cell / anaplastic • ET c multilayered ros- – WNT-activated ettes, C19MC-altered – SHH-activated and TP53 -mutant • Medulloepithelioma – SHH-activated and • CNS Neuroblastoma / TP53 -wildtype Ganglioneuroblastoma – Non-WNT/non-SHH • CNS ET, NOS – Classic • Atypical teratoid / – Desmoplastic/nodular rhabdoid tumor – MB c extensive nodularity (no ‘PNETs’) School of Medicine Taylor et al., Acta Neuropathol 2012;123:465-472 School of Medicine
WNT MOL SUBTYPE SHH MOL SUBTYPE β -catenin- β -catenin+ GAB-1 p53
AT/RT Ho et al. Acta Neuropathol 99:482, 2000 School of Medicine INI1 CASE • 46 yo man • New onset seizures EXAMPLES • MRI: non-enhancing L fronto- temporal mass • Resection performed School of Medicine School of Medicine
School of Medicine School of Medicine POSSIBLE INITIAL REPORT POSSIBLE FINAL REPORT 1. Integrated Diagnosis: pending 1. Integrated Diagnosis: Oligodendroglioma, WHO grade II, IDH1m, 1p19q codeleted 2. Histologic diagnosis: oligoastrocytoma (or ambiguous diffuse glioma) with scattered 2. Histologic diagnosis: oligoastrocytoma (or mitoses, but no MVP or necrosis ambiguous diffuse glioma) with scattered mitoses, but no MVP or necrosis 3. WHO grade: II 3. WHO grade: II 4. Molecular studies: pending 4. Molecular studies: IDH1 R132H mutant protein positive by IHC, 1p19q codeletion by FISH
ACTUAL FINAL REPORT EXAMPLE 2: POSSIBLE INITIAL REPORT 1. Integrated Diagnosis: Diffuse astrocytoma, IDH- 1. Integrated Diagnosis: pending mutant, WHO grade II 2. Histologic diagnosis: oligoastrocytoma (or 2. Histologic diagnosis: oligoastrocytoma (or ambiguous ambiguous diffuse glioma) with atypia, mitoses, diffuse glioma) with scattered mitoses, but no MVP or MVP, and necrosis necrosis 3. WHO grade: II 3. WHO grade: at least III 4. Molecular studies: 1p19q intact, IDH1 R132H mutant 4. Molecular studies: pending on sequencing and IHC, ATRX loss of expression by IHC, p53 overexpression by IHC POSSIBLE FINAL REPORT POSSIBLE FINAL REPORT 1. Integrated Diagnosis: AO, WHO III, IDHm, 1p19q 1. Integrated Diagnosis: AO, WHO III, IDHm, 1p19q codeleted, ATRX intact codeleted, ATRX intact 2. Integrated Diagnosis: GBM (secondary type), 2. Integrated Diagnosis: GBM (secondary type), WHO IV, IDHm, 1p19q intact, ATRX loss WHO IV, IDHm, 1p19q intact, ATRX loss 3. Integrated Diagnosis: GBM (primary type), WHO 3. Integrated Diagnosis: GBM (primary type), WHO IV, IDH intact, 1p19q intact, ATRX intact, +/- IV, IDH intact, 1p19q intact, ATRX intact, +/- EGFR-AMP EGFR-AMP 4. Diagnosis: Diffuse glioma, NOS, at least WHO 4. Diagnosis: Diffuse glioma, NOS, at least WHO grade III (molecular studies not performed) grade III (molecular studies not performed)
Performance of ‘Brain Tumor Rhapsody’ by Musaic (https://www.youtube.com/watch?v=FfP4HTuu6V)
Recommend
More recommend