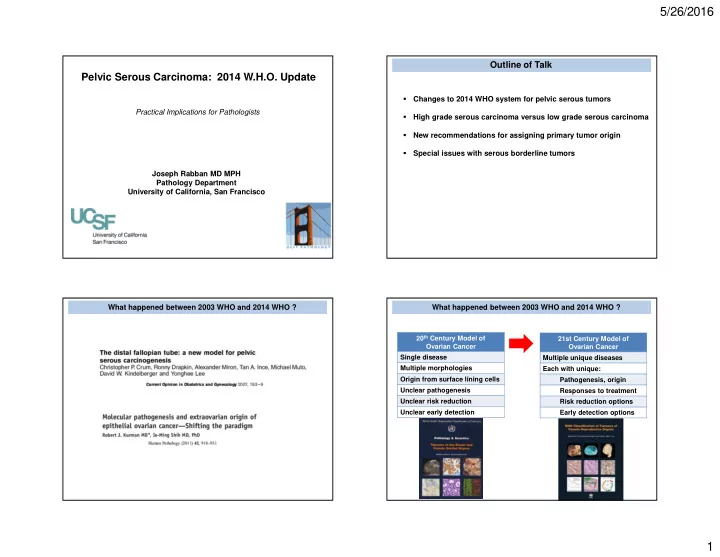
5/26/2016 Outline of Talk Pelvic Serous Carcinoma: 2014 W.H.O. Update Changes to 2014 WHO system for pelvic serous tumors � Practical Implications for Pathologists High grade serous carcinoma versus low grade serous carcinoma � New recommendations for assigning primary tumor origin � Special issues with serous borderline tumors � Joseph Rabban MD MPH Pathology Department University of California, San Francisco What happened between 2003 WHO and 2014 WHO ? What happened between 2003 WHO and 2014 WHO ? 20 th Century Model of 21st Century Model of Ovarian Cancer Ovarian Cancer Single disease Multiple unique diseases Multiple morphologies Each with unique: Origin from surface lining cells Pathogenesis, origin Unclear pathogenesis Responses to treatment Unclear risk reduction Risk reduction options Unclear early detection Early detection options 1
5/26/2016 Ovarian Carcinomas in 2014 WHO 3 Major Changes to Pelvic Serous Tumors in 2014 WHO 2003 2014 High grade serous carcinoma (HGSC) 1 Tumor Class Surface epithelial – stromal Epithelial tumors tumors Low grade serous carcinoma (LGSC) Clear cell carcinoma Endometrioid adenocarcinoma Mucinous carcinoma Rationale: New Evidence Tumor origin is fallopian tube mucosa (either in tube as STIC or in ovary as epithelial inclusion cyst) Implications Fallopian tube is target for risk reduction, early detection Proposed Tubal Origins of Ovarian HGSC versus LGSC Proposed Tubal Origins of Ovarian HGSC versus LGSC Benign tubal P53 mucosa Tubal HGSC (STIC) Inclusion gland Ovarian HGSC P53 Ovarian HGSC 2
5/26/2016 Proposed Tubal Origins of Ovarian HGSC versus LGSC Proposed Tubal Origins of Ovarian HGSC versus LGSC p53 Benign tubal Tubal HGSC (STIC) mucosa benign spread Inclusion Inclusion gland gland p53 Ovarian BRAF Ovarian Ovarian Serous HGSC KRAS LGSC Borderline Tumor MAPK pathway BRAF Ovarian Ovarian Serous KRAS LGSC Borderline Tumor MAPK pathway 3 Major Changes to Pelvic Serous Tumors in 2014 WHO 3 Major Changes to Pelvic Serous Tumors in 2014 WHO 2003 2014 2003 2014 1 Tumor Class Surface epithelial – stromal Epithelial tumors 1 Tumor Class Surface epithelial – stromal Epithelial tumors tumors tumors 2 Serous One tumor, grade 1,2,3 Two tumors: HGSC, LGSC 2 Serous One tumor, grade 1,2,3 Two tumors: HGSC, LGSC Carcinoma Carcinoma 3 Transitional cell Unique tumor Eliminated. Viewed as carcinoma variant of HGSC Rationale: Rationale: New Evidence Distinct behavior, response to therapy, genetics, pathogenesis, origin New Evidence “TCC” has same properties as HGSC Implications Distinct surgical planning, adjuvant therapy, genetic counseling, risk Implications Diagnosis of HGSC includes many reduction different patterns beyond papillary (TCC, endometrioid, solid) 3
5/26/2016 Outline of Talk High Grade Serous Carcinoma Low Grade Serous Carcinoma HGSC LGSC Changes to 2014 WHO system for pelvic serous tumors � High grade serous carcinoma versus low grade serous carcinoma � New recommendations for assigning primary tumor origin � Special issues with serous borderline tumors � LGSC: Clinico-pathologic Features HGSC LGSC BRCA hereditary syndrome ~25 % No Incidence ~5 % of all ovarian cancers Average 4 th to 5 th decade Age P53 mutation Yes No Risk factors No traditional HGSC risk factors BRAF KRAS MAPK pathway defects No Common 20% risk if prior history of advanced stage serous borderline tumor Precursor lesion STIC Borderline ~ risk if prior ovulation induction for fertility tumor Hereditary ? No major syndrome known Platinum chemotherapy sensitive Yes Uncommon Stage >75% are advanced stage at diagnosis PARP inhibitor sensitive Yes Unlikely Median survival ~80-96 months Neoadjuvant chemotherapy candidate Yes No Time to recurrence ~33 months if optimal cytoreduction ~14 months if suboptimal cytoreduction MAPK pathway inhibitor candidate No Yes Romero 2013 Gyn Oncol Fader 2013 Ob Gynecol 4
5/26/2016 HGSC HGSC: Papillary pattern Architecture � Papillary Micro-papillary Solid Pseudo-endometrioid (cribriform) Transitional cell carcinoma-like Cytology � High nucleus-cytoplasm ratio Pleomorphism Nuclear hyperchromasia Brisk / atypical mitoses Macro-nucleoli HGSC: Papillary pattern HGSC: Transitional cell cancer-like pattern Pleomorphism, high N/C ratio, brisk mitoses 5
5/26/2016 HGSC: Transitional cell cancer-like pattern HGSC: Pseudo-endometrioid pattern HGSC HGSC: Pseudo-endometrioid pattern Immunophenotype � Mullerian origin + PAX8, CK7 Extra-uterine serous differentiation + WT1 High grade serous carcinoma Aberrant p53, p16 6
5/26/2016 p53 and Pelvic HGSC p53 and Pelvic HGSC p53 gene mutation p53 IHC stain result Normal p53 gene p53 IHC stain result Diffuse, strong staining ~80% Weak patchy staining (“Normal” / Wild type) ~20% Completely negative p53 Stain Interpretation in Pelvic Serous Carcinoma p53 Stain Interpretation in Pelvic Serous Carcinoma Aberrant p53 Aberrant p53 Wild type p53 Pattern of p53 IHC staining Stain Interpretation Diagnosis HGSC HGSC not HGSC* Strong/diffuse Aberrant p53 HGSC Completely negative Weak/patchy Wild type p53 (normal) not HGSC * Check for internal control 7
5/26/2016 p16 Stain Interpretation in Pelvic Serous Carcinoma Use both p53 and p16 stains for HGSC Diffuse / strong = Patchy or negative = Aberrant p16 Wild-type p16 � Cannot use p53 alone if result is wild type � 4% of HGSC are wild type p53 / aberrant p16 Always do both stains together LGSC MD Anderson Criteria for LGSC Architecture � Papillary branching Micro-papillary Bud-like Macro-papillary Cribriform Grading System # of Grading Tiers Cytology � FIGO 3 Uniform, monotonous Shimizu-Silverberg 3 Focal moderate atypia (<3:1 variable size) MD Anderson 2 Mitoses < 12 / 10 hpf Atypical mitoses uncommon 8
5/26/2016 FIGO Universal Grading of Pelvic Cancer (any type) Shimizu-Silverberg Universal Grading of Ovarian Cancer (any type) Points Architecture Atypia Mitoses /10 hpf Grade Solid Architecture 1 Glandular Mild 0-9 1 <6 % 2 Papillary Moderate 10-24 2 6 % – 50% 3 Solid Severe >24 3 > 50% Total Points Overall Grade 3 – 5 1 6, 7 2 8, 9 3 MD Anderson Classification of Ovarian Serous Carcinoma MD Anderson Classification of Ovarian Serous Carcinoma Classification Associated Borderline Progression Nuclei Mild-Moderate Marked Tumor Free Survival Atypia Atypia LGSC 60 % of cases longer Nuclear appearance Uniform Pleomorphic HGSC 2 % of cases shorter Nuclear size/shape < 3 : 1 variability >3 : 1 variability Nucleoli None to small Macro Chromatin Evenly dispersed Coarse Additional Advantages of 2-tier grading: � More predictive than other grading systems � Reproducible (Malpica 2007 AJSP) � Eventually was validated by: Classification Atypia Mitoses / 10 hpf � p53/p16 immunophenotype LGSC Mild to Moderate < 12 � Molecular pathogenesis HGSC Marked 12 or more � Response to therapy � Association with inherited mutations � Used by 2014 W.H.O. 9
5/26/2016 LGSC with Serous Borderline Tumor LGSC: Micropapillary Buds (avascular) LGSC: Micropapillary Buds (avascular) LGSC: Micropapillary Buds (avascular) <3:1 varying size/shape <3:1 varying size/shape No mitoses No mitoses No macronucleoli No macronucleoli 10
5/26/2016 LGSC: Micropapillary Buds (avascular) LGSC: Papillary Branching (vascularized) <3:1 varying size/shape No mitoses No macronucleoli LGSC: Papillary Branching (vascularized) LGSC: Papillary Branching + Buds <3:1 varying size/shape No mitoses No macronucleoli 11
5/26/2016 LGSC: Papillary Branching + Buds LGSC: Papillary Branching + Buds <3:1 varying size/shape No mitoses No macronucleoli LGSC: Branching + Cribriform Pattern LGSC: Branching + Cribriform Pattern 12
5/26/2016 LGSC: Cribriform Pattern LGSC: Columnar cells LGSC: Columnar cells LGSC with Necrosis Positive WT1 Excludes Endometrioid Tumor 13
5/26/2016 Most LGSC Present at Advanced Stage Most LGSC Present at Advanced Stage Omental Involvement Pelvic Lymph Node Metastasis Most LGSC Present at Advanced Stage LGSC Lung Metastasis Immunophenotype � Mullerian origin + PAX8, CK7 Extra-uterine serous differentiation + WT1 Low grade serous carcinoma Wild type p53, p16 14
5/26/2016 Wild type p53 in LGSC LGSC Wild type p53 Wild type p16 Wild Type p53 and p16 staining Diagnostic Challenges Distinguishing LGSC versus HGSC � 89 % Sensitivity for LGSC � 93 % Specificity LGSC with: � Focal mitotic activity � 98 % Negative predictive value � Notable moderate atypia � Rare severe atypia Aberrant results exclude LGSC HGSC with: � Only moderate nuclear atypia � Abundant cytoplasm � Architecture of borderline tumor or cystadenofibroma � Micropapillary architecture 15
Recommend
More recommend