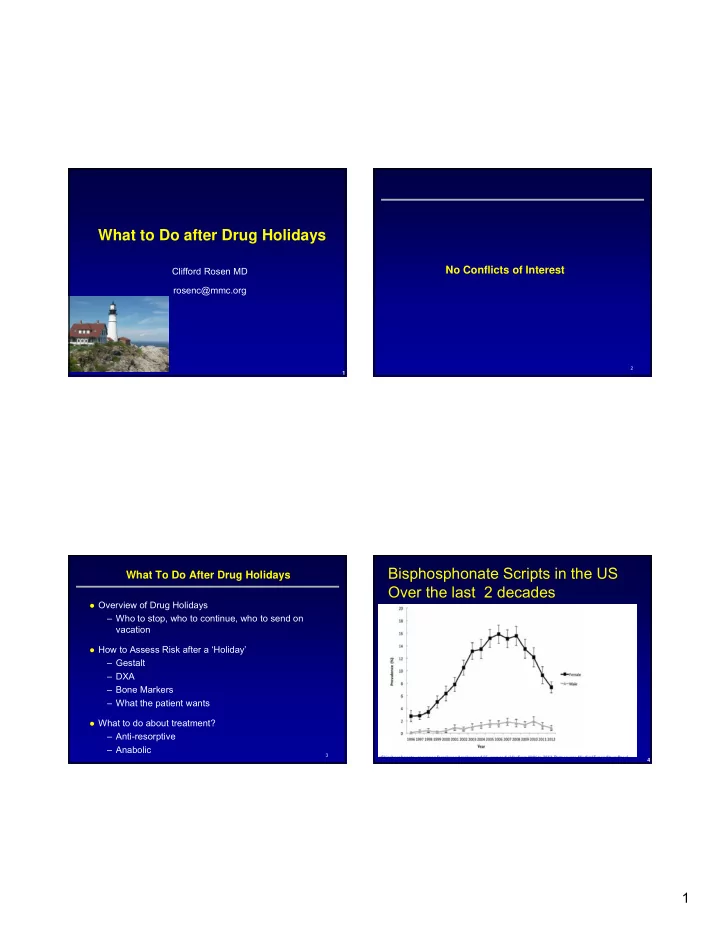
What to Do after Drug Holidays No Conflicts of Interest Clifford Rosen MD rosenc@mmc.org 2 1 Bisphosphonate Scripts in the US What To Do After Drug Holidays Over the last 2 decades Overview of Drug Holidays – Who to stop, who to continue, who to send on AFF first reports vacation How to Assess Risk after a ‘Holiday’ alendronate – Gestalt – DXA – Bone Markers – What the patient wants What to do about treatment? – Anti-resorptive – Anabolic 3 4 1
How Do Bisphosphonates Work? A drug holiday (sometimes also called a drug vacation, medication vacation, structured treatment interruption or strategic treatment interruption) is when a patient stops taking a medication(s) for a period of time; anywhere from a few days to many months or even years if they feel it is in their best interests. Wikipedia- 2016 5 6 Studies of Long Term Bisphosphonate Use (BMD primary endpoint) Study Drug Design N Follow-up Notes years FIT Long- Alendronate Randomized 1099 5+5=10 Term (5 & 10 , blinded trial Extension mg/day) (FLEX) HORIZON- Zoledronic Randomized 1233 3+3=6 PFT Ext. acid (5 blinded trial mg/year) Risedronate Risedronate Observation 164 3+3+3=9 Small, non- weekly al study randomized, adherent only 7 8 2
Design of the FIT Long-Term Extension Total Hip BMD: Mean % Change from FIT Baseline of Alendronate (FLEX)* FLEX Primary endpoint: Change in hip FIT N = 6,459 5 yrs FIT/FLEX Recess BMD 1 to 2 yrs FIT (3 to 4.5 yrs) FIT Mean Percent Change Start of FLEX 3 to 4.5 yrs Placebo N = 3,223 Alendronate N = 3,236 5 Post-FIT (1-2 yrs) 4 3 Randomized in FLEX 2 N = 1,099 FLEX (5 yrs) 2.8% 1 0 F 0 F 1 F 2 F 3 F 4 FL 0 FL 1 FL 2 FL 3 FL 4 FL 5 Alendronate, 5 mg Alendronate, 10 mg Year Placebo N = 437 N = 329 N = 333 FLEX FIT 40% 30% 30% = Placebo P <0.001 ALN vs PBO 9 10 = ALN (Pooled 5 mg and 10 mg groups) * Black, et al, JAMA 12/2006 Survival Curve for Time to First Nonvertebral Fracture in FLEX Fracture Incidence (Exploratory Endpoint) In FLEX ALN PBO Placebo 20 (N = 662) RR (95% CI) (N = 437) ALN (pooled) Cumulative Incidence, % Vertebral 15 0.45 (0.2, 0.8) Clinical 5% 2% 10 11.3% 9.8% 0.86 (0.6, 1.2) Morphometric RH=1.00 (0.76, 1.32) 5 Clinical Any 22% 21% 0.93 (0.7, 1.2) 0 0 1 2 3 4 5 Non-vertebral 20% 19% 1.00 (0.8, 1.4) Time to First Fracture, years Hip 3% 3% 1.02 (0.5, 2.3) F = FIT, FL = FLEX . 11 12 * Black, et al, JAMA 12/2006 Black DM et al. JAMA . 2006;296:1–12. 3
Fracture Results in HORIZON PFT Extension: 3 more HORIZON Extension Study Design years of ZOL Similar to FLEX extension Z6 Z3P3 RR (95% CI) (N = 616) (N = 617) 3 years of annual ZOL, then randomized to Vertebral either: 1.8 (0.5, 6.2) Clinical 0.7% 1.2% – 3 more years of ZOL (6 years, Z6) Morphometric 6% 3% 0.48 (0.3, 0.9) – 3 years of PBO (Z3P3) Non-vertebral Non-vertebral 7.6% 8.2% 0.99 (0.7, 1.5) Hip 1.4% 1.3% 0.90 (0.3, 2.5) 13 13 14 * Black, et al, JBMR 2012 Summary of Vertebral Fracture Reductions Efficacy from the 2 long-term randomized extension studies for FLEX and HORIZON Fracture results for both drugs – Continuing lowers vertebral fractures risk vs discontinuing – Continuing vs. discontinuing no effect on non-vertebral • Confidence intervals are wide and allow for possible benefit BMD results for both drugs (ALN and ZOL): – Continuing long term retains BMD gains Bisphosphonate benefit – Discontinuing BMD loses are modest What about long term safety? Does AFF risk increase with Relative Risk (Bis vs. PBO) longer duration of treatment? 15 16 4
Number 5 Yr risk (%) Femoral Neck BMD T- Needed to Clinical Vert. FLEX vertebral fracture Score (start FLEX) Treat Fx. In PBO benefit: Which patients benefit most from long term ALN All women in study (or ZOL) and should therefore be continued? All BMD values 5.5 34 Who to continue? Primary benefit is in reduction of vertebral fractures ≤ -2.5 9.3 21 -2.5 to -2 5.8 33 Therefore, logical to continue those at highest risk of ≥ -2 2.3 81 vertebral fractures No prevalent vert. fracture (start of FLEX ) – NEJM; 5/2012 ≤ -2.5 8.0 24 • Perspective from FDA together with an analysis from FLEX -2.5 to -2 3.0 63 – Consider femoral neck BMD and vertebral fracture status ≥ -2 1.8 102 at the end of the initial treatment period Prevalent vertebral fracture (start of FLEX) ≤ -2.5 11.1 17 -2.5 to -2 11.1 17 17 ≥ -2 3.7 51 17 18 Black, et al. NEJM 2012 May 31;366(22):2051-3 Black, et al. NEJM 2012 May 31;366(22):2051-3 Other clinical factors to assess to decide on discontinuation? Age (RR=1.5 per 6 years in FLEX) Fracture on initial phase of treatment (some support)* What to do after the ‘holiday’ Who to continue: Older patients with low hip BMD, and/or vertebral fractures and/or those who Or Re-entry Dilemma!!! fracture during initial treatment ASBMR committee Fall 2014: Likely to recommend to continue those with hip BMD < -2.5 or “high risk of fracture” 19 * Cosman et al. ASBMR 2012. 20 5
When to restart? - Discontinue for no more than 5 years - Perhaps BMD change after 3 to 5 year holiday (not 1 or 2 years) - No evidence to support bone marker assessment or change in bone marker 21 22 ROC Curves For Fracture Prediction with FRAX 23 24 6
One year after Discontinuation of BP Summary of Change in BMD 25 26 What To Re-Start or Maintain? BTMs one year after stopping Aln How About Calcium and Vitamin D After a Drug Holiday? 27 28 7
Updated Meta Analysis 2016 Calcium and Vitamin D Vitamin D and Calcium Reduces Fracture Risk (800IU+1200 mg/d) 2007 Tang Lancet 2007 USPSTF: No Risk Reduction for Vitamin D and Hip Fracture- 2014 29 30 Risk of Hip Fracture by Age Group in WHI: Age and Fall Interaction A Host of New Drug Treatments!!! 31 32 8
PTH once weekly Fracture Trial-56ug: 1-34 Nakumara, 2012 Summary • Drug holidays are a reality even though efficacy not clear • Should be considered in long term bisphosphonate users • Assess after the end of the holiday- – BMD, bone turnover markers, others • Restart Rx or add new drug still conjecture 9
On Shaky Ground? Very Little Evidence “First do no harm” 37 10
Recommend
More recommend