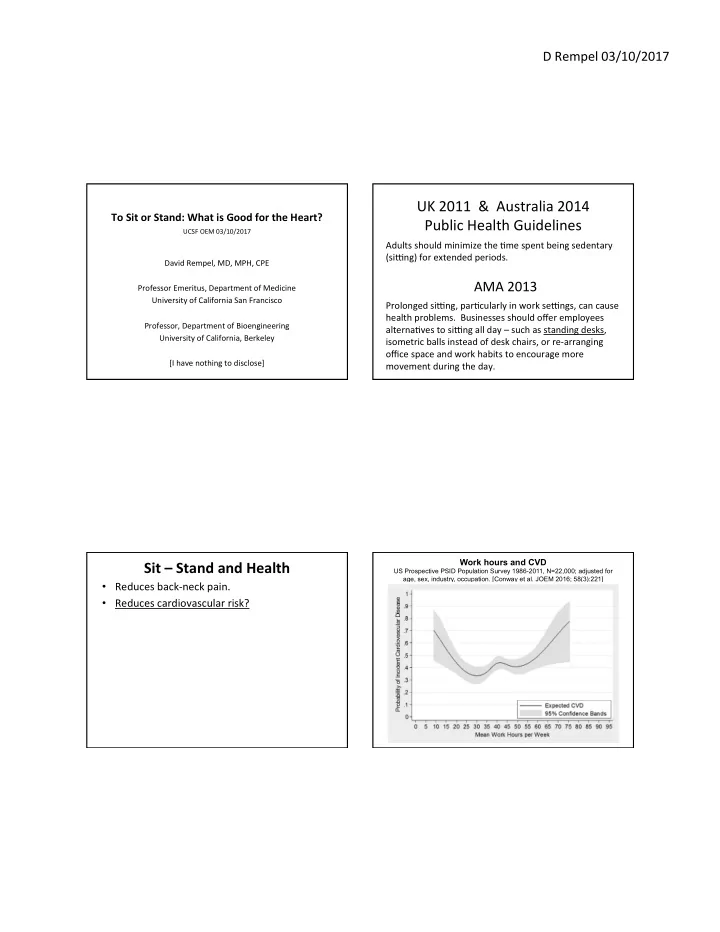
D Rempel 03/10/2017 UK 2011 & Australia 2014 To Sit or Stand: What is Good for the Heart? Public Health Guidelines UCSF OEM 03/10/2017 Adults should minimize the Sme spent being sedentary (siUng) for extended periods. David Rempel, MD, MPH, CPE AMA 2013 Professor Emeritus, Department of Medicine University of California San Francisco Prolonged siUng, parScularly in work seUngs, can cause health problems. Businesses should offer employees Professor, Department of Bioengineering alternaSves to siUng all day – such as standing desks, University of California, Berkeley isometric balls instead of desk chairs, or re-arranging office space and work habits to encourage more [I have nothing to disclose] movement during the day. Work hours and CVD Sit – Stand and Health US Prospective PSID Population Survey 1986-2011, N=22,000; adjusted for age, sex, industry, occupation. [Conway et al. JOEM 2016; 58(3):221] • Reduces back-neck pain. • Reduces cardiovascular risk?
D Rempel 03/10/2017 Predicted Weight Changes Do sit-stand worksta>ons reduce CVD risk? • Does occupaSonal siUng Sme increase CVD? • Does occupaSonal physical acSvity decrease CVD? • Does occupaSonal standing increase CVD? • Does sit-stand reduce BMI? • Does sit-stand reduce blood pressure? • [OccupaSonal standing increases leg volume, leg discomfort, and varicose veins] Church, Thomas, Tudor-Locke, et al. PLoS ONE, 2011 Daily Standing Time and All-Cause Mortality Words [Katzmarzyk 2009] • SiUng Sme • Standing Sme • Sedentary behavior • Physical inacSvity • No moderate-to-vigorous physical acSvity ‘‘For those acSviSes which you do most days of the week (such as work, school and housework), how much Sme do you spend standing?’’ 17,013 Canadians, ages 18-90, (41% of mortality = CVD), no adjustment for covariates
D Rempel 03/10/2017 Daily Standing Time and All-Cause Mortality Total SiUng Time & CVD (MI, CHD) [Katzmarzyk 2014] Study N Years Age HR Comparison Followed VanDerPloeg 2012 (Norway) 222,497 2.8 45-75 1.40 (1.27-1.55) >11 h/d Borodulin 2014 (Finland) 4,516 8.6 25-74 1.06 (1.01-1.11) h/d Petersen 2014 (Denmark) 71,363 5.4 18-99 1.59 (1.19-2.15) >10 h/d Maphews 2015 (USA) 154,614 6.8 59-82 1.42 (1.21-1.66) >12 h/d Chau 2015 ** (Norway) 50,817 3.3 20-75 1.65 (1.24-2.21) >10 h/d ** OccupaSonal siUng Sme did not increase risk Adjustment: sex, age, employment, educaSon, smoking, LTPA, BMI, diet, alcohol, serum cholesterol, hypertension Adjusted: age, smoking, alcohol, LTPA, physical acSvity readiness OccupaSonal SiUng Time & CVD (MI, CHD) London Bus Drivers Study Morris J et al., Lancet 1953. Study N Years Age HR Comparison Followed Stamatakis 2013 (UK) 10,834 12.9 >40 0.94 (0.67-1.33) v Stand-walk Drivers at increased risk for incident CHD Kikuchi 2015 (Japan) – Male* 15,863 10.0 40-74 0.87 (0.75-1.01) >3 h/d compared to conductors: 2.7 v 1.9/1000. Kikuchi 2015 (Japan) –Female* 12,005 10.2 40-74 1.03 (0.77-1.39) >3 h/d “Differences due to differences in physical Moller 2016 (Denmark) 154,840 12.2 21-70 0.99 (0.92-1.06) per 10 h/w acSvity” * Office workers Adjustment: sex, age, employment, educaSon, SES, smoking, LTPA, BMI, alcohol, serum cholesterol, hypertension, waist circumference, CVD at baseline
D Rempel 03/10/2017 Leisure Time Physical Ac>vity (LTPA) Reduces CVD London Bus Drivers Study Morris J et al., Lancet 1953. LTPA and CVD: Meta-analysis [Li et al., 2013] Drivers at increased risk for incident CHD • 23 prospecSve studies compared to conductors: 2.7/1000 vs 1.9. 790,000 adults • • 22,000 incidents “Differences due to differences in physical • Confounders controlled acSvity” • Moderate level LTPA reduced CVD risk 20-30% • High level LTPH No control for stress, BP, smoking, or BMI reduced CVD risk 30-40% Urban bus drivers have elevated BP. 5 Occupa>onal Physical Ac>vity (OPA) Does Not The OPA – LTPA Health Paradox [Li et al. Current Opinion in Cardiology. 28(5):575-583, 2013] • 7 prospecSve studies with adjustment for covariates • Moderate OPA increased risk 5-15% • SystemaSc Review (Li 2013) : OPA is bad & LTPA is good • High OPA increased risk 10-30% • Belgian cohort (Clays 2012) : OPA is bad & LTPA is only good for those with low OPA (OPA*LTPA InteracSon) • StaSc OPA increases BP & dynamic LTPA exercise reduces BP – a possible explanaSon for the paradox ? (Clays 2013) • Finnish cohort (Krause 2015) : OPA (energy expenditure, kcal) or relaSve aerobic workload (% VO 2 max) predict 20-year incidence of AMI. LTPA no effect.
D Rempel 03/10/2017 Does aerobic exercise at work Standing at Work Increases CVD increase fitness ? [Korshøj Met al., SJWEH 2014, EJAP 2015, IAOEH 2016, PLoS 2016] • YES, aerobic exercise (4 mo; 30 min x 2/wk) RCT among Danish cleaners: increased fitness & reduced HR & reduced C-reacSve protein and LDL. • BUT increased resSng and ambulatory SBP (5 mm HG), especially axer work (10 mmHG) among the workers who exceeded relaSve aerobic workload recommendaSons (30% VO2max). Standing compared to Smoking Standing Increases Caro>d Athersclerosis 4-year Change of Caro>d In>ma Media Thickness (IMT), adjusted for Age, Technical, Physical and Psychosocial Job Factors, Income, Biological and Behavioral Factors: Men with IHD Adjusted Mean Change in IMT (mm) 0.8 Adjusted Mean Change in IMT (mm) 0.75 0.8 0.74 0.7 0.7 0.6 0.6 0.5 Standing 0.5 Smoking 0.4 0.4 0.38 0.37 0.3 0.3 0.2 0.2 0.1 0.15 0.15 0.1 0.09 0.08 0 none little 0 quite a lot very much little/ low quite a lot/ very Standing at Work none/none T mid T much/ upper T Standing at Work / Smoking Krause et al., Scand J Work Environ Health, 2000 Krause et al., Scand J Work Environ Health, 2000
D Rempel 03/10/2017 NEPA: Non-exercise physical ac5vity Pictures of acSve workstaSons [Levine AJCN 2000] kcal/h SD Lying down 77 22 SiUng moSonless 80 23 Standing moSonless 87 24 SiWng & Fidge>ng 118 33 Standing & Fidge>ng 148 42 Walking (1.6 km/h) 196 62 Walking (3.2 km/h) 235 77 Walking (4.8 km/h) 305 113 NEPA: Non-exercise physical ac5vity Use of Sit-Stand WorkstaSons Tudor-Locke C et al, Int J Obesity 2014 • Sit-stand workstaSons lead to increased standing 50-70 minutes per day. Standing v SiUng Treadmill Walking v SiUng Seated Pedaling v SiUng 0 kcal/h (C: Speck 2011) 120 kcal/h 56 kcal/h 4 kcal/h (Beers 2008) 20 kcal/h (B: Reiff 2012)
D Rempel 03/10/2017 Does Work NEPA reduce Blood Pressure? SiUng and Lipid Profiles 8 week RCT [Graves et al, 2015] [Saidj 2013] Control (N=21) Sit-Stand Desk (N=23) • Danish working adults; N=2544; 18-69 yo SiUng 402 min/d Δ SiUng -87.6 min/d • Leisure Sme siUng (3.1h) assoc with increased TGs, Standing 44 min/d Δ Standing 72.9 min/d cholesterol, body fat, BMI, waist circumference. (no Walking 34 min/d Δ Walking 7.1 min/d assoc with Hgb A1c, Plasma glucose) Δ Glucose -0.09 mmol/L Δ Triglycerides 0.11 mmol/L • OccupaSonal Sme siUng (4.1h) no associaSons Δ Cholersterol -0.40 mmol/L Δ SBP -1.6 mmHg • Adjusted: sex, age, ed, smoking, alcohol, diet, PA Δ DBP -2.5 mmHg [All differences NS] Predicted Weight Changes Does Work NEPA reduce Blood Pressure? 4 month RCT [Mainsbridge, JOEM 2014] • Every hour soxware prompt to stand up and move • NEPA of 8 minutes/day reduced resSng mean arterial pressure (MAP) by 10 mmHg axer 4 months. • Strength: RCT • Limita5ons: - small samples (N=11+18) - randomizaSon not successful (controls 5.5 years older) - no blinding - no age-adjustment - no between group-effects analyzed, only pre-post Church, Thomas, Tudor-Locke, et al. PLoS ONE, 2011
D Rempel 03/10/2017 Increasing OccupaSonal SiUng Causing Obesity Epidemic? Increasing OccupaSonal SiUng Causing Obesity Epidemic? Church, Thomas, Tudor-Locke, et al. PLoS ONE, 2011 Trends in sedentary, light and moderate intensity occupaSons Church, Thomas, Tudor-Locke, et al. PLoS ONE, 2011 Increasing OccupaSonal SiUng Causing Obesity Epidemic? US Caloric ConsumpSon per Day Daily OccupaSonal Energy Expenditure Church, Thomas, Tudor-Locke, et al. PLoS ONE, 2011 +900 daily kcals -140 daily kcals -120 daily kcals USDA, NHANES
D Rempel 03/10/2017 Conclusions 1. Typically, with reminder soxware, for how many minutes per day are sit-stand workstaSons used for standing? • All Sme siUng increases CVD • OccupaSonal siUng does not increases CVD • Standing at work increases CVD A. 0 to 40 minutes • OccupaSonal physical acSvity does not decrease CVD • No evidence that sit-stand workstaSons decrease CVD B. 40 to 80 minutes • Metabolism é w standing inadequate to decrease BMI • Standing NEPA effects on BP uncertain C. 80 to 120 minutes • Sit-stand workstaSons may be beneficial for LBP D. 120 to 160 minutes 2. Standing, as compared to siUng, 3. Treadmill desks are welcome in open increases caloric consumpSon by office seUngs because A. 0 to 20 kcal/h (a packet of sugar) A. They are quiet B. 20 to 40 kcal/h (a plum) B. They are safe C. They increase metabolism C. 40 to 60 kcal/h (1 tofu dog) D. It is easy to see who is using them D. 60 to 80 kcal/h (a very very light beer)
Recommend
More recommend